Abstract
Purpose
The Ligament Augmentation and Reconstruction System (LARS®) has been at the forefront of a recent revival in the use of synthetic ligaments for ACL reconstruction. However, despite promising short-to-mid-term results its role has been approached with caution due to a high number of major complications in previous synthetic graft designs including mechanical failures, synovitis and osteoarthritis. This study aims to report on the incidence of synovitis in a series of patients undergoing second-look surgery following LARS ACL reconstruction.
Methods
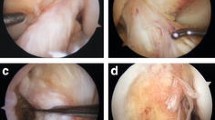
A retrospective analysis was performed of a single surgeon’s series of 12 patients that underwent second-look arthroscopic surgery following primary LARS ACL surgery for indications including mechanical symptoms (meniscal tears/cyclops lesions/chondral flaps) and/or symptomatic instability secondary to LARS failure. In all cases an examination under anaesthesia (EUA) was performed, and a qualitative assessment of the synovium was carried out and graded as normal, reactive or inflammatory. A synovial biopsy was performed in all knees with visible evidence of synovitis and in all cases of LARS failure.
Results
The second-look arthroscopy was performed at a mean of 23 months (7–66) after the index surgery. In 6 (50%) knees the LARS device had failed necessitating removal and revision ACL reconstruction, while in the remaining 6 knees the LARS was still intact. Arthroscopic evaluation of the synovium revealed a normal appearance in 8 knees (67%) and reactive synovitis in 4 knees (23%); of these 4 knees, one had an intact LARS device and 3 had failed LARS. Histological examination from these 4 knees and the 3 knees with graft failures without visible synovitis revealed chronic hypertrophic synovitis (moderate 2, mild 5) in all cases with rare giant cells, consistent with a reaction to foreign body material.
Conclusions
Foreign body synovitis is a common finding in our series of patients undergoing a repeat arthroscopy following a LARS ACL reconstruction. The histological diagnosis of synovitis was more frequently encountered than an arthroscopic appearance of synovitis. Whilst the results of this case series cannot support a direct causative link between LARS failure and the development of synovitis, this study highlights the need to remain vigilant about the risk of reactive synovitis following LARS ACL reconstruction due to exposure of the knee to foreign body material.
Level of evidence
Level IV, case series.


Similar content being viewed by others
References
Adachi N, Ochi M, Uchio Y, Sakai Y, Kuriwaka M, Fujihara A (2003) Harvesting hamstring tendons for ACL reconstruction influences post operative hamstring muscle performance. Arch Orthop Trauma Surg; 123:460–465
Ayral X, Mayoux-Benhamou A, Dougados M (1996) Proposed scoring system for assessing synovial membrane abnormalities at arthroscopy in knee osteoarthritis. Br J Rheumatol 35(Suppl 3):14–17
Batty L, Norsworthy C, Lash N, Wasiak J, Richmond A, Feller J (2015) Synthetic devices for reconstructive surgery of the cruciate ligaments: a systematic review. Arthroscopy 31(5):957–968
Barrera O, Sikka R, Wolters B, Graver R, Boyd JL, Nelson B, Swiontkowski M (2011) Autograft versus allograft: an economic cost comparison of anterior cruciate ligament reconstruction. Arthroscopy 27(9):1219–1225
Dericks G (1995) Ligament advanced reinforcement system anterior cruciate ligament reconstruction. Oper Tech Sports Med 3(3):187–205
Gao K, Chen S, Wang L et al (2010) Anterior cruciate ligament reconstruction with LARS artificial ligament: a multicenter study with 3- to 5-year follow-up. Arthroscopy 26(4):515–523
Glezos C, Waller A, Bourke H, Salmon L, Pinczewski L (2012) Disabling synovitis associated with LARS artificial ligament use in anterior cruciate ligament reconstruction. Am J Sports Med 40(5):1167–1171
Huang J-M, Wang Q, Shen F, Wang Z-M, Kang Y-F (2010) Cruciate ligament reconstruction using LARS artificial ligament under arthroscopy: 81 cases report. Chin Med J 123(2):160
Iliadis DP, Bourlos DN, Mastrokalos DS, Chronopoulos E, Babis GC (2016) LARS artificial ligament versus ABC purely polyester ligament for anterior cruciate ligament reconstruction. Orthop J Sports Med. https://doi.org/10.1177/2325967116653359
Janssen R, Scheffler S (2014) Intra-articular remodelling of hamstring tendon grafts after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 22(9):2102–2108
Johnson D, Waterman (2015) B. Synthetic Grafts—Where Is the Common Sense? Arthroscopy 31(10):1849–1850
Kartus J, Movin T, Karlsson J (2001) Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy 17(9):971–980
Klein W, Jensen K-U (1992) Synovitis and artificial ligaments. Arthroscopy 8(1):116–124
Li H, Yao Z, Jiang J, Hua Y, Chen J, Li Y, Gao K, Chen S (2012) Biologic failure of a ligament advancement reinforcement system artificial ligament in anterior cruciate ligament reconstruction: a report of serious knee synovitis. Arthroscopy 28(4):583–586
Liu Z-T, Zhang X-L, Jiang Y, Zeng B-F (2010) Four-strand hamstring tendon autograft versus LARS artificial ligament for anterior cruciate ligament reconstruction. Int Orthop 34(1):45–49
Machotka Z, Scarborough I, Duncan W, Kumar S, Perraton L (2010) Anterior cruciate ligament repair with LARS (ligament advanced reinforcement system): a systematic review. Sports Med Arthrosc Rehabil Ther Technol 2:29
Maletius W, Gillquist J (1997) Long-term results of anterior cruciate ligament reconstruction with a dacron prosthesis: the frequency of osteoarthritis after seven to eleven years. Am J Sports Med 25(3):288–293
Manunta AF, Zedde P, Pisanu F, Marras F (2015) Sports-related changes of the synovial membrane. Joints Feb 13 2(4):181–187
Mascarenhas R, MacDonald PB (2008) Anterior cruciate ligament reconstruction: a look at prosthetics–past, present and possible future. Mcgill J Med 11(1):29–37
Murray AW, Macnicol MF (2004) 10–16 year results of Leeds-Keio anterior cruciate ligament reconstruction. Knee 11(1):9–14
Nau T, Lavoie P, Duval N (2002) A new generation of artificial ligaments in reconstruction of the anterior cruciate ligament: two-year follow-up of a randomised trial. J Bone Joint Surg Br 84(3):356–360
Pan X, Wen H, Wang L, Ge T (2013) Bone-patellar tendon-bone autograft versus LARS artificial ligament for anterior cruciate ligament reconstruction. Eur J Orthop Surg Traumatol 23(7):819–823
Parchi P, Gianluca C, Dolfi L et al (2013) Anterior cruciate ligament reconstruction with LARS™ artificial ligament results at a mean follow-up of eight years. Int Orthop 37(8):1567–1574
Shaffer B, Gow W, Tibone JE (1993) Graft-tunnel mismatch in endoscopic anterior cruciate ligament reconstruction: a new technique of intraarticular measurement and modified graft harvesting. Arthroscopy 9:633–646
Struewer J, Ziring E, Ishaque B, Efe T, Schwarting T, Buecking B, Schüttler KF, Ruchholtz S, Frangen TM (2013) Second-look arthroscopic findings and clinical results after polyethylene terephthalate augmented anterior cruciate ligament reconstruction. Int Orthop 37(2):327–335
Tiefenboeck T, Thurmaier E, Tiefenboeck M et al (2015) Clinical and functional outcome after anterior cruciate ligament reconstruction using the LARS™ system at a minimum follow-up of 10 years. The Knee; (22): 565–568
Ventura A, Terzaghi C, Legnani C, Borgo E, Albisetti W (2010) Synthetic grafts for anterior cruciate ligament rupture: 19-year outcome study. Knee 17:108–113
Ye JX, Shen GS, Zhou HB et al (2013) Arthroscopic reconstruction of the anterior cruciate ligament with the LARS artificial ligament: thirty-six to fifty-two months follow-up study. Eur Rev Med Pharmacol Sci 17(11):1438–1446
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to declare for any authors.
Ethical approval
Ethics approval for the study was provided by the Epworth Health Care Human Research and Ethics Sub-Committee—ID # LR123-13.
Informed consent
Informed consent was obtained from all individual participants in the study.
Rights and permissions
About this article
Cite this article
Tulloch, S.J., Devitt, B.M., Norsworthy, C.J. et al. Synovitis following anterior cruciate ligament reconstruction using the LARS device. Knee Surg Sports Traumatol Arthrosc 27, 2592–2598 (2019). https://doi.org/10.1007/s00167-018-5280-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5280-0