Abstract
Purpose
The aim of this study was to characterize differences in directives to limit treatments and discontinue invasive mechanical ventilation (IMV) in elderly (65–80 years) and very elderly (> 80 years) intensive care unit (ICU) patients.
Methods
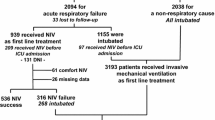
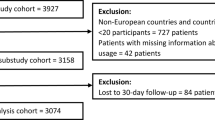
We prospectively described new written orders to limit treatments, IMV discontinuation strategies [direct extubation, direct tracheostomy, spontaneous breathing trial (SBT), noninvasive ventilation (NIV) use], and associations between initial failed SBT and outcomes in 142 ICUs from 6 regions (Canada, India, United Kingdom, Europe, Australia/New Zealand, United States).
Results
We evaluated 788 (586 elderly; 202 very elderly) patients. Very elderly (vs. elderly) patients had similar withdrawal orders but significantly more withholding orders, especially cardiopulmonary resuscitation and dialysis, after ICU admission [67 (33.2%) vs. 128 (21.9%); p = 0.002]. Orders to withhold reintubation were written sooner in very elderly (vs. elderly) patients [4 (2–8) vs. 7 (4–13) days, p = 0.02]. Very elderly and elderly patients had similar rates of direct extubation [39 (19.3%) vs. 113 (19.3%)], direct tracheostomy [10 (5%) vs. 40 (6.8%)], initial SBT [105 (52%) vs. 302 (51.5%)] and initial successful SBT [84 (80%) vs. 245 (81.1%)]. Very elderly patients experienced similar ICU outcomes (mortality, length of stay, duration of ventilation) but higher hospital mortality [26 (12.9%) vs. 38 (6.5%)]. Direct tracheostomy and initial failed SBT were associated with worse outcomes. Regional differences existed in withholding orders at ICU admission and in withholding and withdrawal orders after ICU admission.
Conclusions
Very elderly (vs. elderly) patients had more orders to withhold treatments after ICU admission and higher hospital mortality, but similar ICU outcomes and IMV discontinuation. Significant regional differences existed in withholding and withdrawal practices.


Similar content being viewed by others
Data availability
Written requests for de-identified data can be made to Dr. Burns.
References
Kontis V, Bennett JE, Mathers CD, Li G, Foreman K, Ezzati M (2017) Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet 389(10076):1323–1335
Boumendil A, Somme D, Garrouste-Orgeas M, Guidet B (2007) Should elderly patients be admitted to the intensive care unit? Intensive Care Med 33(7):1252. https://doi.org/10.1007/s00134-007-0621-3
Guidet B, de Lange DW, Flaatten H (2018) Should this elderly patient be admitted to the ICU? Intensive Care Med 44(11):1926–1928
Flaatten H, Garrouste-Orgeas M (2015) The very old ICU patient: a never-ending story. Intensive Care Med 41(11):1996–1998. https://doi.org/10.1007/s00134-015-4052-2
Guidet B, Leblanc G, Simon T, Woimant M, Quenot JP, Ganansia O et al (2017) Effect of systematic intensive care unit triage on long-term mortality among critically ill elderly patients in France: a randomized clinical trial. JAMA 318(15):1450–1459. https://doi.org/10.1001/jama.2017.13889
Needham D, Bronskill SE, Sibbald WJ, Pronovost PJ, Laupacis A (2004) Mechanical ventilation in Ontario, 1999–2000: incidence, survival and hospital bed utilization of noncardiac surgery adult patients. Crit Care Med 32:1504–1509
Needham D, Bronskill SE, Calinawan JR, Sibbald WJ, Pronovost PJ, Laupacis A (2005) Projected incidence of mechanical ventilation in Ontario to 2026: preparing for the aging baby boomers. Crit Care Med 33:574–579. https://doi.org/10.1097/01.ccm.0000155992.21174.31
van Heerden PV, Sviri S, Beil M, Szczeklik W, de Lange D, Jung C, Guidet B, Leaver S, Rhodes A, Boumendil A, Flaatten H (2020) The wave of very old people in the intensive care unit—a challenge in decision-making. J Crit Care 60:290–293. https://doi.org/10.1016/j.jcrc.2020.08.030
Boumendil A, Angus DC, Guitonneau AL, Menn AM, Ginsburg C, Takun K, Davido A, Masmoudi R, Doumenc B, Pateron D, Garrouste-Orgeas M, Somme D, Simon T, Aegerter P, Guidet B, On helalf of the ICU-CUB study group (2012) Variability of intensive care admission decisions for the very elderly. PLoS ONE 7:e34387. https://doi.org/10.1371/journal.pone.0034387
Leblanc G, Boumendil A, Guidet B (2017) Ten things to know about critically ill elderly patients. Intensive Care Med 43:217–219. https://doi.org/10.1007/s00134-016-4477-2
Ihra GC, Lehberger J, Hochrieser H, Bauer P, Schmutz R, Metnitz B, Metnitz PGH (2012) Development of demographics and outcome of very old critically ill patients admitted to intensive care units. Intensive Care Med 38(4):620–626. https://doi.org/10.1007/s00134-012-2474-7
Fuchs L, Chronaki CE, Park S, Novack V, Baumfeld Y, Scott D, McLennan S, Talmor D, Celi L (2012) ICU admission characteristics and mortality rates among elderly and very elderly patients. Intensive Care Med 38(10):1654–1661. https://doi.org/10.1007/s00134-012-2629-6
Somme D, Maillet JM, Gisselbrecht M, Novara A, Ract C, Fagon JY (2003) Critically ill old and the oldest-old patients in intensive care: short- and long-term outcomes. Intensive Care Med 29(12):2137–2143. https://doi.org/10.1007/s00134-003-1929-2
Ferrante LE, Pisani MA, Murphy TE, Gahbauer EA, Leo-Summers L, Gill TM (2015) Functional trajectories among older persons before and after critical illness. JAMA Intern Med 175:523–529. https://doi.org/10.1001/jamainternmed.2014.7889
Muessig JM, Nia AM, Masyuk M et al (2018) Clinical frailty scale (CFS) reliably stratifies octogenarians in German ICUs: a multicenter prospective cohort study. BMC Geriatr 18:162. https://doi.org/10.1186/s12877-018-0847-7
Canevelli M, Raganato R, Remiddi F, Quarata F, Valetta M, Bruno G, Cesari M (2020) Counting deficits or diseases? The agreement between frailty and multimorbidity in subjects with cognitive disturbances. Aging Clin Exp Res 32:179–182. https://doi.org/10.1007/s40520-019-01161-2
Flaatten H, De Lange DW, Morandi A et al (2017) The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (≥ 80 years). Intensive Care Med 43:1820–1828. https://doi.org/10.1007/s00134-017-4940-8
Wermly B, Beil M, Bruno RR, Binnebössel S, Kelm M, Sigal S, van Heerden PV, Boumendil A, Artigas A, Cecconi M, Marsh B, Moreno R, Oeyen S, Pinto BB, Szczeklik W, Leaver S, Walther SM, Schefold JC, Joannidis M, Fjølner J, Zafeiridis T, de Lange D, Guidet B, Flaatten H, Jung C, VIP2 study group (2021) Provision of critical care for the elderly in Europe: a retrospective comparison of national healthcare frameworks in intensive care units. BMJ Open 11(6):e046909
Vallet H, Schwartz GL, Flaatten H, de Lange DW, Guidet B, Deschartres A (2021) Mortality of older patients admitted to an ICU: a systematic review. Crit Care Med 49:324–334. https://doi.org/10.1097/CCM.0000000000004772
Cook D, Rocker G, Marshall J, Sjokvist P, Dodek P, Griffith L et al (2003) Withdrawal of mechanical ventilation in anticipation of death in the intensive care unit. N Engl J Med 349:1123–1132. https://doi.org/10.1056/NEJMoa030083
Cheng AC, Liao KM, Ho CH, Lai CC, Chao CM, Chiu CC, Chiang SR, Cheng KC, Chen CM (2020) The prognosis in extremely elderly patients receiving orotracheal intubation and mechanical ventilation after planned extubation. Medicine (Baltimore) 99(38):e21970. https://doi.org/10.1097/MD.0000000000021970
Esteban A, Anzueto A, Frutos-Vivar F, Alia I, Ely EW, Brochard L, Stewart TE, Apezteguia C, Tobin MJ, Nightingale P, Matamis D, Pimental J, Abroug F (2004) Outcome of older patients receiving mechanical ventilation. Intenive Care Med 30:639–646. https://doi.org/10.1007/s00134-004-2160-5
Burns KEA, Rizvi L, Meade MO, Dodek PM, Epstein SK, Slutsky A, Jones A, Villar J, Kapadia FN, Gattas D, Lellouche F, Cook DJ, Canadian Critical Care Trials Group (2018) Practices in end-of-life care and in discontinuing mechanical ventilation in elderly critically ill patients: a nested study within an international observational study. Intensive Care Med Exp 6(Suppl 2):1035
Burns KEA, Rizvi L, Cook DJ, Lebovic G, Dodek P, Villar J, Slutsky AS, Jones A, Kapadia FN, Gattas DJ, Epstein SK, Pelosi P, Kefala K, Meade MO, For the Canadian Critical Care Trials Group (2021) Ventilator weaning and discontinuation practices for critically ill adults. JAMA 325(12):1173–1184. https://doi.org/10.1001/jama.2021.2384
Vincent JL, de Mendonca A, Cantraine F, Moreno R, Takala J, Suter PM, Sprung CL, Colardyn F, Blecher S (1998) Use of the SOFA score to assess the incidence of organ dysfunction failure in intensive care units:results of a multicenter, prospective study. Crit Care Med 26(11):1793–1800. https://doi.org/10.1097/00003246-199811000-00016
Prendergast TJ, Claessens MT, Luce JM (1998) A national survey of end-of-life care for critically ill patients. Am J Respir Crit Care Med 158:1163–1167. https://doi.org/10.1164/ajrccm.158.4.9801108
Eidelman LA, Jakobson DJ, Pizov R, Geber D, Leibovitz L, Sprung CL (1998) Foregoing life-sustaining treatment in an Israeli ICU. Intensive Care Med 24:162–166. https://doi.org/10.1007/s001340050539
Holzapfel L, Demingeon G, Piralla B, Biot L, Nallet B (2002) A four-step protocol for limitation of treatment in terminal care. An observational study in 475 intensive care unit patients. Intensive Care Med 28:1309–1315. https://doi.org/10.1007/s00134-002-1370-y
Winter B, Cohen S (1999) ABC of intensive care. Withdrawal of treatment. BMJ 319:306–308. https://doi.org/10.1136/bmj.319.7205.306
Buckley TA, Joynt GM, Tan PY, Cheng CA, Yap FH (2004) Limitation of life support: frequency and practice in a Hong Kong intensive care unit. Crit Care Med 32:415–420. https://doi.org/10.1097/01.CCM.0000110675.34569.A9
Flaatten H, Guidet B, de Lange DW, Beil M, Leaver SK, Fjølner J, van Heerden PV, Sigal S, Szczeklik W, Jung C (2002) The importance of revealing data on limitation of life sustaining therapy in critical ill elderly Covid-19 patients. J Crit Care 67:147–148. https://doi.org/10.1016/j.jcrc.2021.10.024
Heyland D, Cook D, Bagshaw SM, Garland A, Stelfox HT, Mehta S, Dodek P, Kutsogiannis J, Burns K, Muscedere J, Turgeon AF, Fowler R, Jiang X, Day AG, For the Canadian Critical Care Trials Group and the Canadian Researchers At the End of Life Network (2015) The very elderly admitted to the ICU: a quality finish? Crit Care Med 43:1352–1360. https://doi.org/10.1097/CCM.0000000000001024
Melltorp G, Nilstun T (1997) The difference between withholding and withdrawing life-sustaining treatment. Intensive Care Med 23:1264–1267. https://doi.org/10.1007/s001340050496
Levin PD, Sprung CL (2005) Withdrawing and withholding life sustaining therapies are not the same. Crit Care 9:230–232. https://doi.org/10.1186/cc3487
Phua J, Joynt GM, Nishimura M, Deng Y, Myatra SN, Chan YH, Binh NG, Tan CC, Faruq MO, Arabi YM, Wahjuprajitno B, Liu SF, Hashemian SMR, Kashif W, Staworn D, Palo JE, Koh Y, For the ACME Study Investigators and the Asian Critical Care Trials Group (2015) Withholding and withdrawal of life-sustaining treatments in intensive care units in Asia. JAMA Internal Med 175(3):363–371. https://doi.org/10.1001/jamainternmed.2014.7386
Øystein UL (2019) Withholding and withdrawing life-sustaining treatment: ethically equivalent? Am J Bioeth 19(3):10–20. https://doi.org/10.1080/15265161.2018.1561961
Cook DJ, Rocker G, Giacomini M, Sinuff T, Heyland D (2006) Understanding and changing attitudes towards withdrawal and withholding life support in the intensive care unit. Crit Care Med 34(11):S317-323. https://doi.org/10.1097/01.CCM.0000237042.11330.A9
Wilkinson D, Butcherine E, Savulescu J (2019) Withdrawal aversion and the equivalence test. Am J Bioeth 19(3):21–28. https://doi.org/10.1080/15265161.2019.1574465
Truog RD, Campbell ML, Curtis JR, Haas CE, Luce JM, Rubenfeld GD, Rushton CH, Kaufmann DC (2008) Recommendations for end-of-life care in the intensive care unit: a consensus statement by the American College of Critical Care Medicine. Crit Care Med 36:953–963. https://doi.org/10.1097/CCM.0B013E3181659096
Avidan A, Sprung CL, Schefold JC, ETHICUS-2 Study Group et al (2021) Variations in end-of-life practices in intensive care units worldwide (Ethicus-2): a prospective observational study. Lancet Respir Med 9(10):1101–1110. https://doi.org/10.1016/S2213-2600(21)00261-7
Phua J, Joynt GM, Nishimura M, Deng Y, Myatra SN, Chan YH, Binh NG, Tan CC, Faruq MO, Arabi YM, Wahjuprajitno B, Liu SF, Hashemian SMR, Kashif W, Palo JE, Koh Y, ACME Study Investigators and the Asian Critical Care Trials Group (2016) Withholding and withdrawal of life-sustaining treatments in low-middle-income versus high-income Asian countries. Intensive Care Med 42:1118–1127. https://doi.org/10.1007/s00134-016-4347-y
Kapadia F, Singh M, Divatia J, Vaidyanathan P, Udwadia FE, Raisinghaney SJ, Limaye HS, Karnad DR (2005) Limitation and withdrawal of intensive therapy at the end of life: practices in intensive care units in Mumbai India. Crit Care Med 33(6):1272–1275. https://doi.org/10.1097/01.ccm.0000165557.02879.29
Lobo SM, De Simoni FHB, Jakob SM (2017) Decision-making on withdrawing or withholding life supportin the ICU: a world-wide perspective. Chest 152:321–329. https://doi.org/10.1016/j.chest.2017.04.176
Bulow HH, Sprung CL, Reinhart K, Prayag S, Du B, Armaganidis A, Abroug F, Levy MM (2008) The worlds’ major religions’ points of view on end-of-life decision in the intensive care unit. Intensive Care Med 34:423–430. https://doi.org/10.1007/s00134-007-0973-8
Wong WT, Phua JT, Joynt GM (2018) Worldwide end-of-life practice for patients in ICUs. Curr Opin Anesthesiol 31:172–178. https://doi.org/10.1097/ACO.0000000000000563
Ferrand E, Robert R, Ingrand P, Lemaire F (2001) Withholding and withdrawal of life support in intensive care units in France: a prospective survey. French Lataria Group. Lancet 347:9–14. https://doi.org/10.1016/s0140-6736(00)03564-9
Ely EW, Evans GW, Haponik EF (1999) Mechanical ventilation in a cohort of elderly patients admitted to an intensive care unit. Ann Intern Med 131:96–104. https://doi.org/10.7326/0003-4819-131-2-199907200-00004
Acknowledgements
We thank the members of the Canadian Critical Care Trials Group (CCCTG) for their contributions to the study design and guidance during study implementation. We thank the site investigators and research personnel who participated in the Ventilator Weaning and Discontinuation Practices for Critically Ill Patients study.
Funding
This study was funded by a peer-reviewed grant from the Canadian Frailty Network. The parent study was investigator-initiated and peer-review funded [CIHR-industry partnered grant (CIHR, Fisher & Paykel, Covidien, and GE Healthcare Ltd)]. KEAB currently holds a Mid-Career Physician Services Incorporated Award. DJC holds a Canada Research Chair in Knowledge Translation. JV received grants from CIBER de Enfermedades Respiratorias, Madrid, Spain (CB06/06/1088), and from Fundación Canaria Instituto de Investigación Sanitaria de Canarias, Spain (PIFIISC21-36).
Author information
Authors and Affiliations
Consortia
Contributions
Concept and design: KEAB, DJC, PD, JV, SKE, PP and MOM. Acquisition, analysis, or interpretation of data: KEAB, DJC, KX, JV, AJ, FNK, DJG, SKE, KK and MOM. Drafting of the manuscript: KEAB and JV. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: KX. Obtained funding: KEAB and MOM. Administrative, technical, or material support: KEAB, DJC, AJ and SKE. Supervision: KEAB, JV and PP. Other—coordinated UK contribution: AJ and KK. Other—coordinated India contribution: FNK. Other—coordinated Europe contribution: JV and PP. Other—coordinated Aus/NZ contribution: DJG. Other – coordinated USA contribution: SKE.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare.
Guarantor
KEAB and KX had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Role of the funder/sponsor
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Burns, K.E.A., Cook, D.J., Xu, K. et al. Differences in directives to limit treatment and discontinue mechanical ventilation between elderly and very elderly patients: a substudy of a multinational observational study. Intensive Care Med 49, 1181–1190 (2023). https://doi.org/10.1007/s00134-023-07188-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-023-07188-4