Abstract
Purpose
One of the causes of aseptic loosening is marked tibial bone resorption (TR) at the tibial bone–component interface after total knee arthroplasty (TKA). It was hypothesized that insufficient coverage of the tibial component and improper cementing technique would cause increased TR after cemented TKA.
Methods
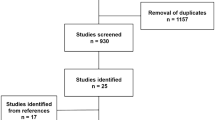
One hundred thirty-four primary TKAs in 107 patients with varus osteoarthritis were included in this study. The relationships between the TRs at 2 years after TKA and the tibial component underhang (TUH), the thickness of the cement mantle around the keel, and clinical parameters were evaluated.
Results
The widths of TRs on anteroposterior radiographs were significantly larger on the medial side than on the lateral side (p = 0.001), whereas the difference between the anterior and posterior sides on lateral radiographs was relatively small. Multiple regression analyses showed that medial TR was positively related to medial TUH (p = 0.006), and lateral TR was positively related to a thicker distal cement mantle (p = 0.027). On the lateral view, stepwise selection indicated that postoperative knee flexion angle was the most significant risk factor (p = 0.005) for anterior TR, and posterior TUH was the strongest predictor (p = 0.001) of posterior TR.
Conclusions
To avert postoperative progressive TR, surgeons should perfectly fit a suitably sized tibial component to the medial edge of the tibia. Also, care should be taken to avoid an excessive cement mantle at the distal portion of the keel during TKA.
Level of evidence
IV.


Similar content being viewed by others
References
Abdel MP, Bonadurer GF 3rd, Jennings MT, Hanssen AD (2015) Increased aseptic tibial failures in patients with a BMI ≥ 35 and well-aligned total knee arthroplasties. J Arthroplast 30:2181–2184
Al-Nabhani K, Michopoulou S, Allie R, Alkalbani J, Saad Z, Sajjan R et al (2014) Painful knee prosthesis: can we help with bone SPECT/CT? Nucl Med Commun 35:182–188
Awengen R, Rasch H, Amsler F, Hirschmann MT (2016) Symptomatic versus asymptomatic knees after bilateral total knee arthroplasty: what is the difference in SPECT/CT? Eur J Nucl Med Mol Imaging 43:762–772
Berend ME, Ritter MA, Hyldahl HC, Meding JB, Redelman R (2008) Implant migration and failure in total knee arthroplasty is related to body mass index and tibial component size. J Arthroplast 23:104–109
Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R et al (2004) Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res 428:26–34
Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP et al (2010) The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res 468:45–51
Cawley DT, Kelly N, McGarry JP, Shannon FJ (2013) Cementing techniques for the tibial component in primary total knee replacement. Bone Joint J 95:295–300
Cerquiglini A, Henckel J, Hothi H, Rotigliano N, Hirschmann MT, Hart AJ (2018) 3D patient imaging and retrieval analysis help understand the clinical importance of rotation in knee replacements. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-4891-9
Chau R, Gulati A, Pandit H, Beard DJ, Price AJ, Dodd CAF et al (2009) Tibial component overhang following unicompartmental knee replacement—Does. it matter? Knee 16:310–313
Clary C, Aram L, Deffenbaugh D, Heldreth M (2014) Tibial base design and patient morphology affecting tibial coverage and rotational alignment after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:3012–3018
Completo A, Fonseca F, Simões JA (2008) Strain shielding in proximal tibia of stemmed knee prosthesis: experimental study. J Biomech 41:560–566
Completo A, Simões JA, Fonseca F, Oliveira M (2008) The influence of different tibial stem designs in load sharing and stability at the cement-bone interface in revision TKA. Knee 15:227–232
Fukagawa S, Matsuda S, Mitsuyasu H, Miura H, Okazaki K, Tashiro Y et al (2011) Anterior border of the tibia as a landmark for extramedullary alignment guide in total knee arthroplasty for varus knees. J Orthop Res 29:919–924
Guha AR, Debnath UK, Graham NM (2008) Radiolucent lines below the tibial component of a total knee replacement (TKR)—a comparison between single-and two-stage cementation techniques. Int Orthop 32:453–457
Hazelwood KJ, O’Rourke M, Stamos VP, McMillan RD, Beigler D, Robb WJ (2015) Case series report: early cement-implant interface fixation failure in total knee replacement. Knee 22:424–428
Hirschmann MT, Amsler F, Rasch H (2015) Clinical value of SPECT/CT in the painful total knee arthroplasty (TKA): a prospective study in a consecutive series of 100 TKA. Eur J Nucl Med Mol Imaging 42:1869–1882
Jazrawi LM, Bai B, Kummer FJ, Hiebert R, Stuchin SA (2001) The effect of stem modularity and mode of fixation on tibial component stability in revision total knee arthroplasty. J Arthroplasty 16:759–767
Kuriyama S, Hyakuna K, Inoue S, Kawai Y, Tamaki Y, Ito H et al (2018) Bone-femoral component interface gap after sagittal mechanical axis alignment is filled with new bone after cementless total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26:1478–1484
Kuriyama S, Hyakuna K, Inoue S, Tamaki Y, Ito H, Matsuda S (2014) Tibial rotational alignment was significantly improved by use of a CT-navigated control device in total knee arthroplasty. J Arthroplast 29:2352–2356
Kuriyama S, Ishikawa M, Furu M, Ito H, Matsuda S (2014) Malrotated tibial component increases medial collateral ligament tension in total knee arthroplasty. J Orthop Res 32:1658–1666
Kuriyama S, Ishikawa M, Nakamura S, Furu M, Ito H, Matsuda S (2017) Noise generation with good range of motion but without femorotibial instability has small effect on patient satisfaction after total knee arthroplasty. J Arthroplast 32:407–412
Lim HA, Song EK, Seon JK, Park KS, Shin YJ, Yang HY (2017) Causes of aseptic persistent pain after total knee arthroplasty. Clin Orthop Surg 9:50–56
Martin JR, Watts CD, Levy DL, Kim RH (2017) Medial tibial stress shielding: a limitation of cobalt chromium tibial baseplates. J Arthroplast 32:558–562
Martin JR, Watts CD, Levy DL, Miner TM, Springer BD, Kim RH (2017) Tibial tray thickness significantly increases medial tibial bone resorption in cobalt–chromium total knee arthroplasty implants. J Arthroplast 32:79–82
Martin S, Saurez A, Ismaily S, Ashfaq K, Noble P, Incavo SJ (2014) Maximizing tibial coverage is detrimental to proper rotational alignment. Clin Orthop Relat Res 472:121–125
Meneghini RM, Mont MA, Backstein DB, Bourne RB, Dennis DA, Scuderi GR (2015) Development of a modern knee society radiographic evaluation system and methodology for total knee arthroplasty. J Arthroplast 30:2311–2314
Nakamura S, Ito H, Nakamura K, Kuriyama S, Furu M, Matsuda S (2017) Long-term durability of ceramic tri-condylar knee implants: a minimum 15-year follow-up. J Arthroplast 32:1874–1879
Nakamura S, Kobayashi M, Ito H, Nakamura K, Ueo T, Nakamura T (2010) The bi-surface total knee arthroplasty: minimum 10-year follow-up study. Knee 17:274–278
Pfitzner T, von Roth P, Voerkelius N, Mayr H, Perka C, Hube R (2016) Influence of the tourniquet on tibial cement mantle thickness in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24:96–101
Pijls BG, Valstar ER, Nouta K-A, Plevier JW, Fiocco M, Middeldorp S et al (2012) Early migration of tibial components is associated with late revision: a systematic review and meta-analysis of 21,000 knee arthroplasties. Acta Orthop 83:614–624
Ritter MA, Keating EM, Sueyoshi T, Davis KE, Barrington JW, Emerson RH (2016) Twenty-five-years and greater, results after nonmodular cemented total knee arthroplasty. J Arthroplast 31:2199–2202
Scott CE, Biant LC (2012) The role of the design of tibial components and stems in knee replacement. J Bone Joint Surg Br 94:1009–1015
Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J (2014) Why are total knee arthroplasties failing today—Has anything changed after 10 years? J Arthroplast 29:1774–1778
Simsek ME, Akkaya M, Gursoy S, Isik C, Zahar A, Tarabichi S et al (2018) Posterolateral overhang affects patient quality of life after total knee arthroplasty. Arch Orthop Trauma Surg 138:409–418
Staats K, Wannmacher T, Weihs V, Koller U, Kubista B, Windhager R (2018) Modern cemented total knee arthroplasty design shows a higher incidence of radiolucent lines compared to its predecessor. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5130-0
Sundfeldt M, Carlsson LV, Johansson CB, Thomsen P, Gretzer C (2006) Aseptic loosening, not only a question of wear: a review of different theories. Acta Orthop 77:177–197
Thiele K, Perka C, Matziolis G, Mayr HO, Sostheim M, Hube R (2015) Current failure mechanisms after knee arthroplasty have changed: Polyethylene wear is less common in revision surgery. J Bone Joint Surg Am 97:715–720
van de Groes, de Waal-Malefijt, V (2014) Probability of mechanical loosening of the femoral component in high flexion total knee arthroplasty can be reduced by rather simple surgical techniques. Knee 21:209–215
Vanlommel J, Luyckx JP, Labey L, Innocenti B, De Corte R, Bellemans J (2011) Cementing the tibial component in total knee arthroplasty: which technique is the best? J Arthroplasty 26:492–496
Wang H, Lou H, Zhang H, Jiang J, Liu K (2014) Similar survival between uncemented and cemented fixation prostheses in total knee arthroplasty: a meta-analysis and systematic comparative analysis using registers. Knee Surg Sports Traumatol Arthrosc 22:3191–3197
Zelle J, Janssen D, Van Eijden J, De Waal Malefijt M, Verdonschot N (2011) Does high-flexion total knee arthroplasty promote early loosening of the femoral component? J Orthop Res 29:976–983
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest in association with the present study.
Ethical approval
All procedures were in accordance with the ethical standards of our institutional research committee.
Informed consent
Informed consent was obtained from all study participants.
Rights and permissions
About this article
Cite this article
Gu, S., Kuriyama, S., Nakamura, S. et al. Underhang of the tibial component increases tibial bone resorption after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 27, 1270–1279 (2019). https://doi.org/10.1007/s00167-018-5309-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5309-4