Abstract
Purpose
Rupture of the contralateral Achilles tendon following Achilles tendon rupture can lead to devastating outcomes. However, despite the clinical importance, the risk factors and incidence of contralateral Achilles tendon rupture have not been well studied. This study aimed to determine the incidence of contralateral tendon rupture after Achilles tendon rupture and to identify associated patient characteristics.
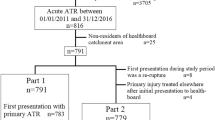
Methods
Medical records for 226 consecutive patients with Achilles tendon rupture were retrospectively reviewed. The occurrence of contralateral Achilles tendon rupture and patient characteristics were determined through review of medical records and telephone surveys.
Results
The cumulative incidences of contralateral Achilles tendon rupture at 1, 3, 5, and 7 years after Achilles tendon rupture were 0.4%, 1.8%, 3.4%, and 5.1%, respectively. The only statistically significant risk factor was age between 30 and 39 years at the time of initial Achilles tendon rupture (hazard ratio = 4.9).
Conclusions
Patients who sustain Achilles tendon rupture in their 30 s have significantly increased risk for contralateral tendon rupture.
Level of evidence
III.


Similar content being viewed by others
References
Aröen A, Helgo D, Granlund OG, Bahr R (2004) Contralateral tendon rupture risk is increased in individuals with a previous Achilles tendon rupture. Scand J Med Sci Sports 14:30–33
El Khoury L, Ribbans WJ, Raleigh SM (2016) MMP3 and TIMP2 gene variants as predisposing factors for Achilles tendon pathologies: attempted replication study in a British case-control cohort. Meta Gene 9:52–55
Ganestam A, Kallemose T, Troelsen A, Barfod KW (2016) Increasing incidence of acute Achilles tendon rupture and a noticeable decline in surgical treatment from 1994 to 2013. A nationwide registry study of 33,160 patients. Knee Surg Sports Traumatol Arthrosc 24:3730–3737
Gwynne-Jones DP, Sims M, Handcock D (2011) Epidemiology and outcomes of acute Achilles tendon rupture with operative or nonoperative treatment using an identical functional bracing protocol. Foot Ankle Int 32:337–343
Halasi T, Kynsburg A, Tallay A, Berkes I (2004) Development of a new activity score for the evaluation of ankle instability. Am J Sports Med 32:899–908
Houshian S, Tscherning T, Riegels-Nielsen P (1998) The epidemiology of Achilles tendon rupture in a Danish county. Injury 29:651–654
Kannus P, Jozsa L (1991) Histopathological changes preceding spontaneous rupture of a tendon. A controlled study of 891 patients. J Bone Joint Surg Am 73:1507–1525
Khan RJ, Fick D, Keogh A, Crawford J, Brammar T, Parker M (2005) Treatment of acute achilles tendon ruptures. A meta-analysis of randomized, controlled trials. J Bone Jt Surg Am 87:2202–2210
Kim SK, Roos TR, Roos AK, Kleimeyer JP, Ahmed MA, Goodlin GT, Fredericson M, Ioannidis JP, Avins AL, Dragoo JL (2017) Genome-wide association screens for Achilles tendon and ACL tears and tendinopathy. PLoS One 12:e0170422
Maffulli N, Ewen SW, Waterston SW, Reaper J, Barrass V (2000) Tenocytes from ruptured and tendinopathic achilles tendons produce greater quantities of type III collagen than tenocytes from normal achilles tendons. An in vitro model of human tendon healing. Am J Sports Med 28:499–505
Maffulli N, Waterston SW, Squair J, Reaper J, Douglas AS (1999) Changing incidence of Achilles tendon rupture in Scotland: a 15-year study. Clin J Sport Med 9:157–160
Moller A, Astron M, Westlin N (1996) Increasing incidence of Achilles tendon rupture. Acta Orthop Scand 67:479–481
Nilsson-Helander K, Silbernagel KG, Thomee R, Faxen E, Olsson N, Eriksson BI, Karlsson J (2010) Acute achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med 38:2186–2193
Nyyssonen T, Luthje P, Kroger H (2008) The increasing incidence and difference in sex distribution of Achilles tendon rupture in Finland in 1987–1999. Scand J Surg 97:272–275
Park YH, Jeong SM, Choi GW, Kim HJ (2017) How early must an acute Achilles tendon rupture be repaired? Injury 48:776–780
Raikin SM, Garras DN, Krapchev PV (2013) Achilles tendon injuries in a United States population. Foot Ankle Int 34:475–480
Reito A, Logren HL, Ahonen K, Nurmi H, Paloneva J (2018) Risk factors for failed nonoperative treatment and rerupture in acute achilles tendon rupture. Foot Ankle Int. https://doi.org/10.1177/10711007177540421071100717754042
Rettig AC, Liotta FJ, Klootwyk TE, Porter DA, Mieling P (2005) Potential risk of rerupture in primary achilles tendon repair in athletes younger than 30 years of age. Am J Sports Med 33:119–123
Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K (2005) Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy 21:948–957
Webster KE, Feller JA, Leigh WB, Richmond AK (2014) Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med 42:641–647
Willits K, Amendola A, Bryant D, Mohtadi NG, Giffin JR, Fowler P, Kean CO, Kirkley A (2010) Operative versus nonoperative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation. J Bone Jt Surg Am 92:2767–2775
Yasui Y, Tonogai I, Rosenbaum AJ, Shimozono Y, Kawano H, Kennedy JG (2017) The risk of achilles tendon rupture in the patients with achilles tendinopathy: healthcare database analysis in the United States. Biomed Res Int 2017:7021862
Young SW, Patel A, Zhu M, van Dijck S, McNair P, Bevan WP, Tomlinson M (2014) Weight-bearing in the nonoperative treatment of acute achilles tendon ruptures: a randomized controlled trial. J Bone Jt Surg Am 96:1073–1079
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
YHP: lead investigator and first author. TJK: data analysis and manuscript review. GWC: data analysis and manuscript review. HJK: corresponding author, primary surgeon. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the contents of this study.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Institutional review board approval was obtained, and the requirement for informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Park, Y.H., Kim, T.J., Choi, G.W. et al. Age is a risk factor for contralateral tendon rupture in patients with acute Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc 28, 1625–1630 (2020). https://doi.org/10.1007/s00167-019-05380-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05380-y