Abstract
Purpose
The purpose of the present study was to determine the value of shoulder magnetic resonance imaging (MRI) obtained in the community setting interpreted by musculoskeletal radiologists in patients with shoulder pain initiated by a single non-dislocating shoulder trauma.
Methods
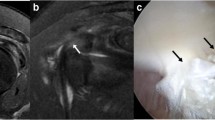
In 56 of 61 consecutive patients who underwent shoulder arthroscopy due to pain after a single non-dislocating shoulder trauma, the data sets of non-contrast MRI were complete. These were retrospectively interpreted by three radiologists specialized on musculoskeletal MRI who were blinded for patients’ history and who did not have access to the reports of arthroscopy. Standard evaluation forms were used to assess the MRIs for superior labrum anterior and posterior (SLAP) lesions, anterior or posterior labrum lesions, lesions of the long head of biceps tendon (LHB) and for partial tears of the supraspinatus tendon and the upper quarter of the subscapularis tendon. Quality of the MRI was assessed by each radiologist on a four-point scale.
Results
The pooled sensitivity for the three radiologists for the detection of SLAP lesions was 45.0 %, for anterior or posterior labrum tears 77.8 and 66.7 %, for lesions of the LHB 63.2 % and for partial tears of the supraspinatus or subscapularis tendon tears 84.8 and 33.3 %. Corresponding inter-rater reliabilities were poor (SLAP lesions) to substantial (anterior labrum tears). Quality of MRI only influenced the accuracy for the detection of posterior labrum tears.
Conclusion
A non-contrast shoulder MRI obtained in the community setting after non-dislocating shoulder trauma has a moderate sensitivity for most intraarticular pathologies when interpreted by musculoskeletal radiologists. Accuracy is dependent on the observer and not on the assessed quality.
Level of evidence
Case series, Level IV.






Similar content being viewed by others
References
Adams CR, Schoolfield JD, Burkhart SS (2010) Accuracy of preoperative magnetic resonance imaging in predicting a subscapularis tendon tear based on arthroscopy. Arthroscopy 26:1427–1433
Adams CR, Brady PC, Koo SS, Narbona P, Arrigoni P, Karnes GJ, Burkhart SS (2012) A systematic approach for diagnosing subscapularis tendon tears with preoperative magnetic resonance imaging scans. Arthroscopy 28:1592–1600
Amin MF, Youssef A (2012) The diagnostic value of magnetic resonance arthrography of the shoulder in detection and grading of SLAP lesions: comparison with arthroscopic findings. Eur J Radiol 81:2343–2347
Applegate GR, Hewitt M, Snyder SJ, Watson E, Kwak S, Resnick D (2004) Chronic labral tears: value of magnetic resonance arthrography in evaluating the glenoid labrum and labral-bicipital complex. Arthroscopy 20:959–963
Barth JR, Burkhart SS, De Beer JF (2006) The bear-hug test: a new and sensitive test for diagnosing a subscapularis tear. Arthroscopy 22:1076–1084
Bartsch M, Greiner S, Haas NP, Scheibel M (2010) Diagnostic values of clinical tests for subscapularis lesions. Knee Surg Sports Traumatol Arthrosc 18:1712–1717
Connolly KP, Schwartberg RS, Reuss B, Crumble D, Homan BM (2013) Sensitivity and specifity of non-contrast magnetic resonance imaging reports in the diagnosis of type-II superior labral anterior–posterior lesions in the community setting. J Bone Joint Surg-A 20:308–313
Fallahi F, Green N, Gadde S, Jeavons L, Armstrong P, Jonker L (2013) Indirect magnetic resonance arthrography of the shoulder; a reliable diagnostic tool for investigation of suspected labral pathology. Skelet Radiol 42:1225–1233
Foad A, Wijdicks CA (2012) The accuracy of magnetic resonance imaging magnetic resonance arthrogram versus arthroscopy in the diagnosis of subscapularis tendon injury. Arthroscopy 28:636–641
Fox JA, Noerdlinger MA, Romeo AA (2003) Arthroscopic subscapularis repair. Tech Shoulder Elbow Surg 4:154–168
Freeman R, Khanna S, Ricketts D (2013) Inappropriate requests for magnetic resonance scans of the shoulder. Int Orthop 37:2181–2184
Grant JA, Miller BS, Jacobson JA, Morag Y, Bedi A, Carpenter JE, The MOON shoulder group (2012) Intra- and inter-rater reliability of the detection of tears of the supraspinatus central tendon on MRI by shoulder surgeons. J Shoulder Elbow Surg 21:1–7
Gusmer PB, Potter HG, Schatz JA, Wickiewicz TL, Altchek DW, O’Brien SJ, Warren RF (2006) Labral injuries: accuracy of detection with unenhanced MR imaging of the shoulder. Radiology 200:519–524
Habermeyer P, Krieter C, Kang-lai T, Lichtenberg S, Magosch P (2008) A new arthroscopic classification of articular-sided footprint lesions: a prospective comparison with Snyder’s and Ellman’s classification. J Shoulder Elbow Surg 17:909–913
Houtz CG, Schwartzberg RS, Barry JA, Reuss BL, Papa L (2011) Shoulder MRI accuracy in the community setting. J Shoulder Elbow Surg 20:537–542
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Maffet MW, Gartsman GM, Moseley B (1995) Superior labrum-biceps tendon complex lesions of the shoulder. Am J Sports Med 23:93–98
Major NM, Browne J, Domzalski J, Cothran RL, Helms CA (2011) Evaluation of glenoid labrum with 3-T MRI: is intraarticular contrast necessary? AJR 19:1139–1144
Neviaser TJ (1993) The GLAD lesion: another cause of anterior shoulder pain. Arthroscopy 9:22–23
Nicola T (1942) Anterior dislocation of the shoulder: the role of the articular capsule. J Bone Joint Surg-A 25:614–616
Philipps JC, Cook C, Beaty S, Kissenberth MJ, Siffri P, Hawkins RJ (2013) Validity of noncontrast magnetic resonance imaging in diagnosing superior labrum anterior–posterior tears. J Shoulder Elbow Surg 22:3–8
Reuss BL, Schwartzberg R, Zlatkin MB, Cooperman A, Dixon JR (2006) Magnetic resonance imaging accuracy for the diagnosis of superior labrum anterior–posterior lesions in the community setting: eighty-three arthroscopically confirmed cases. J Shoulder Elbow Surg 15:580–585
Schaeffeler C, Waldt S, Holzapfel K, Kirchhoff C, Jungmann PM, Wolf P, Schröder M, Rummeny EJ, Imhoff AB, Woertler K (2012) Lesions of the biceps pulley: diagnostic accuracy of MR arthrography of the shoulder and evaluation of previously described and new diagnostic signs. Radiology 264:504–513
Smith TO, Daniell H, Geere J-A, Toms AP, Hing CB (2012) The diagnostic accuracy of MRI for the detection of partial- and full-thickness rotator cuff tears in adults. Magn Resonance Imaging 30:336–446
Smith TO, Drew BT, Toms AP (2012) A meta-analysis of the diagnostic test accuracy of MRA and MRI for the detection of glenoid labral injury. Arch Orthop Trauma Surg 132:905–919
Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ (1990) SLAP lesions of the shoulder. Arthroscopy 6:274–279
Spencer EE, Dunn WR, Wright RW, Wolf BR, Spindler KP, McCarthy E, Ma CB, Jones G, Safran M, Holloway GB, Kuhn JE, Shoulder Multicenter Orthopaedic Outcomes Network (Shoulder MOON Group) (2008) Interobserver agreement in the classification of rotator cuff tears using magnetic resonance imaging. Am J Sports Med 36:99–103
Stetson WB, Phillips T, Deutsch A (2005) The use of magnetic resonance arthrography to detect partial-thickness rotator cuff tears. J Bone Joint Surg-A 87:81–88
Suder PA, Hougaard F, Frich LH, Rasmussen OS, Lundorf E (1994) Intraarticular findings in the chronically painful shoulder. A study of 32 posttraumatic cases. Acta Orthop Scand 65:339–343
Suder PA, Frich LH, Hougaard K, Lundorf E, Jakobsen BW (1995) Magnetic resonance imaging evaluation of capsulolabral tears after traumatic primary anterior shoulder dislocation. A prospective comparison with arthroscopy of 25 cases. J Shoulder Elbow Surg 4:419–428
Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H, Kobayashi T (2010) Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg 19:116–120
Conflict of interest
No author declares conflicts of interest regarding this publication.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Banerjee, M., Müller-Hübenthal, J., Grimme, S. et al. Moderate value of non-contrast magnetic resonance imaging after non-dislocating shoulder trauma. Knee Surg Sports Traumatol Arthrosc 24, 1888–1895 (2016). https://doi.org/10.1007/s00167-014-3102-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3102-6