Abstract
Purpose
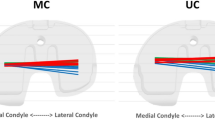
As the aims of changes in total knee arthroplasty (TKA) designs are to reinstate more natural kinematics, the current study evaluated the in vivo kinematics in patients who underwent a cruciate retaining gradually changing femoral radius (“G-CURVE”) against a cruciate retaining conventional changing femoral radius (“J-CURVE”) geometry TKA design. The hypothesis of the study is that the G-CURVE design would allow a substantial increase in the femoral rollback compared to the J-CURVE design.
Methods
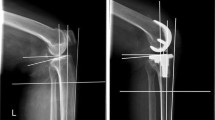
Retrospective study design. Thirty patients were included (G-CURVE, n = 20; J-CURVE, n = 10). Single-plane fluoroscopic analysis and marker-based motion capture gait analysis was performed to analyse dynamic tibiofemoral motion during weight-bearing and unloaded activities at 24 month after index surgery.
Results
The analysis of the medial and lateral points on the tibia plateau during the unloaded flexion–extension and the weight-bearing lunge activities revealed a significant difference in femoral rollback in G-CURVE TKA above 60° (p = 0.001) and 30° (p = 0.02) of knee flexion, respectively. Moreover, the lateral condyle of the G-CURVE showed a higher extent of femoral rollback while the lateral condyle of the J-CURVE rolled forward.
Conclusion
At 2 years post-operative, the G-CURVE TKA showed significant differences in femoro-tibial translation in comparison with the J-CURVE system, in vivo. The G-CURVE resulted in an increased lateral rollback and simultaneously in an elimination of the paradoxical medial roll-forward present in the J-CURVE design. Moreover, knee kinematics analysis showed significant differences between unloaded and weight-bearing conditions revealing the impact of load and muscle force. The analysis conducted in this study contributes to further understand the principal movement characteristics in widely used older designs in comparison with recently developed concepts to get a better overview on their potential benefits on in vivo kinematics.
Level of evidence
III.





Similar content being viewed by others
References
Abdel MP, Morrey ME, Jensen MR, Morrey BF (2011) Increased long-term survival of posterior cruciate-retaining versus posterior cruciate-stabilizing total knee replacements. J Bone Jt Surg Am 93:2072–2078
Andersen MS, Benoit DL, Damsgaard M, Ramsey DK, Rasmussen J (2010) Do kinematic models reduce the effects of soft tissue artefacts in skin marker-based motion analysis? An in vivo study of knee kinematics. J Biomech 43:268–273
Ardestani MM, Moazen M, Jin Z (2015) Contribution of geometric design parameters to knee implant performance: conflicting impact of conformity on kinematics and contact mechanics. Knee 22:217–224
Bailey O, Ferguson K, Crawfurd E, James P, May PA, Brown S, Blyth M, Leach WJ (2015) No clinical difference between fixed- and mobile-bearing cruciate-retaining total knee arthroplasty: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc 23:1653–1659
Becher C, Heyse TJ, Kron N, Ostermeier S, Hurschler C, Schofer MD, Fuchs-Winkelmann S, Tibesku CO (2009) Posterior stabilized TKA reduce patellofemoral contact pressure compared with cruciate retaining TKA in vitro. Knee Surg Sports Traumatol Arthrosc 17:1159–1165
Benoit DL, Damsgaard M, Andersen MS (2015) Surface marker cluster translation, rotation, scaling and deformation: their contribution to soft tissue artefact and impact on knee joint kinematics. J Biomech 48:2124–2129
Bertin KC, Komistek RD, Dennis DA, Hoff WA, Anderson DT, Langer T (2002) In vivo determination of posterior femoral rollback for subjects having a NexGen posterior cruciate-retaining total knee arthroplasty. J Arthroplasty 17:1040–1048
Bieger R, Huch K, Kocak S, Jung S, Reichel H, Kappe T (2014) The influence of joint line restoration on the results of revision total knee arthroplasty: comparison between distance and ratio-methods. Arch Orthop Trauma Surg 134:537–541
Boeth H, Duda GN, Heller MO, Ehrig RM, Doyscher R, Jung T, Moewis P, Scheffler S, Taylor WR (2013) Anterior cruciate ligament-deficient patients with passive knee joint laxity have a decreased range of anterior–posterior motion during active movements. Am J Sports Med 41:1051–1057
Cereatti A, Della Croce U, Cappozzo A (2006) Reconstruction of skeletal movement using skin markers: comparative assessment of bone pose estimators. J Neuroeng Rehabil 3:1–12
Choi WC, Ryu KJ, Lee S, Seong SC, Lee MC (2013) Painful patellar clunk or crepitation of contemporary knee prostheses. Clin Orthop Relat Res 471:1512–1522
Clary CW, Fitzpatrick CK, Maletsky LP, Rullkoetter PJ (2013) The influence of total knee arthroplasty geometry on mid-flexion stability: an experimental and finite element study. J Biomech 46:1351–1357
Dennis DA, Komistek RD, Mahfouz MR, Outten JT, Sharma A (2005) Mobile-bearing total knee arthroplasty: do the polyethylene bearings rotate? Clin Orthop Relat Res 440:88–95
Dennis DA, Komistek RD, Mahfouz MR, Walker SA, Tucker A (2004) A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res 428:180–189
Donadio J, Pelissier A, Boyer P, Massin P (2015) Control of paradoxical kinematics in posterior cruciate-retaining total knee arthroplasty by increasing posterior femoral offset. Knee Surg Sports Traumatol Arthrosc 23:1631–1637
Ehrig RM, Taylor WR, Duda GN, Heller MO (2006) A survey of formal methods for determining the centre of rotation of ball joints. J Biomech 39:2798–2809
Ehrig RM, Taylor WR, Duda GN, Heller MO (2007) A survey of formal methods for determining functional joint axes. J Biomech 40:2150–2157
Fantozzi S, Catani F, Ensini A, Leardini A, Giannini S (2006) Femoral rollback of cruciate-retaining and posterior-stabilized total knee replacements: in vivo fluoroscopic analysis during activities of daily living. J Orthop Res 24:2222–2229
Freeman MA, Pinskerova V (2005) The movement of the normal tibio-femoral joint. J Biomech 38:197–208
Garling EH, Kaptein BL, Geleijns K, Nelissen RG, Valstar ER (2005) Marker configuration model-based roentgen fluoroscopic analysis. J Biomech 38:893–901
Heyse TJ, Becher C, Kron N, Ostermeier S, Hurschler C, Schofer MD, Tibesku CO, Fuchs-Winkelmann S (2010) Patellofemoral pressure after TKA in vitro: highly conforming vs. posterior stabilized inlays. Arch Orthop Trauma Surg 130:191–196
Hube R, Mayr HO, Kalteis T, Matziolis G (2011) Extension first technique for TKA implantation. Oper Orthop Traumatol 23:241–248
Ji SJ, Zhou YX, Jiang X, Cheng ZY, Wang GZ, Ding H, Yang ML, Zhu ZL (2015) Effect of joint line elevation after posterior-stabilized and cruciate-retaining total knee arthroplasty on clinical function and kinematics. Chin Med J (Engl) 128:2866–2872
Jiang C, Liu Z, Wang Y, Bian Y, Feng B, Weng X (2016) Posterior cruciate ligament retention versus posterior stabilization for total knee arthroplasty: a meta-analysis. PLoS ONE 11:1–15
Kaptein BL, Valstar ER, Stoel BC, Rozing PM, Reiber JH (2003) A new model-based RSA method validated using CAD models and models from reversed engineering. J Biomech 36:873–882
Komistek RD, Scott RD, Dennis DA, Yasgur D, Anderson DT, Hajner ME (2002) In vivo comparison of femorotibial contact positions for press-fit posterior stabilized and posterior cruciate-retaining total knee arthroplasties. J Arthroplasty 17:209–216
Konno T, Onodera T, Nishio Y, Kasahara Y, Iwasaki N, Majima T (2014) Correlation between knee kinematics and patellofemoral contact pressure in total knee arthroplasty. J Arthroplasty 29:2305–2308
Kratzenstein S, Kornaropoulos EI, Ehrig RM, Heller MO, Popplau BM, Taylor WR (2012) Effective marker placement for functional identification of the centre of rotation at the hip. Gait Posture 36:482–486
LaCour MT, Sharma A, Carr CB, Komistek RD, Dennis DA (2014) Confirmation of long-term in vivo bearing mobility in eight rotating-platform TKAs. Clin Orthop Relat Res 472:2766–2773
Li G, Zayontz S, Most E, Otterberg E, Sabbag K, Rubash HE (2001) Cruciate-retaining and cruciate-substituting total knee arthroplasty: an in vitro comparison of the kinematics under muscle loads. J Arthroplasty 16:150–156
Moewis P, Wolterbeek N, Diederichs G, Valstar E, Heller MO, Taylor WR (2012) The quality of bone surfaces may govern the use of model based fluoroscopy in the determination of joint laxity. Med Eng Phys 34:1427–1432
Moskal JT, Capps SG (2014) Rotating-platform TKA no different from fixed-bearing TKA regarding survivorship or performance: a meta-analysis. Clin Orthop Relat Res 472:2185–2193
Petersen W, Rembitzki IV, Bruggemann GP, Ellermann A, Best R, Koppenburg AG, Liebau C (2014) Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop 38:319–328
Pinskerova V, Samuelson KM, Stammers J, Maruthainar K, Sosna A, Freeman MA (2009) The knee in full flexion: an anatomical study. J Bone Joint Surg Br 91:830–834
Ploegmakers MJ, Ginsel B, Meijerink HJ, de Rooy JW, de Waal Malefijt MC, Verdonschot N, Banks SA (2010) Physical examination and in vivo kinematics in two posterior cruciate ligament retaining total knee arthroplasty designs. Knee 17:204–209
Prins AH, Kaptein BL, Stoel BC, Nelissen RG, Reiber JH, Valstar ER (2011) Integrated contour detection and pose estimation for fluoroscopic analysis of knee implants. Proc Inst Mech Eng H 225:753–761
Saffarini M, Demey G, Nover L, Dejour D (2016) Evolution of trochlear compartment geometry in total knee arthroplasty. Ann Transl Med 4:1–6
Sharma A, Dennis DA, Zingde SM, Mahfouz MR, Komistek RD (2014) Femoral condylar contact points start and remain posterior in high flexing patients. J Arthroplasty 29:945–949
Shervin D, Pratt K, Healey T, Nguyen S, Mihalko WM, El-Othmani MM, Saleh KJ (2015) Anterior knee pain following primary total knee arthroplasty. World J Orthop 6:795–803
Stiehl JB, Dennis DA, Komistek RD, Keblish PA (2000) In vivo kinematic comparison of posterior cruciate ligament retention or sacrifice with a mobile bearing total knee arthroplasty. Am J Knee Surg 13:13–18
Taylor WR, Ehrig RM, Duda GN, Schell H, Seebeck P, Heller MO (2005) On the influence of soft tissue coverage in the determination of bone kinematics using skin markers. J Orthop Res 23:726–734
Taylor WR, Kornaropoulos EI, Duda GN, Kratzenstein S, Ehrig RM, Arampatzis A, Heller MO (2010) Repeatability and reproducibility of OSSCA, a functional approach for assessing the kinematics of the lower limb. Gait Posture 32:231–236
van Houten AH, Heesterbeek PJ, Wymenga AB (2016) Patella position is not a determinant for anterior knee pain 10 years after balanced gap total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24:2656–2662
Victor J, Banks S, Bellemans J (2005) Kinematics of posterior cruciate ligament-retaining and -substituting total knee arthroplasty: a prospective randomised outcome study. J Bone Jt Surg Br 87:646–655
Acknowledgements
We would like to thank Arne Schlausch for his assistance in the gait and fluoroscopic data acquisition as well as data post-processing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Tilman Pfitzner has received payment by Depuy Synthes for board membership, consultancy and development of educational presentations outside the present study. The rest of the authors declare that they have no conflict of interest in relation to this manuscript.
Funding
This study was funded by Depuy Synthes (Research Grant Nr: IIS2013009), BMBF 01EC1408A (OVERLOAD-PrevOP; SPO3) and EFRE (16409608, OrthoLoadLab).
Ethical approval
The local ethics committee approved the study (Approval-Nr: EA1/232/10).
Informed consent
All subjects provided written consent prior to participation.
Additional information
Tilman Pfitzner and Philippe Moewis shared first authorship.
Philipp von Roth and Georg N. Duda shared last authorship.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Pfitzner, T., Moewis, P., Stein, P. et al. Modifications of femoral component design in multi-radius total knee arthroplasty lead to higher lateral posterior femoro-tibial translation. Knee Surg Sports Traumatol Arthrosc 26, 1645–1655 (2018). https://doi.org/10.1007/s00167-017-4622-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4622-7