Abstract
Purpose
This randomized study investigates whether novices learning simulation-based arthroscopic skills in one anatomical joint environment can immediately transfer their learnt skills to another joint.
Methods
Medical students were randomized to a simulated diagnostic knee or shoulder arthroscopic task on benchtop training models. After nine task repetitions over 3 weeks on one model, each participant undertook the simulation task of the other anatomical joint. Performance was objectively measured using a validated electromagnetic motion analysis system and a validated global rating scale (GRS).
Results
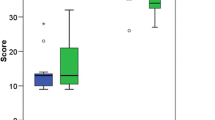
Eighteen students participated; eight started the knee task and ten the shoulder task. All participants demonstrated a learning curve in all parameters during task repetition (time taken, hand path length, number of hand movements and GRS scores; p < 0.001) with learning effects >1 SD from initial performance (range 1.1–2.2 SD). When the groups swapped models, there was no immediate evidence of skill transfer, with a significant drop in performance between the final training episode and the transfer task (all parameters p < 0.003). In particular, the transfer task performance was no better than the first episode performance on that model by these novices.
Conclusion
This study showed basic arthroscopic skills did not immediately transfer to an unfamiliar anatomical environment within a simulated setting. These findings have important clinical implications with regard to surgical training as they potentially challenge the assumption that arthroscopic skills acquired in one joint are universally transferrable to other joints. Future orthopaedic simulation training should aim to deliver exposure to a greater variety of arthroscopic procedures and joint environments. This would allow trainees to become familiar with the different arthroscopic setting before undertaking real surgery and consequently improve patient safety.
Level of evidence
Therapeutic, Level II.







Similar content being viewed by others
References
Alvand A, Auplish S, Gill H, Rees J (2011) Innate arthroscopic skills in medical students and variation in learning curves. J Bone Joint Surg Am 93(1–9):e115
Tuijthof GJ, van Sterkenburg MN, Sierevelt IN, van Oldenrijk J, Van Dijk CN, Kerkhoffs GM (2010) First validation of the passport training environment for arthroscopic skills. Knee Surg Sports Traumatol Arthrosc 18:218–224
Cameron JL (1997) William Stewart Halsted. Our surgical heritage. Ann Surg 225:445–458
Damadi A, Davis AT, Saxe A, Apelgren K (2007) ACGME duty-hour restrictions decrease resident operative volume: a 5-year comparison at an ACGME-accredited university general surgery residency. J Surg Educ 64:256–259
Chikwe J, De Souza AC, Pepper JR (2004) No time to train the surgeons. Br Med J 328:418–419
Slade Shantz JAS, Leiter JR, Gottschalk T, MacDonald PB (2014) The internal validity of arthroscopic simulators and their effectiveness in arthroscopic education. Knee Surg Sports Traumatol Arthrosc 22:33–40
Pedowitz RA, Marsh JL (2012) Motor skills training in orthopaedic surgery: a paradigm shift toward a simulation-based educational curriculum. J Am Acad Orthop Surg 20:407–409
Al-Ali S, Alvand A, Gill HS, Beard DJ, Jackson W, Price AJ, Rees JL (2012) Objective assessment of the learning curve for arthroscopic meniscal repair. J Bone Joint Surg Br 94:74
Alvand A, Auplish S, Gill HS, Rees JL (2012) The impact of training on the arthroscopic performance of medical students: a randomised study. J Bone Joint Surg Br 94:39
Alvand A, Logishetty K, Middleton R, Khan T, Jackson WF, Price AJ, Rees JL (2013) Validating a global rating scale to monitor individual resident learning curves during arthroscopic knee meniscal repair. Arthroscopy 29:906–912
Howells NR, Auplish S, Hand GC, Gill HS, Carr AJ, Rees JL (2009) Retention of arthroscopic shoulder skills learned with use of a simulator. Demonstration of a learning curve and loss of performance level after a time delay. J Bone Joint Surg Am 91:1207–1213
Howells NR, Gill HS, Carr AJ, Price AJ, Rees JL (2008) Transferring simulated arthroscopic skills to the operating theatre. J Bone Joint Surg Br 90:494–499
Jackson WFM, Khan T, Alvand A, Al-Ali S, Gill HS, Price AJ, Rees JL (2012) Learning and retaining simulated arthroscopic meniscal repair skills. J Bone Joint Surg Am 94(e132):1–8
Pollard TC, Khan T, Price AJ, Gill HS, Glyn-Jones S, Rees JL (2012) Simulated hip arthroscopy skills: learning curves with the lateral and supine patient positions. a randomized trial. J Bone Joint Surg Am 94(1–10):e68
Alvand A, Auplish S, Khan T, Gill HS, Rees JL (2011) Identifying orthopaedic surgeons of the future the inability of some medical students to achieve competence in basic arthroscopic tasks despite training: a randomised study. J Bone Joint Surg Br 93:1586–1591
Howells NR, Brinsden MD, Gill RS, Carr AJ, Rees JL (2008) Motion analysis: a validated method for showing skill levels in arthroscopy. Arthroscopy 24:335–342
Insel A, Carofino B, Leger R, Arciero R, Mazzocca AD (2009) The development of an objective model to assess arthroscopic performance. J Bone Joint Surg Am 91:2287–2295
Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT, Erwin PJ, Hamstra SJ (2011) Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. J Am Med Assoc 306:978–988
Henn RF, Shah N, Warner JJ, Gomoll AH (2013) Shoulder arthroscopy simulator training improves shoulder arthroscopy performance in a cadaveric model. Arthroscopy 29:982–985
Naik VN, Matsumoto ED, Houston PL, Hamstra SJ, Yeung RY-M, Mallon JS, Martire TM (2001) Fiberoptic orotracheal intubation on anesthetized patients: do manipulation skills learned on a simple model transfer into the operating room? Anesthesiology 95:343–348
Park J, MacRae H, Musselman LJ, Rossos P, Hamstra SJ, Wolman S, Reznick RK (2007) Randomized controlled trial of virtual reality simulator training: transfer to live patients. Am J Surg 194:205–211
Stefanidis D, Hope WW, Korndorffer JR, Markley S, Scott DJ (2010) Initial laparoscopic basic skills training shortens the learning curve of laparoscopic suturing and is cost-effective. J Am Coll Surg 210:436–440
Zendejas B, Cook DA, Bingener J, Huebner M, Dunn WF, Sarr MG, Farley DR (2011) Simulation-based mastery learning improves patient outcomes in laparoscopic inguinal hernia repair: a randomized controlled trial. Ann Surg 254:502–511
Ström P, Kjellin A, Hedman L, Wredmark T, Felländer-Tsai L (2004) Training in tasks with different visual-spatial components does not improve virtual arthroscopy performance. Surg Endosc 18:115–120
Kassab E, Tun JK, Kneebone RL (2012) A novel approach to contextualized surgical simulation training. Simul Healthc 7:155–161
Kneebone RL, Nestel D, Vincent C, Darzi A (2007) Complexity, risk and simulation in learning procedural skills. Med Educ 41:808–814
Sadideen H, Hamaoui K, Saadeddin M, Kneebone R (2012) Simulators and the simulation environment: getting the balance right in simulation-based surgical education. Int J Surg 10:458–462
Schaverien MV (2010) Development of expertise in surgical training. J Surg Educ 67:37–43
Ericsson KA, Krampe RT, Tesch-Römer C (1993) The role of deliberate practice in the acquisition of expert performance. Psychol Rev 100:363–406
Ericsson KA (1996) The acquisition of expert performance: an introduction to some of the issues. In: Ericsson KA (ed) The road to excellence: the acquisition of expert performance in the arts and sciences, sports and games. Lawrence Erlbaum Associates, Mahwah, pp 1–50
Ericsson KA (2004) Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med 79:S70–S81
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ferguson, J., Middleton, R., Alvand, A. et al. Newly acquired arthroscopic skills: Are they transferable during simulator training of other joints?. Knee Surg Sports Traumatol Arthrosc 25, 608–615 (2017). https://doi.org/10.1007/s00167-015-3766-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3766-6