Abstract
Snoring and obstructive sleep apnea (OSA) are often associated with uvula vibrations and pharynx constrictions. However, successful treatment of snoring or accurate diagnosis of OSA has been proven challenging. This study aimed to identify acoustic indexes that were sensitive to underlying airway structural or kinematic variations. Six physiologically realistic models were developed that consisted of three pharynx constriction levels (M1-3) and two uvula-flapping kinematics (K1-2). Direct numerical simulations (DNS) were performed to resolve spatial and temporal flow dynamics, and an immersed boundary method was used to approximate the uvula vibrations. Time-varying acoustic pressures at six points in the pharynx were analyzed using different algorithms in frequency- or frequency–time domains. Signature flow structures formed near the uvula for different uvula motions and in the pharynx for different pharyngeal constriction levels. The fast Fourier transform showed that the acoustic energy was mainly distributed in four peaks (flapping frequency and three harmonics) with descending magnitudes. Their amplitudes and distribution patterns differed among the six models but were not substantial. The continuous wavelet transforms showed clearly separated acoustic cycles (in both frequency and time) in the uvula-induced flows and revealed a cascading bifurcation pattern in the input–output semblance map. Specifically, the multifractal spectrum was sensitive to uvula flapping kinematics but not pharynx constrictions. By contrast, the input–output cross-correlation and Hilbert phase space showed high sensitivity to pharynx constrictions but low sensitivity to uvula kinematics. The frequency–time analyses of DNS-predicted pressures offered insight into the acoustics signals that were not apparent in original signals and could be used individually or in combination in diagnosis or treatment planning for snoring/OSA patients.
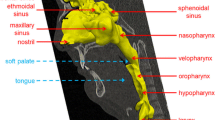
Graphic abstract














Similar content being viewed by others
Availability of data and materials
The DNS simulation results and MATLAB analysis codes are available upon request.
References
Huang, Y., White, D.P., Malhotra, A.: Use of computational modeling to predict responses to upper airway surgery in obstructive sleep apnea. Laryngoscope 117, 648–653 (2007)
Aragon, S.B.: Surgical management for snoring and sleep apnea. Dent. Clin. North Am. 45, 867–879 (2001)
Key, A.P.F., Molfese, D.L., O’Brien, L., Gozal, D.: Sleep-disordered breathing affects auditory processing in 5-7-year-old children: evidence from brain recordings. Dev. Neuropsychol. 34, 615–628 (2009)
Bonsignore, M.R., Baiamonte, P., Mazzuca, E., Castrogiovanni, A., Marrone, O.: Obstructive sleep apnea and comorbidities: a dangerous liaison. Multidiscip. Respir. Med. 14, 8–8 (2019)
Tietjens, J.R., Claman, D., Kezirian, E.J., De Marco, T., Mirzayan, A., et al.: Obstructive sleep apnea in cardiovascular disease: a review of the literature and proposed multidisciplinary clinical management strategy. J. Am. Heart Assoc. 8, e010440 (2019)
Touboul, P.J., Grobbee, D.E., den Ruijter, H.: Assessment of subclinical atherosclerosis by carotid intima media thickness: technical issues. Eur. J. Prev. Cardiol. 19, 18–24 (2012)
Dalmasso, F., Prota, R.: Snoring: analysis, measurement, clinical implications and applications. Eur. Respir. J. 9, 146–159 (1996)
Young, T., Palta, M., Dempsey, J., Skatrud, J., Weber, S., et al.: The occurrence of sleep-disordered breathing among middle-aged adults. N. Engl. J. Med. 328, 1230–1235 (1993)
Lindberg, E., Elmasry, A., Gislason, T., Janson, C., Bengtsson, H., et al.: Evolution of sleep apnea syndrome in sleepy snorers: a population-based prospective study. Am. J. Respir. Crit. Care Med. 159, 2024–2027 (1999)
Punjabi, N.M.: The epidemiology of adult obstructive sleep apnea. Proc. Am. Thorac. Soc. 5, 136–143 (2008)
Subramani, Y., Singh, M., Wong, J., Kushida, C.A., Malhotra, A., et al.: Understanding phenotypes of obstructive sleep apnea: applications in anesthesia, srgery, and prioperative mdicine. Anesth. Analg. 124, 179–191 (2017)
Osman, A.M., Carter, S.G., Carberry, J.C., Eckert, D.J.: Obstructive sleep apnea: current perspectives. Nat. Sci. Sleep. 10, 21–34 (2018)
Akhter, S., Abeyratne, U.R., Swarnkar, V., Hukins, C.: Snore sound analysis can detect the presence of obstructive sleep apnea specific to NREM or REM sleep. J. Clin. Sleep Med. 14, 991–1003 (2018)
Ramar, K., Dort, L.C., Katz, S.G., Lettieri, C.J., Harrod, C.G., et al.: Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J. Clin. Sleep Med. 11, 773–827 (2015)
Wang, J., Xi, J., Han, P., Wongwiset, N., Pontius, J., et al.: Computational analysis of a flapping uvula on aerodynamics and pharyngeal wall collapsibility in sleep apnea. J. Biomech. 94, 88–98 (2019)
Xi, J., Si, X., Kim, J., Su, G., Dong, H.: Modeling the pharyngeal anatomical effects on breathing resistance and aerodynamically generated sound. Med. Biol. Eng. Comput. 52, 567–577 (2014)
Xi, J., Wang, Z., Talaat, K., Glide-Hurst, C., Dong, H.J.S., et al.: Numerical study of dynamic glottis and tidal breathing on respiratory sounds in a human upper airway model. Sleep Breath. 22, 463–479 (2018)
Xi, J., April Si, X., Dong, H., Zhong, H.: Effects of glottis motion on airflow and energy expenditure in a human upper airway model. Eur. J. Mech. B. Fluids 72, 23–37 (2018)
Zinchuk, A., Yaggi, H.K.: Phenotypic subtypes of OSA: a challenge and opportunity for precision medicine. Chest 157, 403–420 (2020)
Naughton, M.T.: Loop gain in apnea: Gaining control or controlling the gain? Am. J. Respir. Crit. Care Med. 181, 103–105 (2010)
Xi, J., Talaat, M., Si, X.A., Dong, H.: Flow dynamics and acoustics from glottal vibrations at different frequencies. Acoustics 4, 1939796 (2022)
Messineo, L., Taranto-Montemurro, L., Azarbarzin, A., Oliveira Marques, M.D., Calianese, N., et al.: Breath-holding as a means to estimate the loop gain contribution to obstructive sleep apnoea. J. Physiol. 596, 4043–4056 (2018)
Gottlieb, D.J., Punjabi, N.M.: Diagnosis and management of obstructive sleep apnea: a review. JAMA 323, 1389–1400 (2020)
Kim, H.-H., Rakibuzzaman, M., Suh, S.-H., Kim, H.-J., Choi, J.-Y., et al.: A study of fluid dynamics parameters for prediction of obstructive sleep apnea. J. Mech. Sci. Tech. 32, 1079–1085 (2018)
Wakayama, T., Suzuki, M., Tanuma, T.: Effect of nasal obstruction on continuous positive airway pressure treatment: computational fluid dynamics analyses. PLoS ONE 11, e0150951 (2016)
Mihaescu, M., Murugappan, S., Gutmark, E., Donnelly, L.F., Kalra, M.: Computational modeling of upper airway before and after adenotonsillectomy for obstructive sleep apnea. Laryngoscope 118, 360–362 (2008)
Sittitavornwong, S., Waite, P., Shih, A., Cheng, G., Koomullil, R., et al.: Computational fluid dynamic analysis of the posterior airway space after maxillomandibular advancement for obstructive sleep apnea syndrome. J. Oral. Maxillofac. Surg. 71, 1397–405 (2013)
Taherian, S., Rahai, H., Lopez, S., Shin, J., Jafari, B.: Evaluation of human obstructive sleep apnea using computational fluid dynamics. Commun. Biol. 2, 423 (2019)
Back, G.W., Nadig, S., Uppal, S., Coatesworth, A.P.: Why do we have a uvula?: literature review and a new theory. Clin. Otolaryngol. Allied Sci. 29, 689–693 (2004)
Xi, J., Wang, J., Si, X.A., Zheng, S., Donepudi, R., et al.: Extracting signature responses from respiratory flows: low-dimensional analyses on Direct Numerical Simulation-predicted wakes of a flapping uvula. Int. J. Numer. Method Biomed. Eng. 36, e3406 (2020)
Clark, A., Newman, S., Dasovich, N.: Mouth and oropharyngeal deposition of pharmaceutical aerosols. J. Aerosol Med. 11, S116–S120 (1998)
Borojeni, A.A.T., Garcia, G.J.M., Moghaddam, M.G., Frank-Ito, D.O., Kimbell, J.S., et al.: Normative ranges of nasal airflow variables in healthy adults. Int. J. Comput. Assist. Radiol. Surg. 15, 87–98 (2020)
Mittal, R., Dong, H., Bozkurttas, M., Najjar, F.M., Vargas, A., et al.: A versatile sharp interface immersed boundary method for incompressible flows with complex boundaries. J. Comput. Phys. 227, 4825–4852 (2008)
Wang, J., Wainwright, D.K., Lindengren, R.E., Lauder, G.V., Dong, H.: Tuna locomotion: a computational hydrodynamic analysis of finlet function. J. R. Soc. Interface 17, 20190590 (2020)
Li, C., Dong, H., Liu, G.: Effects of a dynamic trailing-edge flap on the aerodynamic performance and flow structures in hovering flight. J. Fluid Struct. 58, 49–65 (2015)
Wang, J., Ren, Y., Li, C., Dong, H.: Computational investigation of wing-body interaction and its lift enhancement effect in hummingbird forward flight. Bioinspir. Biomim. 14, 046010 (2019)
Ren, Y., Dong, H., Deng, X., Tobalske, B.: Turning on a dime: asymmetric vortex formation in hummingbird maneuvering flight. Phys. Rev. Fluids. 1, 050511 (2016)
Liu, G., Dong, H., Li, C.: Vortex dynamics and new lift enhancement mechanism of wing-body interaction in insect forward flight. J. Fluid Mech. 795, 634–651 (2016)
Wan, H., Dong, H., Gai, K.: Computational investigation of cicada aerodynamics in forward flight. J. R. Soc. Interface 12, 20141116 (2015)
Dong, H., Mittal, R., Najjar, F.M.: Wake topology and hydrodynamic performance of low-aspect-ratio flapping foils. J. Fluid Mech. 566, 309–343 (2006)
Hekmati, A., Ricot, D., Druault, P.: About the convergence of POD and EPOD modes computed from CFD simulation. Comput. Fluids 50, 60–71 (2011)
Hunt, J., Wray, A., Moin, P.: Eddies, streams, and convergence zones in turbulent flows. Studying Turbulence Using Numerical Simulation Databases, pp. 193–208 (1988)
Grossmann, A., Morlet, J.: Decomposition of hardy functions into square integrable wavelets of constant shape. SIAM J. Math. Anal. 15, 723–736 (1984)
Subbu, A., Ray, A. Space partitioning via Hilbert transform for symbolic time series analysis (2008)
Jubran, B.A., Hamdan, M.N., Shabanneh, N.H., Szepessy, S.: Wavelet and chaos analysis of irregularities of vortex shedding. Mech. Res. Commun. 25, 583–591 (1998)
Oczeretko, E., Swiatecka, J., Kitlas, A., Laudanski, T., Pierzynski, P.: Visualization of synchronization of the uterine contraction signals: running cross-correlation and wavelet running cross-correlation methods. Med. Eng. Phys. 28, 75–81 (2006)
Elghobashi, S.: Direct numerical simulation of turbulent flows laden with droplets or bubbles. Annu. Rev. Fluid Mech. 51, 217–244 (2019)
Xi, J., Si, X.A., Kim, J., Mckee, E., Lin, E.-B.: Exhaled aerosol pattern discloses lung structural abnormality: a sensitivity study using computational modeling and fractal analysis. PLoS ONE 9, e104682 (2014)
Calderón-Díaz, M., Ulloa-Jiménez, R., Saavedra, C., Salas, R.: Wavelet-based semblance analysis to determine muscle synergy for different handstand postures of Chilean circus athletes. Comput. Methods Biomech. Biomed. Eng. 24, 1053–1063 (2021)
Pickering, D.N., Beardsmore, C.S.: Nasal flow limitation in children. Pediatr. Pulmonol. 27, 32–36 (1999)
Ohki, M., Ogoshi, T., Yuasa, T., Kawano, K., Kawano, M.: Extended observation of the nasal cycle using a portable rhinoflowmeter. J. Otolaryngol. 34, 346–349 (2005)
Xi, J., Kim, J., Si, X.A.: Effects of nostril orientation on airflow dynamics, heat exchange, and particle depositions in human noses. Eur. J. Mech. B. Fluids 55, 215–228 (2016)
Xi, J., Yuan, J.E., Yang, M., Si, X., Zhou, Y., et al.: Parametric study on mouth-throat geometrical factors on deposition of orally inhaled aerosols. J. Aerosol. Sci. 99, 94–106 (2016)
Zhou, Y., Guo, M., Xi, J., Irshad, H., Cheng, Y.S.: Nasal deposition in infants and children. J. Aerosol. Med. Pulm. Drug Deliv. 27, 110–116 (2014)
Khosla, S., Murugappan, S., Lakhamraju, R., Gutmark, E.: Using particle imaging velocimetry to measure anterior-posterior velocity gradients in the excised canine larynx model. Ann. Otol. Rhinol. Laryngol. 117, 134–144 (2008)
Saha, S., Moussavi, Z., Hadi, P., Bradley, T.D., Yadollahi, A.: Effects of increased pharyngeal tissue mass due to fluid accumulation in the neck on the acoustic features of snoring sounds in men. J. Clin. Sleep Med. JCSM Off. Publ. Am. Acad. Sleep Med. 14, 1653–1660 (2018)
Pasterkamp, H., Kraman, S.S., Wodicka, G.R.: Respiratory sounds: advances beyond the stethoscope. Am. J. Respir. Crit. Care Med. 156, 974–987 (1997)
El Taoum, K.K., Xi, J., Kim, J., Berlinski, A.: In vitro evaluation of aerosols delivered via the nasal route. Respir. Care 60, 1015–1025 (2015)
Xi, J., Si, X., Zhou, Y., Kim, J., Berlinski, A.: Growth of nasal and laryngeal airways in children: implications in breathing and inhaled aerosol dynamics. Respir. Care 59, 263–273 (2014)
Xi, J., Kim, J., Si, X.A., Corley, R.A., Zhou, Y.: Modeling of inertial deposition in scaled models of rat and human nasal airways: towards in vitro regional dosimetry in small animals. J. Aerosol Sci. 99, 78–93 (2016)
Xi, J., Si, X.A., Kim, J., Zhang, Y., Jacob, R.E., et al.: Anatomical details of the rabbit nasal passages and their implications in breathing, air conditioning, and olfaction. Anat. Rec. 299, 853–868 (2016)
Patel, J.A., Ray, B.J., Fernandez-Salvador, C., Gouveia, C., Zaghi, S., et al.: Neuromuscular function of the soft palate and uvula in snoring and obstructive sleep apnea: a systematic review. Am. J. Otolaryngol. 39, 327–337 (2018)
Pirnar, J., Dolenc-Grošelj, L., Fajdiga, I., Žun, I.: Computational fluid-structure interaction simulation of airflow in the human upper airway. J. Biomech. 48, 3685–3691 (2015)
Zörner, S., Kaltenbacher, M., Döllinger, M.: Investigation of prescribed movement in fluid-structure interaction simulation for the human phonation process. Comput. Fluids 86, 133–140 (2013)
Yang, J., Wang, X., Krane, M., Zhang, L.T.: Fully-coupled aeroelastic simulation with fluid compressibility: for application to vocal fold vibration. Comput. Methods Appl. Mech. Eng. 315, 584–606 (2017)
Mittal, R., Zheng, X., Bhardwaj, R., Seo, J.H., Xue, Q., et al.: Toward a simulation-based tool for the treatment of vocal fold paralysis. Front. Physiol. 2, 19 (2011)
Luo, H., Mittal, R., Bielamowicz, S.A.: Analysis of flow-structure interaction in the larynx during phonation using an immersed-boundary method. J. Acoust. Soc. Am. 126, 816–824 (2009)
Funding
This study was funded by NSF CBET-1605232 (H.D.) and NSF Grant CBET 2001090 (J.X.).
Author information
Authors and Affiliations
Contributions
JX and HD designed the study, JW and HD conducted the computational simulations and prepared Figs. 1, 2 and 3, XS and JX conducted the theoretical analyses and prepared Figs. 4, 5, 6, 7, 8, 9, 10, 11, 12 and 13, and JX and XS wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The author declares no conflicts of interest, financial or otherwise.
Additional information
Communicated by Outi Tammisola.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xi, J., Wang, J., Si, X.A. et al. Direct numerical simulations and flow-pressure acoustic analyses of flapping-uvula-induced flow evolutions within normal and constricted pharynx. Theor. Comput. Fluid Dyn. 37, 131–149 (2023). https://doi.org/10.1007/s00162-023-00638-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00162-023-00638-1