Abstract
Purpose
The reliability of the Rockwood classification, the gold standard for acute acromioclavicular (AC) joint separations, has not yet been tested. The purpose of this study was to investigate the reliability of visual and measured AC joint lesion grades according to the Rockwood classification.
Methods
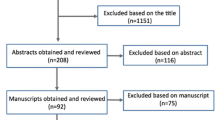
Four investigators (two shoulder specialists and two second-year residents) examined radiographs (bilateral panoramic stress and axial views) in 58 patients and graded the injury according to the Rockwood classification using the following sequence: (1) visual classification of the AC joint lesion, (2) digital measurement of the coracoclavicular distance (CCD) and the horizontal dislocation (HD) with Osirix Dicom Viewer (Pixmeo, Switzerland), (3) classification of the AC joint lesion according to the measurements and (4) repetition of (1) and (2) after repeated anonymization by an independent physician. Visual and measured Rockwood grades as well as the CCD and HD of every patient were documented, and a CC index was calculated (CCD injured/CCD healthy). All records were then used to evaluate intra- and interobserver reliability.
Results
The disagreement between visual and measured diagnosis ranged from 6.9 to 27.6 %. Interobserver reliability for visual diagnosis was good (0.72–0.74) and excellent (0.85–0.93) for measured Rockwood grades. Intraobserver reliability was good to excellent (0.67–0.93) for visual diagnosis and excellent for measured diagnosis (0.90–0.97). The correlations between measurements of the axial view varied from 0.68 to 0.98 (good to excellent) for interobserver reliability and from 0.90 to 0.97 (excellent) for intraobserver reliability.
Conclusion
Bilateral panoramic stress and axial radiographs are reliable examinations for grading AC joint injuries according to Rockwood’s classification. Clinicians of all experience levels can precisely classify AC joint lesions according to the Rockwood classification. We recommend to grade acute ACG lesions by performing a digital measurement instead of a sole visual diagnosis because of the higher intra- and interobserver reliability.
Level of evidence
Case series, Level IV.


Similar content being viewed by others
References
Alexander OM (1949) Dislocation of the acromioclavicular joint. Radiography 15(179):260
Alexander OM (1954) Radiography of the acromioclavicular articulation. Med Radiogr Photogr 30(2):34–39
Allman FL Jr (1967) Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg Am 49(4):774–784
Balke M, Schneider MM, Shafizadeh S, Bathis H, Bouillon B, Banerjee M (2013) Current state of treatment of acute acromioclavicular joint injuries in Germany: is there a difference between specialists and non-specialists? A survey of German trauma and orthopaedic departments. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2795-2
Bathis H, Tingart M, Bouillon B, Tiling T (2000) Conservative or surgical therapy of acromioclavicular joint injury—what is reliable? A systematic analysis of the literature using “evidence-based medicine” criteria. Chirurg 71(9):1082–1089
Beitzel K, Cote MP, Apostolakos J, Solovyova O, Judson CH, Ziegler CG, Edgar CM, Imhoff AB, Arciero RA, Mazzocca AD (2013) Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy 29(2):387–397
Gstettner C, Tauber M, Hitzl W, Resch H (2008) Rockwood type III acromioclavicular dislocation: surgical versus conservative treatment. J Shoulder Elbow Surg 17(2):220–225
Habermeyer P, Lichtenberg S, Magosch P (2010) Schulterchirurgie, vol 4. Urban & Fischer Verlag/Elsevier GmbH, Heidelberg
Kraeutler MJ, Williams GR Jr, Cohen SB, Ciccotti MG, Tucker BS, Dines JS, Altchek DW, Dodson CC (2012) Inter- and intraobserver reliability of the radiographic diagnosis and treatment of acromioclavicular joint separations. Orthopedics 35(10):e1483–1487
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174
Mazzocca AD, Arciero RA, Bicos J (2007) Evaluation and treatment of acromioclavicular joint injuries. Am J Sports Med 35(2):316–329
Nemec U, Oberleitner G, Nemec SF, Gruber M, Weber M, Czerny C, Krestan CR (2011) MRI versus radiography of acromioclavicular joint dislocation. AJR Am J Roentgenol 197(4):968–973
Phillips AM, Smart C, Groom AF (1998) Acromioclavicular dislocation. Conservative or surgical therapy. Clin Orthop Relat Res 353:10–17
Raschke MJ, Haas NP (2012) Unfallchirurgie. In: Siewert JR, Stein HJ (eds) Chirurgie, vol 9. Springer, Berlin, pp 908–909
Rockwood CA, Green DP (1975) Fractures in adults, 2nd edn. J.B. Lippincott, Philadelphia
Ruchholtz S, Wirtz DC (2012) Orthopädie und Unfallchirurgie essentials—Intensivkurs zur Weiterbildung, vol 2. Georg Thieme Verlag, Stuttgart
Taft TN, Wilson FC, Oglesby JW (1987) Dislocation of the acromioclavicular joint. An end-result study. J Bone Joint Surg Am 69(7):1045–1051
Tauber M (2014) Acromioclavicular injuries in professional athletes. Orthopade. doi:10.1007/s00132-013-2148-3
Tossy JD, Mead NC, Sigmond HM (1963) Acromioclavicular separations: useful and practical classification for treatment. Clin Orthop Relat Res 28:111–119
Vaisman A, Villalon Montenegro IE, Tuca De Diego MJ, Valderrama Ronco J (2014) A novel radiographic index for the diagnosis of posterior acromioclavicular joint dislocations. Am J Sports Med 42(1):112–116
Wellmann M, Smith T (2012) Epidemiology, anatomy, biomechanics and imaging of acromioclavicular joint injuries. Unfallchirurg 115(10):867–871
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schneider, M.M., Balke, M., Koenen, P. et al. Inter- and intraobserver reliability of the Rockwood classification in acute acromioclavicular joint dislocations. Knee Surg Sports Traumatol Arthrosc 24, 2192–2196 (2016). https://doi.org/10.1007/s00167-014-3436-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3436-0