Abstract
Purpose
The aim of our study was to evaluate knee rotational laxity and proprioceptive function 2 years after partial anterior cruciate ligament (ACL) reconstruction. According to our hypothesis, partial ACL reconstruction could restore knee laxity and function to the intact level.
Methods
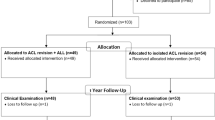
We conducted a study in fifteen consecutive patients undergoing partial ACL reconstruction. Fifteen anteromedial bundle tears were identified intraoperatively. Partial ACL reconstructions were performed by the same senior surgeon using a single-incision technique. A bone–patellar tendon–bone graft was used in 13 cases and a double-stranded semitendinosus graft in 2 cases of chronic patellar tendonitis. The mean age at surgery was 29 years. The time between ACL tear and surgery averaged 7.8 months (range 2.5–29.5 months).
We developed an original device designed to assess knee proprioception (passive and active) and measure weight-bearing rotational laxity in full extension and at 30°, 60° and 90° of knee flexion. All measurements were taken on both the reconstructed and healthy knee.
Results
The mean follow-up of the study was 3.4 years (range 2.6–4.4). No statistically significant difference in rotational laxity, active or passive proprioception could be observed between the reconstructed and healthy knee. External rotation was significantly greater than internal rotation in full extension and at 30° of flexion in the reconstructed and the healthy knee (P < 0.05). For each knee, active proprioception was found to be significantly different (higher) than passive proprioception (P < 0.05).
Conclusion
Our study did not detect any difference in rotational laxity and proprioception between the reconstructed and the healthy knee. Therefore, partial ACL reconstruction appears to restore satisfactory knee laxity and function in case of partial ACL tear.
Level of evidence
IV.


Similar content being viewed by others
References
Adachi N, Ochi M, Uchio Y, Iwasa J, Ryoke K, Kuriwaka M (2002) Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scand 73(3):330–334
Adachi N, Ochi M, Uchio Y, Sumen Y (2000) Anterior cruciate ligament augmentation under arthroscopy. A minimum 2-year follow-up in 40 patients. Arch Orthop Trauma Surg 120(3–4):128–133
Beard DJ, Kyberd PJ, Fergusson CM, Dodd CA (1993) Proprioception after rupture of the anterior cruciate ligament. An objective indication of the need for surgery? J Bone Joint Surg Br 75(2):311–315
Boerboom AL, Huizinga MR, Kaan WA, Stewart RE, Hof AL, Bulstra SK, Diercks RL (2008) Validation of a method to measure the proprioception of the knee. Gait Posture 28(4):610–614
Corrigan JP, Cashman WF, Brady MP (1992) Proprioception in the cruciate deficient knee. J Bone Joint Surg Br 74(2):247–250
Fremerey RW, Lobenhoffer P, Zeichen J, Skutek M, Bosch U, Tscherne H (2000) Proprioception after rehabilitation and reconstruction in knees with deficiency of the anterior cruciate ligament: a prospective, longitudinal study. J Bone Joint Surg Br 82(6):801–806
Furman W, Marshall JL, Girgis FG (1976) The anterior cruciate ligament. A functional analysis based on postmortem studies. J Bone Joint Surg Am 58(2):179–185
Gobbi A, Mahajan V, Karnatzikos G, Nakamura N (2011) Single- versus double-bundle ACL reconstruction: is there any difference in stability and function at 3-year followup? Clin Orthop Relat Res [Epub ahead of print]
Hewett TE, Paterno MV, Myer GD (2002) Strategies for enhancing proprioception and neuromuscular control of the knee. Clin Orthop Relat Res 402:76–94
Ochi M, Iwasa J, Uchio Y, Adachi N, Sumen Y (1999) The regeneration of sensory neurones in the reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br 81(5):902–906
Rozzi SL, Lephart SM, Gear WS, Fu FH (1999) Knee joint laxity and neuromuscular characteristics of male and female soccer and basketball players. Am J Sports Med 27(3):312–319
Skinner HB, Barrack RL, Cook SD (1984) Age-related decline in proprioception. Clin Orthop Relat Res 184:208–211
Sonnery-Cottet B, Lavoie F, Ogassawara R, Scussiato RG, Kidder JF, Chambat P (2010) Selective anteromedial bundle reconstruction in partial ACL tears: a series of 36 patients with mean 24 months follow-up. Knee Surg Sports Traumatol Arthrosc 18(1):47–51
Zaffagnini S, Martelli S, Falcioni B, Motta M, Marcacci M (2000) Rotational laxity after anterior cruciate ligament injury by kinematic evaluation of clinical tests. J Med Eng Technol 24(5):230–236
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chouteau, J., Testa, R., Viste, A. et al. Knee rotational laxity and proprioceptive function 2 years after partial ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 20, 762–766 (2012). https://doi.org/10.1007/s00167-012-1879-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-1879-8