Abstract
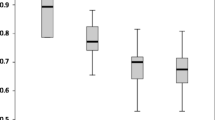
The aim of the present study was to differentiate acute rejection, chronic rejection, and tacrolimus nephrotoxicity with color and power Doppler imaging of renal transplants. One hundred examinations were obtained from 45 patients. Pulsatility and resistive indices were calculated from color Doppler images. The grade of renal vascularization was quantified using computer-assisted pixel analysis in a rectangular region-of-interest. The percentage of vessel-covered renal parenchyma (POV) was calculated using a histogram that discriminated renal vessels from renal parenchyma via power Doppler images. Furthermore, the distance from the most peripherally located vessels to the renal capsule (PVD) was measured. A reduced POV K 55 % proved to be the best discriminator when chronic rejection was suspected (sensitivity 79 %, specificity 87 %). Tacrolimus nephrotoxicity showed not only a moderate elevation of the Doppler signal but also an increased PVD L 3.9 mm and a normal POV. We conclude that the evaluation of renal vessels by power Doppler images improves diagnostic accuracy for patients with renal allografts.
Similar content being viewed by others
Author information
Authors and Affiliations
Additional information
Received: 22 June 1998 Received after revision: 29 September 1998 Accepted: 12 October 1998
About this article
Cite this article
Venz, S., Kahl, A., Hierholzer, J. et al. Contribution of color and power Doppler sonography to the differential diagnosis of acute and chronic rejection, and tacrolimus nephrotoxicity in renal allografts. Transpl Int 12, 127–134 (1999). https://doi.org/10.1007/s001470050197
Issue Date:
DOI: https://doi.org/10.1007/s001470050197