Abstract
Purpose
Recent advances in the treatment of ACL ruptures employ platelet-rich plasma combined with collagen to modulate growth factor release from platelets to stimulate healing. Among the most notable of these growth factors is VEGF, which is a potent mitogen and stimulator of vascular growth and healing. However, the effect of such a growth factor on healing depends on the cellular ability to bind with its receptor. The purpose of this study was to test (1) whether the strength of a tissue-engineered ACL repair is associated with VEGF receptors’ mRNA expression of ACL cells and (2) whether age influences this association.
Method
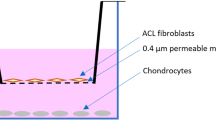
Nineteen female Yucatan pigs underwent enhanced ACL repair. Biomechanical testing was performed after 15 weeks of healing. Messenger RNA of VEGF receptors 1 and 2 in ACL fibroblasts was assessed by RT–PCR. The ACL structural properties were regressed on receptor expression levels in a multivariate model including serum levels of VEGF, age, and weight as potential confounders.
Result
While maximum load and linear stiffness were independent of VEGF receptor expression, VEGF receptor 1 was associated with displacement (positively) and yield load (negatively). In a multivariate model of VEGF receptor expression and biomechanics, age was associated with maximum load and yield load.
Conclusion
These findings suggest that high VEGF receptor expression, even more so at higher age, results in a more compliant scar, which in turn may lead to greater knee laxity and a compromised clinical result.

Similar content being viewed by others
References
Carmeliet P (2003) Angiogenesis in health and disease. Nat Med 9(6):653–660
Casteleyn P (1999) Management of anterior cruciate ligament lesions: surgical fashion, personal whim or scientific evidence? Study of medium and long-term results. Acta Orthop Belg 65:327–339
Cheng M, Wang H, Yoshida R, Murray MM (2009) Platelets and plasma proteins are both required to stimulate collagen gene expression by anterior cruciate ligament cells in three-dimensional culture. Tissue Eng Part A 16(5):1479–1489
Cohen M, Amaro JT, Ejnisman B, Carvalho RT, Nakano KK, Peccin MS, Teixeira R, Laurino CF, Abdalla RJ (2007) Anterior cruciate ligament reconstruction after 10 to 15 years: association between meniscectomy and osteoarthrosis. Arthroscopy 23(6):629–634
Dupont WD, Plummer WD (1990) Power and sample size calculations: a review and computer program. Control Clin Trial 11:116–128
Dupont WD, Plummer WD Jr (1998) Power and sample size calculations for studies involving linear regression. Control Clin Trial 19(6):589
Everts PA, Knape JT, Weibrich G, Schonberger JP, Hoffmann J, Overdevest EP, Box HA, van Zundert A (2006) Platelet-rich plasma and platelet gel: a review. J Extra Corpor Technol 38(2):174–187
Fleming BC, Carey JL, Spindler KP, Murray MM (2008) Can suture repair of ACL transection restore normal anteroposterior laxity of the knee? An ex vivo study. J Orthop Res 26(11):1500–1505
Fleming BC, Magarian EM, Harrison SL, Paller DJ, Murray MM (2010) Collagen scaffold supplementation does not improve the functional properties of the repaired anterior cruciate ligament. J Orthop Res 28(6):703–709
Fleming BC, Spindler KP, Palmer M, Magarian E, Murray MM (2009) Collagen-platelet composites improve the biomechanical properties of healing ACL grafts in a porcine model. Am J Sports Med 37(8):1554–1563
Hofstaetter JG, Saad FA, Samuel RE, Wunderlich L, Choi YH, Glimcher MJ (2004) Differential expression of VEGF isoforms and receptors in knee joint menisci under systemic hypoxia. Biochem Biophys Res Commun 324(2):667–672
Hofstaetter JG, Saad FA, Sunk IG, Bobacz K, Friehs I, Glimcher MJ (2007) Age-dependent expression of VEGF isoforms and receptors in the rabbit anterior cruciate ligament. Biochim Biophys Acta 1770(7):997–1002
Hofstaetter JG, Wunderlich L, Samuel RE, Saad FA, Choi YH, Glimcher MJ (2005) Systemic hypoxia alters gene expression levels of structural proteins and growth factors in knee joint cartilage. Biochem Biophys Res Commun 330(2):386–394
Hou Y, Mao Z, Wei X, Lin L, Chen L, Wang H, Fu X, Zhang J, Yu C (2009) Effects of transforming growth factor-beta1 and vascular endothelial growth factor 165 gene transfer on Achilles tendon healing. Matrix Biol 28(6):324–335
Joshi SM, Mastrangelo AN, Magarian EM, Fleming BC, Murray MM (2009) Collagen-platelet composite enhances biomechanical and histologic healing of the porcine anterior cruciate ligament. Am J Sports Med 37(12):2401–2410
Kessler MA, Behrend H, Henz S, Stutz G, Rukavina A, Kuster MS (2008) Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc 16(5):442–448
Kilian O, Alt V, Heiss C, Jonuleit T, Dingeldein E, Flesch I, Fidorra U, Wenisch S, Schnettler R (2005) New blood vessel formation and expression of VEGF receptors after implantation of platelet growth factor-enriched biodegradable nanocrystalline hydroxyapatite. Growth Factors 23(2):125–133
Lind M, Menhert F, Pedersen AB (2008) The first results from the Danish ACL reconstruction registry: epidemiologic and 2 year follow-up results from 5,818 knee ligament reconstructions. Knee Surg Sports Traumatol Arthrosc
Lohmander LS, Englund M, Dahl L, Roos EM (2007) The long-term consequence of anterior cruciate ligament and meniscus injuries. Am J Sports Med 35:1756–1769
Lohmander LS, Ostenberg A, Englund M, Roos H (2004) High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum 50(10):3145–3152
Mastrangelo A, Magarian E, Palmer M, Vavken P, Murray M (2009) The effect of skeletal maturity on the regenerative function of intrinsic ACL cells. J Orthop Res 28(5):644–651
Mastrangelo A, Vavken P, Fleming B, Harrison S, Murray M (2011) Reduced platelet concentration does not harm PRP effectiveness for ACL repair in a porcine in vivo model. J Orthop Res (in press)
Mastrangelo AN, Haus BM, Vavken P, Palmer MP, Machan JT, Murray MM (2010) Immature animals have higher cellular density in the healing anterior cruciate ligament than adolescent or adult animals. J Orthop Res 28(8):1100–1106
Mastrangelo AN, Magarian EM, Palmer MP, Vavken P, Murray MM (2010) The effect of skeletal maturity on the regenerative function of intrinsic ACL cells. J Orthop Res 28(5):644–651
Murray MM, Magarian EM, Harrison SL, Zurakowski D, Fleming BC (2010) The effect of skeletal maturity on functional healing of the anterior cruciate ligament. J Bone Joint Surg Am 92(11):2039–2049
Murray MM, Martin SD, Martin TL, Spector M (2000) Histological changes in the human anterior cruciate ligament after rupture. J Bone Joint Surg Am 82(10):1387–1397
Murray MM, Palmer M, Abreu E, Spindler KP, Zurakowski D, Fleming BC (2009) Platelet-rich plasma alone is not sufficient to enhance suture repair of the ACL in skeletally immature animals: an in vivo study. J Orthop Res 27(5):639–645
Odorisio T, Schietroma C, Zaccaria M, Cianfarani F, Tiveron C, Tatangelo L, Failla C, Zambruno G (2002) Mice overexpressing placenta growth factor exhibit increased vascularization and vessel permeability. J Cell Sci 115:2559–2567
Petersen W, Pufe T, Unterhauser F, Zantop T, Mentlein R, Weiler A (2003) The splice variants 120 and 164 of the angiogenic peptide vascular endothelial cell growth factor (VEGF) are expressed during Achilles tendon healing. Arch Orthop Trauma Surg 123(9):475–480
Petersen W, Unterhauser F, Pufe T, Zantop T, Sudkamp NP, Weiler A (2003) The angiogenic peptide vascular endothelial growth factor (VEGF) is expressed during the remodeling of free tendon grafts in sheep. Arch Orthop Trauma Surg 123(4):168–174
Petrova T, Makinen T, Alitalo K (1999) Signaling via vascular endothelial growth factor receptors. Exp Cell Res 253(117)
Rahimi N (2006) VEGFR-1 and VEGFR-2: two non-identical twins with a unique physiognomy. Front Biosci 11:818–829
Spindler KP, Murray MM, Carey JL, Zurakowski D, Fleming BC (2009) The use of platelets to affect functional healing of an anterior cruciate ligament (ACL) autograft in a caprine ACL reconstruction model. J Orthop Res 27(5):631–638
Vavken P, Culen G, Dorotka R (2008) Management of confounding in controlled orthopaedic trials: a cross-sectional study. Clin Orthop Relat Res 466(4):985–989
Vavken P, Heinrich KM, Koppelhuber C, Rois S, Dorotka R (2009) The use of confidence intervals in reporting orthopaedic research findings. Clin Orthop Relat Res 467(12):3334–3339
Vavken P, Murray MM (2009) Translational studies in ACL repair. Tissue Eng Part B 16(1):5–11
Vavken P, Saad F, Murray M (2010) Age-dependence of expression of growth factor receptors in porcine ACL fibroblasts. J Orthop Res 28(8):1107–1112
Weibrich G, Kleis WK, Hafner G, Hitzler WE (2002) Growth factor levels in platelet-rich plasma and correlations with donor age, sex, and platelet count. J Craniomaxillofac Surg 30(2):97–102
Yancopoulos G, Davis S, Gale N, Rudge J, Wiegand S, Holash J (2000) Vascular-specific growth factors and blood vessel formation. Nature 407(6801):242–248
Yoshikawa T, Tohyama H, Katsura T, Kondo E, Kotani Y, Matsumoto H, Toyama Y, Yasuda K (2006) Effects of local administration of vascular endothelial growth factor on mechanical characteristics of the semitendinosus tendon graft after anterior cruciate ligament reconstruction in sheep. Am J Sports Med 34(12):1918–1925
Acknowledgment
This study was funded by the NIH NIAMS Grant R01 AR052772 and NIH Grant AR054099.
Conflict of interest
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vavken, P., Saad, F.A., Fleming, B.C. et al. VEGF receptor mRNA expression by ACL fibroblasts is associated with functional healing of the ACL. Knee Surg Sports Traumatol Arthrosc 19, 1675–1682 (2011). https://doi.org/10.1007/s00167-011-1443-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1443-y