Abstract
Purpose
Patient-specific instrumentation (PSI) is a technique to plan and position the prosthesis components in unicompartmental knee arthroplasty (UKA) surgery. This study assesses whether the definitive component position in the frontal, sagittal and axial plane is according to the preoperative plan, based on the hypothesis that PSI is accurate.
Methods
Twenty-six patients who had PSI Oxford UKA surgery were included prospectively. The component position in vivo was determined with a postoperative CT-scan and compared with the planned component position using MRI-based digital 3D imaging. Adjustments to the preoperative plan and implanted component sizes during surgery were recorded.
Results
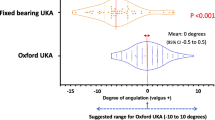
Intraoperatively, no femoral adjustments were performed; 12 tibial re-resections were necessary. The median absolute deviation from the plan in degrees (range) in the frontal, sagittal and axial plane was 1.8° (− 1.5°–6.5°), 2.0° (− 6.5°–8.0°) and 1.0° (− 1.5°–5.0°) for the femoral component, and 2.5° (− 1.0°–6.0°), 3.0° (− 1.0°–5.0°) and 5.0° (− 6.5°–12.5°) for the tibial component. The femoral component is positioned 0.5 (− 1°–2.5°) mm more lateral and 0.8 (− 1.0°–2.5°) mm more anterior. The tibial component is positioned 2.0 (− 5.0–0.0) mm more lateral and 1.3 (− 3.0–6.0) mm more distal. The femoral and tibial default plans were changed four times (15.4%) and nine times (34.6%), respectively, before approval by the surgeon.
Conclusion
PSI in Oxford UKA surgery is reliable and accurately translates the preoperative plan into the in vivo situation, except for the tibial rotational position. The preoperative planning is a crucial step in avoiding re-resections that can cause angular deviations in prosthesis position, especially in tibial component rotational position. It is advised to avoid re-resections and to consider this while planning the PSI procedure.
Level of evidence
Prospective comparative study Level II.


Similar content being viewed by others
References
Boonen B, Schotanus MG, Kerens B, Hulsmans FJ, Tuinebreijer WE, Kort NP (2015) Patient-specific positioning guides for total knee arthroplasty: no significant difference between final component alignment and pre-operative digital plan except for tibial rotation. Knee Surg Sports Traumatol Arthrosc 25(9):2809–2817
Goodfellow J, O’Connor J, Dodd C, Murray D (2006) Unicompartmental arthroplasty with the Oxford Knee. Oxford University Press, Oxford, p 190
Hamilton WG, Parks NL, Saxena A (2011) Patient-specific instrumentation does not shorten surgical time: a prospective, randomized trial. J Arthroplasty 28:96–100
Hirschmann MT, Konala P, Amsler F, Iranpour F, Friederich NF, Cobb JP (2011) The position and orientation of total knee replacement components: a comparison of conventional radiographs, transverse 2D-CT slices and 3D-CT reconstruction. J B Jt Surg Br 93:629–633
Hooper N, Snell D, Hooper G, Maxwell R, Frampton C (2015) The 5-year radiological results of the uncemented Oxford medial compartment knee arthroplasty. B Jt J 97–B:1358–1363
Iriberri I, Aragón JF (2014) Alignment of the tibial component of the unicompartmental knee arthroplasty, assessed in the axial view by CT-scan: does it influence the outcome? Knee 21(6):1269–1274
Jenny JY, Boeri C (2003) Unicompartmental knee prosthesis implantation with a non-image-based navigation system: rationale, technique, case-control comparative study with a conventional instrumented implantation. Knee Surg Sports Traumatol Arthrosc 11:40–45
Jonkergouw F, Allé F, Chellaoui K, Vander Sloten J, Vangeneugden D (2016) Three-dimensional measurement technique to assess implant position and orientation after total knee arthroplasty. Med Eng Phys 38(12):1513–1517
Jung KA, Kim SJ, Lee SC, Hwang SH, Ahn NK (2010) Accuracy of implantation during computer-assisted minimally invasive Oxford unicompartmental knee arthroplasty: a comparison with a conventional instrumented technique. Knee 17:387–391
Kendrick BJ, Kaptein BL, Valstar ER, Gill HS, Jackson WF, Dodd CA, Price AJ, Murray DW (2015) Cemented versus cementless Oxford unicompartmental knee arthroplasty using radiostereometric analysis: a randomised controlled trial. B Jt J 97–B:185–191
Kerens B, Schotanus MG, Boonen B, Kort NP (2015) No radiographic difference between patient-specific guiding and conventional Oxford UKA surgery. Knee Surg Sports Traumatol Arthrosc 23:1324–1329
Liow MH, Tsai TY, Dimitriou D, Li G, Kwon YM (2016) Does 3-dimensional in vivo component rotation affect clinical outcomes in unicompartmental knee arthroplasty? J Arthroplasty 31(10):2167–2172
Lisowski LA, van den Bekerom MP, Pilot P, van Dijk CN, Lisowski AE (2010) Oxford phase 3 unicompartmental knee arthroplasty: medium-term results of a minimally invasive surgical procedure. Knee Surg Sports Traumatol Arthrosc 19:277–284
Pandit H, Hamilton TW, Jenkins C, Mellon SJ, Dodd CA, Murray DW (2015) The clinical outcome of minimally invasive phase 3 Oxford unicompartmental knee arthroplasty: a 15-year follow-up of 1000 UKAs. B Jt J 97–B:1493–1500
Renson L, Poilvache P, Van den Wyngaert H (2014) Improved alignment and operating room efficiency with patient-specific instrumentation for TKA. Knee 21:1216–1220
Schotanus MGM, Schoenmakers DAL, Sollie R, Kort NP (2015) Patient-specific instruments for total knee 247 arthroplasty can accurately predict the component size as used peroperative. Knee Surg Sports Traumatol Artrosc. https://doi.org/10.1007/s0016701643451
Schotanus MGM, Thijs E, Boonen B et al (2017) Revision of partial knee to total knee arthroplasty with use of patient-specific instruments results in acceptable femoral rotation. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-017-4674-8
Servien E, Fary C, Lustig S et al (2011) Tibial component rotation assessment using CT-scan in medial and lateral unicompartmental knee arthroplasty. Orthop Traumatol Surg Res 97(3):272–275
Trong MLD, Diezi C, Goerres G, Helmy N (2015) Improved positioning of the tibial component in unicompartmental knee arthroplasty with patient-specific cutting blocks. Knee Surg Sports Traumatol Artrosc 23:1993–1998
Tsai TY, Dimitriou D, Liow MH, Rubash HE, Li G, Kwon YM (2016) Three-dimensional imaging analysis of unicompartmental knee arthroplasty evaluated in standing position: component alignment and in vivo articular. Contact J Arthroplasty 31(5):1096–1101
van Leeuwen JA, Röhrl SM (2016) Patient-specific positioning guides do not consistently achieve the planned implant position in UKA. Knee Surg Sports Traumatol Arthrosc 3:752–758
Acknowledgements
The authors would like to thank Drs. M. Keulen, M.D., from the Dell Medical School at the University of Texas in Austin, USA, who served as external reader, and for his comments that greatly improved the manuscript.
Author information
Authors and Affiliations
Contributions
BK participated in the design of the study, acquisition of data and writing of the manuscript. AL participated in the design of the study and helped to draft the manuscript. MS participated in the design of the study and acquisition of data and helped to draft the manuscript. BB participated in the design of the study and helped to draft the manuscript. WT participated in the statistical analysis and helped to draft the manuscript. BJ participated in the design of the study and helped to draft the manuscript. PE participated in the design of the study and helped to draft the manuscript. NK participated in the design of the study and helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
One author (NK) is a paid consultant for Zimmer-Biomet. The other authors have no conflict of interest to be reported.
Funding
No funding has been received for this study.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kerens, B., Leenders, A.M., Schotanus, M.G.M. et al. Patient-specific instrumentation in Oxford unicompartmental knee arthroplasty is reliable and accurate except for the tibial rotation. Knee Surg Sports Traumatol Arthrosc 26, 1823–1830 (2018). https://doi.org/10.1007/s00167-017-4826-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4826-x