Abstract
With the expanding use of molecular assays, viral pathogens are increasingly recognized among critically ill adult patients with community-acquired severe respiratory illness; studies have detected respiratory viral infections (RVIs) in 17–53% of such patients. In addition, novel pathogens including zoonotic coronaviruses like the agents causing Severe Acute Respiratory Syndrome (SARS), Middle East Respiratory Syndrome (MERS) and the 2019 novel coronavirus (2019 nCoV) are still being identified. Patients with severe RVIs requiring ICU care present typically with hypoxemic respiratory failure. Oseltamivir is the most widely used neuraminidase inhibitor for treatment of influenza; data suggest that early use is associated with reduced mortality in critically ill patients with influenza. At present, there are no antiviral therapies of proven efficacy for other severe RVIs. Several adjunctive pharmacologic interventions have been studied for their immunomodulatory effects, including macrolides, corticosteroids, cyclooxygenase-2 inhibitors, sirolimus, statins, anti-influenza immune plasma, and vitamin C, but none is recommended at present in severe RVIs. Evidence-based supportive care is the mainstay for management of severe respiratory viral infection. Non-invasive ventilation in patients with severe RVI causing acute hypoxemic respiratory failure and pneumonia is associated with a high likelihood of transition to invasive ventilation. Limited existing knowledge highlights the need for data regarding supportive care and adjunctive pharmacologic therapy that is specific for critically ill patients with severe RVI. There is a need for more pragmatic and efficient designs to test different therapeutics both individually and in combination.
Similar content being viewed by others
Evidence-based supportive care is the mainstay for management of severe respiratory viral infection. Early treatment with neuraminidase inhibitors is associated with reduced mortality in severe influenza. There is a need for pragmatic and efficient trial designs, to test a variety of investigational therapeutics, individually and in combination. |
Introduction
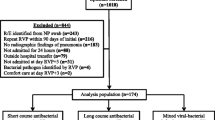
With the expanding use of molecular assays, viral pathogens are increasingly detected among critically ill adult patients with respiratory illness; studies have reported a prevalence between 17% and 53% of patients (Table 1), depending on study design, sample type, duration of illness, and assay methods. Common viruses that can cause severe respiratory viral infections (RVIs) include influenza A and B viruses, picornaviruses (rhinovirus, enterovirus [e.g., enterovirus D68]), human coronaviruses (229E, NL63, OC43, HKU1), respiratory syncytial virus (RSV), human metapneumovirus, parainfluenza virus, and adenovirus (Tables 1 and 2). Novel pathogens including zoonotic coronaviruses like the agents causing Severe Acute Respiratory Syndrome (SARS), Middle East Respiratory Syndrome (MERS) and the 2019 novel coronavirus (2019 nCoV) are still being identified (Table 2).
Establishing causation between viruses detected in respiratory specimens and the clinical illness is sometimes difficult, because (1) detection of some agents (e.g., picornaviruses) in the upper respiratory tract may indicate asymptomatic or mild infection, (2) upper respiratory tract samples may be negative despite positive lower respiratory tract ones, and (3) secondary bacterial and less often fungal infections are commonly co-identified [1]. However, it is generally believed that most respiratory viruses by themselves can cause severe illness, especially so in the elderly, persons with co-morbidities (particularly immunosuppression), and occasionally in previously healthy persons, in addition to predisposing to secondary infections [2].
The objective of this narrative review is to outline current knowledge on the management of adults requiring ICU admission for community-acquired severe acute respiratory infection (SARI) due to RVIs. This review focuses on viral pathogens transmitted via the respiratory route. Respiratory infections with other viral pathogens, such as cytomegalovirus and herpes simplex viruses, are not discussed in this review.
Antiviral therapy
Generally available antiviral agents for different RVIs are summarized in Table 3 [3]. Very few randomized-controlled trials have been completed in patients hospitalized for severe RVIs; recently completed trials of nitazoxanide in SARI patients and of the RSV inhibitor presatovir in adult RSV patients yielded negative results [4, 5]. Antiviral therapeutics for influenza have been studied most extensively and are discussed briefly below. A number of other antiviral agents for influenza, RSV, and other RVIs are advancing in clinical study [6]. Controlled studies of lopinavir/ritonavir combined with interferon-beta in hospitlized MERS patients (NCT02845843) and of lopinavir/ritonavir and interferon-alpha 2b in hospitalized 2019-nCoV patients (ChiCTR2000029308) are currently in progess.
Neuraminidase inhibitors
Among the neuraminidase inhibitors (NAIs), oral oseltamivir is the most widely available agent. In an individual participant data meta-analysis of hospitalized patients with influenza A(H1N1)pdm09 virus infection (n = 29 234 patients from 78 studies), NAI treatment (almost exclusively oseltamivir) was associated with a reduction in mortality compared with no treatment, including in the subgroup of ICU patients. Early treatment (within 2 days of symptom onset) was associated with a reduction in mortality compared with later treatment [7]. Observational data also indicate reduction in influenza A(H5N1)-associated mortality with timely oseltamivir treatment before the onset of respiratory failure [8]. The importance of timing of oseltamivir treatment has been demonstrated in an observational study of 1950 patients admitted to ICUs with influenza A(H1N1)pdm09, which showed a trend toward improved survival for those treated earliest [9]. Nevertheless, the Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA) recommends oseltamivir for all hospitalized patients with influenza, regardless of illness duration prior to hospitalization [10].
In observational studies of critically ill patients with influenza, higher compared to standard doses of oseltamivir did not demonstrate benefit [11,12,13]. An RCT of standard versus double-dose oseltamivir in hospitalized children and adults found no advantage with respect to virologic and clinical endpoints [14]. Additionally, a study demonstrated accumulation of oseltamivir in patients on both extracorporeal membrane oxygenation and continuous venovenous hemodiafiltration leading to 4-to 5-fold increase in plasma levels [15]. The IDSA recommends against the routine use of higher doses of US Food and Drug Administration-approved NAI drugs for the treatment of seasonal influenza [10].
Duration of treatment is traditionally 5 days, but treatment duration is often extended to 10 days for severely ill patients with ARDS or pneumonia or those who are immunocompromised [10]. This approach is supported by data showing slow influenza viral clearance from the lower respiratory tract in critically ill patients with influenza A(H1N1)pdm09 [16]. Of concern is the recent observation of emergence of oseltamivir resistance in 23% of 22 critically ill A(H1N1)pdm09 patients, and its association with persistent virus detection and much higher mortality [17].
Nebulized zanamivir solution has been administered to mechanically ventilated patients on compassionate use basis, but the commercial formulation contains lactose and should not be used for nebulization, because its use has been associated with blockage of the ventilator circuit.
Peramivir is the only intravenous influenza antiviral agent currently approved by the US Food and Drug Administration (FDA). Intravenous zanamivir has been recently approved by the European Medicines Agency (EMA) (Table 3). These agents appear to have comparable activity to oseltamivir in hospitalized influenza patients, although one RCT comparing two dose levels of intravenous zanamivir to oral oseltamivir found trends toward shorter illness duration in the subset of ICU patients given higher dose intravenous zanamivir [18]. One the other hand, one RCT failed to demonstrate a clinical benefit with intravenous peramivir in hospitalized patients with influenza [19]. Because its spectrum of activity includes most oseltamivir-resistant viruses, intravenous zanamivir is indicated for treatment of severe influenza A or B when the patient’s influenza virus is known or suspected to be resistant to anti-influenza antivirals other than zanamivir, and/or other antivirals, including inhaled zanamivir, are not suitable (Table 3).
Baloxavir
Two phase III trials in non-hospitalized patients with influenza found that single-dose baloxavir was superior to placebo in alleviating influenza symptoms, and was superior to both oseltamivir and placebo in reducing viral replication [20, 21]. Baloxavir is inhibitory for strains resistant to current agents. However, high frequencies of emergence of variants with reduced susceptibility have been observed during monotherapy. A double-blind RCT comparing oseltamivir to the combination of oseltamivir and baloxavir is currently in progress in hospitalized patients (NCT03684044). Data on baloxavir’s pharmacokinetics and optimal dose regimen in critical influenza illness leading to ICU admission are needed [20]. At present, baloxavir is approved in the US, Japan, and over ten other countries.
Adjunctive pharmacologic interventions
A wide variety of agents have been proposed for managing immunopathologic host responses that contribute to the pathogenesis of severe RVIs [6]. As summarized below, those that have progressed to clinical study include macrolides, corticosteroids, cyclo-oxygenase2 inhibitors, mTOR inhibitors like sirolimus, statins, and high-dose vitamin C. However, until further evidence becomes available, these agents should not be used for managing severe RVIs unless there is another indication or as part of a clinical trial.
Macrolides
Macrolide antibiotics, due to putative anti-inflammatory and possible antiviral effects, have been studied in patients with RVIs but with inconsistent results. In an open-label RCT of hospitalized patients with influenza (n = 107), early combination therapy with clarithromycin, naproxen, and oseltamivir was associated with reduced mortality and hospital length of stay compared to oseltamivir monotherapy [22]. On the other hand, in a multicenter observational study (n = 733), macrolides were not associated with improved survival in critically ill patients with influenza A(H1N1)pdm09 [23]. In patients with MERS (n = 349), macrolide therapy is not associated with a reduction in 90-day mortality or improvement in MERS-CoV RNA clearance [24]. A study of clarithromycin combined with the cyclooxygenase inhibitor flufenamic acid in hospitalized patients with influenza is underway (NCT03238612). In addition, macrolides are also examined in one of the domains of the REMAP-CAP trial (Randomized, Embedded, Multifactorial Adaptive Platform Trial for Community-Acquired Pneumonia, NCT02735707).
Corticosteroids
Data on the use of corticosteroids in severe RVIs are largely observational. Several studies demonstrated the association of corticosteroid use with mortality, bacterial and fungal infection and the emergence of antiviral resistance in influenza-associated pneumonia or ARDS [25]. A study (n = 607) that accounted for time-dependent patient-level confounders found no independent influence of corticosteroids on mortality of influenza [26]. The IDSA recommends against corticosteroid adjunctive therapy in patients with influenza unless clinically indicated for other reasons [10]. In a study of patients hospitalized with RSV (n = 50), corticosteroid therapy was not associated with significant differences in peak viral load, duration of RSV shedding, nasal cytokines, or lymphocyte subsets, although antibody responses to RSV were slightly blunted [27]. In one randomized-controlled trial that included 16 non-ICU SARS patients, “early” (< 7 days of illness) hydrocortisone therapy was associated with a higher subsequent plasma viral load [28]. In a study on MERS patients (n = 309), corticosteroid therapy was not associated with significant change in 90-day mortality after adjustment for time-varying confounders, but was associated with delayed MERS-CoV RNA clearance [29].
Cyclooxygenase-2 inhibitors
Cyclooxygenase-2 may modulate excessive pro-inflammatory responses in severe influenza [30]. In addition to the above study of naproxen–clarithromycin added to oseltamivir [23], preliminary results from a RCT (n = 120) showed that the combination of celecoxib-oseltamivir compared to oseltamivir alone reduced mortality and cytokine levels, although not viral titers, in hospitalized influenza A(H3N2) patients without increased adverse effects [31].
Sirolimus
Inhibitors of the mTOR pathway like sirolimus combined with oseltamivir have shown inconsistent effects in murine models of severe influenza [32, 33]. Sirolimus also can modulate inflammatory responses through its immunosuppressive properties [34]. In a small RCT (n = 28), treatment with sirolimus compared to no sirolimus in patients with influenza A(H1N1) pneumonia receiving invasive mechanical ventilation (in addition to oseltamivir and corticosteroids) resulted in improvement in hypoxia, multiple organ dysfunction and virus clearance, and in shorter duration of mechanical ventilation [34]. Further study of sirolimus without systemic corticosteroids is planned among patients hospitalized with influenza (NCT03901001).
Statins
Because of the putative anti-inflammatory effects, statins have been proposed as adjunctive therapy in influenza (NCT02056340), although large clinical trials in patients in ARDS have not demonstrated clinical benefit [35]. A secondary analysis of data from RCTs using latent class analysis suggested that patients with ARDS may be classified into hyper-inflammatory and hypo-inflammatory subphenotypes, and treatment with simvastatin compared to placebo was associated with improved survival in the hyper-inflammatory but not in the hypo-inflammatory subphenotype [36]. Further studies are needed to examine whether adjunctive pharmacologic interventions would be beneficial in targeted subphenotypes of severe RVI.
Immune therapy
Studies in which various antibody immunotherapies have been added to neuraminidase inhibitor treatment in hospitalized influenza patients have yielded inconsistent results. A small randomized-controlled trial (n = 35) demonstrated that treatment of severe influenza A(H1N1)pdm09 patients with hyperimmune globulin (H-IVIG) containing high titers of virus-specific neutralizing antibodies within 5 days of symptom onset was associated with a lower viral load and reduced mortality compared to low-titer IVIG [37]. Two recent phase III trials have been completed in seasonal influenza patients. The FLU-IVIG RCT found no overall effect of anti-influenza hyperimmune IVIG compared to placebo on the primary outcome measured by a six-point ordinal scale of clinical status on day 7, although antiviral and clinical benefits were noted in the subgroup of patients with influenza B virus infection [38]. The second trial of high-titer versus low-titer anti-influenza immune plasma was terminated for futility because of the lack of effect on the same primary outcome [39]. A placebo-controlled, randomized trial of the anti-hemagglutinin stem monoclonal antibody MHAA4549A did not demonstrate benefit over oseltamivir alone [6]. The results from these recent trials suggest that polyclonal antibody therapies may not significantly improve outcomes in severe seasonal influenza A, although their possible value in treating severe RVI by novel influenza strains remains to be determined.
Vitamin C
The recent CITRIS-ALI trial demonstrated that 96-h infusion of vitamin C compared with placebo in a relatively small number (n = 167) of patients with sepsis and ARDS did not improve the primary outcome of organ dysfunction scores or alter markers of inflammation and vascular injury. However, mortality, which was one of the forty-six pre-specified secondary endpoints, was significantly lower with vitamin C [40]. Results of other ongoing larger trials are awaited, and data on severe RVI are needed.
Antibacterial therapy
Co-infections with bacterial pathogens occur often with RVI. Co-infection with Staphylococcus aureus is common with influenza pneumonia and can be especially virulent [10]. The recent 2019 ATS/IDSA clinical practice guidelines recommend standard antibacterial therapy to be initially prescribed for adults with community-acquired pneumonia who test positive for influenza [10]. The guidelines provide details on when to consider empiric therapy for methicillin resistant Staphylococcus aureus and Pseudomonas aeruginosa and provide guidance for de-escalation of antibacterial therapy in patients with confirmed influenza [10]. Clinicians should be aware of the reports of invasive pulmonary aspergillosis in severely ill influenza patients especially those with underlying conditions or receiving corticosteroids, although up to 30% of patients with influenza-associated aspergillosis had been previously healthy [41].
Supportive care
Patients with severe RVI present typically with pneumonia, acute respiratory distress syndrome (ARDS), decompensated heart failure, or exacerbation of chronic lung disease; leading frequently to acute hypoxemic, and less commonly hypercapnic, respiratory failure. Except for several influenza and novel coronavirus studies noted below, most of the data regarding supportive care strategies come from studies that have not documented specific RVIs. In many ARDS trials, patients with pneumonia constituted a majority of enrolled patients; but detailed description of etiologic pathogens is often lacking. Given the high prevalence of viral pathogens as outlined earlier, it is likely that severe RVIs constitute a considerable proportion. There are general pathophysiologic and clinical similarities between ARDS and pneumonia caused by severe RVIs and those due to other pathogens or etiologies, and therefore, the extrapolation of findings from unselected populations to patients with severe RVIs can be justified in the absence of specific data. At the same time, there are important differences that may lead to heterogeneity in response to treatment.
Non-invasive ventilation
Data on non-invasive ventilation (NIV) in severe RVI are limited. In patients with severe RVI resulting in chronic obstructive pulmonary disease (COPD) exacerbations or cardiogenic pulmonary edema, NIV may be effective in reducing the need of endotracheal intubation and decreasing ventilator-associated complications and mortality [42].
However, NIV in patients with severe RVI causing acute hypoxemic respiratory failure and pneumonia is of uncertain benefit. Observational studies reported variable results for NIV in patients with severe influenza A(H1N1)pdm09 with some reporting NIV failure in up to 85% [43]. In one multicenter observational study of 1898 critically ill patients with acute hypoxemic respiratory failure due to influenza, 806 underwent initial NIV, and 56.8% of them required conversion to invasive ventilation. Patients with SOFA ≥ 5 had a higher risk of NIV failure. Similar to other studies, NIV failure was associated with increased ICU mortality compared with invasive mechanical ventilation [44].
Data from uncontrolled studies suggested that NIV might have been effective and safe in the management of some patients with SARS [45], while others highlighted concerns of increased SARS transmission risk to healthcare workers [46]. In a multicenter cohort of 302 MERS critically ill patients, NIV was used initially in 35% of patients, but the vast majority of them (92.4%) required conversion to invasive mechanical ventilation; however, NIV was not independently associated with 90-day mortality [47].
A recent single-center RCT in patients with unselected patients with ARDS (n = 83, 45% pneumonia) showed that treatment with helmet NIV resulted in significant reduction of intubation rates and in 90-day mortality [48]. Further studies in patients with severe RVI are needed, as helmet NIV may be more effective than traditional masks and may be associated with less risk of transmission due to aerosol generation.
Based on available evidence, NIV in severe RVI may be used in selected patients in early stages and milder forms of acute hypoxemic respiratory failure, excluding those in shock or multiorgan failure, with the recognition that for patients who do not show signs of early recovery, NIV may well delay but not avoid invasive ventilation [42].
High-flow nasal cannula
High-flow nasal cannula has emerged as an alternative to NIV to prevent intubation in patients with acute hypoxemic respiratory failure. In one trial (n = 310, 72% community-acquired pneumonia), treatment with high-flow oxygen, standard oxygen, or NIV did not result in significantly different intubation rates; however, there was a significant difference in favor of high-flow nasal cannula in 90-day mortality [49]. A small cohort of patients with severe RVI with influenza A(H1N1)pdm09 (n = 25) showed that high-flow nasal cannula was associated with avoidance of intubation in 45% of patients, although almost all patients with higher severity of illness and shock were eventually intubated [50].
Invasive ventilation
Based on current evidence, patients with ARDS due to severe RVI should be managed with lung-protective strategy with low tidal volumes (6 ml/kg predicted body weight) and plateau pressures < 30 to 35 cmH2O. In adults with acute lung injury or ARDS due to various causes, an individual patient data meta-analysis of 2299 patients from three trials (50% with pneumonia) found that higher positive end-expiratory pressure (PEEP) levels were associated with improved survival among the subgroup of patients with ARDS (defined by PaO2/FiO2 ≤ 200 mmHg) [51]. A recent RCT of over 1000 patients with moderate-to-severe ARDS (55% with pneumonia) demonstrated that prolonged and high-pressure recruitment maneuvers was associated with increased 28-day mortality [52]. Titration of PEEP to achieve optimal oxygenation, perhaps without aggressive recruitment maneuvers, remains a reasonable strategy for most patients.
High-frequency oscillatory ventilation (HFOV)
HFOV ventilates the lung with tidal volumes lower than anatomical dead space while achieving relatively high mean airway pressures [53]. In patients with influenza A(H1N1)pdm09 influenza, HFOV has been used as a rescue therapy for those not responding to conventional ventilation [53]. Two randomized clinical trials showed that HFOV in moderate-to-severe ARDS was not associated with improved outcomes compared to conventional ventilation [54, 55]. However, a meta-analysis of 1552 patients (55% with pneumonia) found that the HFOV treatment effect depended on baseline severity of hypoxemia, with harm among patients with mild-moderate ARDS but possibly decreased mortality in patients with very severe ARDS [56]. Therefore, while HFOV is not recommended for routine use in ARDS, there may still be a role as rescue therapy [53].
Prone positioning
A multicenter RCT (n = 474, 60% with pneumonia) demonstrated that early application of prone positioning (at least 16 h per session) in patients with severe ARDS (PaO2/FiO2 < 150 mmHg, with an FiO2 ≥ 0.6, PEEP of ≥ 5 cmH2O, and a tidal volume close to 6 ml/kg predicted body weight) resulted in decreased mortality [57]. Prone positioning in patients with avian A(H7N9) influenza-related severe ARDS has been associated with improved oxygenation, sustained after returning to a supine position, and with decreased carbon dioxide retention [58].
Neuromuscular blockers
In patients with severe ARDS, in one trial (n = 339, 38% community-acquired pneumonia), early administration of a neuromuscular blocking agent improved the adjusted 90-day survival and increased the time off the ventilator without increasing muscle weakness [59]. However, in a recent larger trial that enrolled patients with moderate-to-severe ARDS (n = 1006, 59% pneumonia), treated with a strategy involving high PEEP, there was no significant difference in mortality at 90 days between patients who received an early, continuous cisatracurium infusion and those who were treated with a usual-care approach with lighter sedation targets [60]. Specific data on neuromuscular blockade in severe RVI are lacking.
Extracorporeal membrane oxygenation (ECMO)
The latest RCT for ECMO (EOLIA) included 249 patients with severe ARDS, 18% with viral etiologies, and found that ECMO did not reduce mortality at day 60 [61]. Yet, a post hoc Bayesian analysis found that the interpretation of benefit versus no benefit in this trial is critically dependent upon the range of prior assumptions reflecting varying degrees of skepticism and enthusiasm of previous evidence for the benefit of ECMO—clinicians with more enthusiasm for the benefit of ECMO may be justified in considering it for certain patients [62].
Indeed, observational studies reported lower hospital mortality among patients with ARDS related to influenza A(H1N1)pdm09 with transfer to an ECMO center compared with matched non-ECMO-referred patients [63]. A case–control study also suggested survival benefit for ECMO in patients with severe MERS [64]. ECMO is likely to be associated with better outcomes when used among patients with limited organ failures and good premorbid functional status, and should be considered for patients who fail other evidence-based oxygenation strategies according to individual patient characteristics and a potential risk–benefit determination.
Cardiovascular management
Timely adequate fluid resuscitation is an essential element of the management of patients with severe RVI and shock. However, in those with ARDS (n = 1000, 47% pneumonia), a conservative strategy of fluid management improved lung function and shortened the duration of mechanical ventilation without increasing non-pulmonary-organ failures [65]. In addition, aggressive fluid administration may worsen ventricular function. This may be particularly relevant for patients with severe RVI. Myocardial involvement is not uncommon with severe influenza A or B virus infection, and multiple studies have shown an association between influenza and acute myocardial infection and myocarditis [66,67,68]. Echocardiographic findings often include right- and left-ventricular dysfunction [66]. Therefore, clinical assessment of fluid responsiveness is important along with quantification of right- and left-ventricular size and function using echocardiography and/or dynamic minimally invasive cardiovascular monitoring, if available. Myocarditis has associated with longer duration of vasoactive agents and mortality and may sometimes require ECMO or other types of supportive care [69, 70].
Infection prevention and control
Table 2 summarizes infection control precautions for different RVIs as recommended by the Centers for Disease Control and Prevention (please refer to Table 2 footnote for CDC references). In patients presenting with severe RVIs, contact plus droplet precautions are recommended; droplet precautions may be discontinued when adenovirus and influenza have been ruled out. For patients with a history of recent travel (10–21 days) to countries with active outbreaks of SARS, MERS, or avian influenza, airborne plus contact precautions and eye protection are recommended.
Aerosol-generating procedures, such as bronchoscopy, endotracheal intubation, and open suctioning of the respiratory tract, tracheotomy, manual ventilation before intubation, nebulizer treatment, high-flow nasal cannula, non-invasive ventilation, and chest compressions, have been implicated with transmission of infectious agents to healthcare personnel. However, these findings were identified from limited studies, mainly during the SARS outbreak [71]. Nevertheless, it is recommended during aerosol-generating procedures on patients with suspected or proven infections transmitted by aerosols (for example influenza, MERS, SARS) to wear a fit-tested N95 mask in addition to gloves, gown, and face/eye protection. Closed-circuit suctioning may reduce the exposure to aerosols. Performing these procedures in an airborne isolation room when feasible is recommended.
RCTs comparing N95 respirators to medical masks in health care personnel working in outpatient and ward settings have not shown significant differences in protection from laboratory-confirmed influenza or other RVIs [72, 73]. The relevance of these observations to the ICU setting is uncertain, given the frequent use of aerosol-generating procedures in critically ill patients. Cloth masks are clearly inferior to medical masks in protecting HCWs from RVIs [74]. Other aspects of prevention strategies to prevent transmission when caring for patients with severe RVIs include annual influenza vaccination of healthcare workers, adherence to standard precautions, including hand hygiene, during the care of any patient and appropriate management of ill healthcare workers (please refer to Table 2 footnote for CDC references). Recently, antiseptic hand rubbing using ethanol-based disinfectants (EBDs) was found to be less effective than hand washing with running water in inactivating influenza virus in undried mucus under experimental conditions; [75] also nonenveloped viruses like adenovirus which are not easily inactivated by EBDs. The implications of these observations for clinical practice remain to be determined but hand washing with soap and water or hand rubbing with EBD for longer than 30 s may be warranted.
Future directions for research
The Global Influenza Programme has published the updated WHO Public Health Research Agenda for Influenza, in which research priorities were identified for several domains including patient management [76]. Existing knowledge highlights the need for data regarding supportive care and adjunctive pharmacologic therapy that is specific for critically ill patients with severe RVI. Data on supportive management in resource-restricted settings are severely lacking. There is a need for more pragmatic and efficient designs to test antiviral therapeutics, individually and in combination in patients with severe RVI who are at increased risk for complications from both the disease and treatments. Adaptive randomized-controlled trial that tests several treatments, such as the REMAP-CAP trial (NCT02735707), may represent an efficient approach.
References
Karhu J, Ala-Kokko TI, Vuorinen T, Ohtonen P, Syrjala H (2014) Lower respiratory tract virus findings in mechanically ventilated patients with severe community-acquired pneumonia. Clin Infect Dis 59:62–70
Hasvold J, Sjoding M, Pohl K, Cooke C, Hyzy RC (2016) The role of human metapneumovirus in the critically ill adult patient. J Crit Care 31:233–237
Zumla A, Memish ZA, Maeurer M, Bates M, Mwaba P, Al-Tawfiq JA, Denning DW, Hayden FG, Hui DS (2014) Emerging novel and antimicrobial-resistant respiratory tract infections: new drug development and therapeutic options. Lancet Infect Dis 14:1136–1149
Hanfelt-Goade D, Maimon N, Nimer A, et al A phase 2b, randomized, double-blind, placebo-controlled trial of presatovir (GS-5806), a novel oral rsv fusion inhibitor, for the treatment of respiratory syncytial virus (RSV) in hospitalized adults American Thoracic Society 2018 international conference, San Diego, 2018: abstract A4457
Gamino-Arroyo AE, Guerrero ML, McCarthy S, Ramirez-Venegas A, Llamosas-Gallardo B, Galindo-Fraga A, Moreno-Espinosa S, Roldan-Aragon Y, Araujo-Melendez J, Hunsberger S, Ibarra-Gonzalez V, Martinez-Lopez J, Garcia-Andrade LA, Kapushoc H, Holley HP Jr, Smolskis MC, Ruiz-Palacios GM, Beigel JH, Mexico Emerging Infectious Diseases Clinical Research N (2019) Efficacy and safety of nitazoxanide in addition to standard of care for the treatment of severe acute respiratory illness. Clin Infect Dis 69:1903–1911
Beigel JH, Nam HH, Adams PL, Krafft A, Ince WL, El-Kamary SS, Sims AC (2019) Advances in respiratory virus therapeutics—a meeting report from the 6th isirv Antiviral Group conference. Antiviral Res 167:45–67
Muthuri SG, Venkatesan S, Myles PR, Leonardi-Bee J, Al Khuwaitir TS, Al Mamun A, Anovadiya AP, Azziz-Baumgartner E, Baez C, Bassetti M, Beovic B, Bertisch B, Bonmarin I, Booy R, Borja-Aburto VH, Burgmann H, Cao B, Carratala J, Denholm JT, Dominguez SR, Duarte PA, Dubnov-Raz G, Echavarria M, Fanella S, Gao Z, Gerardin P, Giannella M, Gubbels S, Herberg J, Iglesias AL, Hoger PH, Hu X, Islam QT, Jimenez MF, Kandeel A, Keijzers G, Khalili H, Knight M, Kudo K, Kusznierz G, Kuzman I, Kwan AM, Amine IL, Langenegger E, Lankarani KB, Leo YS, Linko R, Liu P, Madanat F, Mayo-Montero E, McGeer A, Memish Z, Metan G, Mickiene A, Mikic D, Mohn KG, Moradi A, Nymadawa P, Oliva ME, Ozkan M, Parekh D, Paul M, Polack FP, Rath BA, Rodriguez AH, Sarrouf EB, Seale AC, Sertogullarindan B, Siqueira MM, Skret-Magierlo J, Stephan F, Talarek E, Tang JW, To KK, Torres A, Torun SH, Tran D, Uyeki TM, Van Zwol A, Vaudry W, Vidmar T, Yokota RT, Zarogoulidis P, Investigators PC, Nguyen-Van-Tam JS (2014) Effectiveness of neuraminidase inhibitors in reducing mortality in patients admitted to hospital with influenza A H1N1pdm09 virus infection: a meta-analysis of individual participant data. Lancet Respir Med 2:395–404
Adisasmito W, Chan PK, Lee N, Oner AF, Gasimov V, Aghayev F, Zaman M, Bamgboye E, Dogan N, Coker R, Starzyk K, Dreyer NA, Toovey S (2010) Effectiveness of antiviral treatment in human influenza A(H5N1) infections: analysis of a Global Patient Registry. J Infect Dis 202:1154–1160
Louie JK, Yang S, Acosta M, Yen C, Samuel MC, Schechter R, Guevara H, Uyeki TM (2012) Treatment with neuraminidase inhibitors for critically ill patients with influenza A (H1N1)pdm09. Clin Infect Dis 55:1198–1204
Uyeki TM, Bernstein HH, Bradley JS, Englund JA, File TM, Fry AM, Gravenstein S, Hayden FG, Harper SA, Hirshon JM, Ison MG, Johnston BL, Knight SL, McGeer A, Riley LE, Wolfe CR, Alexander PE, Pavia AT (2019) Clinical practice guidelines by the infectious diseases society of America: 2018 update on diagnosis, treatment, chemoprophylaxis, and institutional outbreak management of seasonal influenzaa. Clin Infect Dis 68:895–902
Welch SC, Lam SW, Neuner EA, Bauer SR, Bass SN (2015) High-dose versus standard dose oseltamivir for treatment of severe influenza in adult intensive care unit patients. Intensive Care Med 41:1365–1366
Lee N, Hui DS, Zuo Z, Ngai KL, Lui GC, Wo SK, Tam WW, Chan MC, Wong BC, Wong RY, Choi KW, Sin WW, Lee EL, Tomlinson B, Hayden FG, Chan PK (2013) A prospective intervention study on higher-dose oseltamivir treatment in adults hospitalized with influenza a and B infections. Clin Infect Dis 57:1511–1519
Noel ZR, Bastin MLT, Montgomery AA, Flannery AH (2017) Comparison of high-dose versus standard dose oseltamivir in critically ill patients with influenza. J Intensive Care Med 32:574–577
South East Asia Infectious Disease Clinical Research N (2013) Effect of double dose oseltamivir on clinical and virological outcomes in children and adults admitted to hospital with severe influenza: double blind randomised controlled trial. BMJ 346:f3039
Lemaitre F, Luyt CE, Roullet-Renoleau F, Nieszkowska A, Zahr N, Corvol E, Fernandez C, Antignac M, Farinotti R, Combes A (2012) Impact of extracorporeal membrane oxygenation and continuous venovenous hemodiafiltration on the pharmacokinetics of oseltamivir carboxylate in critically ill patients with pandemic (H1N1) influenza. Ther Drug Monit 34:171–175
Lee N, Chan PK, Wong CK, Wong KT, Choi KW, Joynt GM, Lam P, Chan MC, Wong BC, Lui GC, Sin WW, Wong RY, Lam WY, Yeung AC, Leung TF, So HY, Yu AW, Sung JJ, Hui DS (2011) Viral clearance and inflammatory response patterns in adults hospitalized for pandemic 2009 influenza A(H1N1) virus pneumonia. Antivir Ther 16:237–247
Behillil S, May F, Fourati S, Luyt CE, Chicheportiche T, Sonneville R, Tandjaoui-Lambiotte Y, Roux D, Guerin L, Mayaux J, Maury E, Ferre A, Georger JF, Voiriot G, Enouf V, van der Werf S, Mekontso DA, de Prost N (2019) Oseltamivir resistance in severe influenza A(H1N1)pdm09 pneumonia and acute respiratory distress syndrome: a French multicenter observational cohort study. Clin Infect Dis. https://doi.org/10.1093/cid/ciz904
Marty FM, Vidal-Puigserver J, Clark C, Gupta SK, Merino E, Garot D, Chapman MJ, Jacobs F, Rodriguez-Noriega E, Husa P, Shortino D, Watson HA, Yates PJ, Peppercorn AF (2017) Intravenous zanamivir or oral oseltamivir for hospitalised patients with influenza: an international, randomised, double-blind, double-dummy, phase 3 trial. Lancet Respir Med 5:135–146
de Jong MD, Ison MG, Monto AS, Metev H, Clark C, O’Neil B, Elder J, McCullough A, Collis P, Sheridan WP (2014) Evaluation of intravenous peramivir for treatment of influenza in hospitalized patients. Clin Infect Dis 59:e172–e185
Hayden FG, Shindo N (2019) Influenza virus polymerase inhibitors in clinical development. Curr Opin Infect Diseases 32(2):176–186
Ison MG, Portsmouth S, Yoshida Y, Shishido T, Hayden F, Uehara T (2018) LB16. Phase 3 trial of baloxavir marboxil in high-risk influenza patients (CAPSTONE-2 study). Open Forum Infect Dis 5:S764–S765
Hung IFN, To KKW, Chan JFW, Cheng VCC, Liu KSH, Tam A, Chan TC, Zhang AJ, Li P, Wong TL, Zhang R, Cheung MKS, Leung W, Lau JYN, Fok M, Chen H, Chan KH, Yuen KY (2017) Efficacy of clarithromycin-naproxen-oseltamivir combination in the treatment of patients hospitalized for influenza A(H3N2) infection: an open-label randomized, controlled, phase IIb/III trial. Chest 151:1069–1080
Martin-Loeches I, Bermejo-Martin JF, Valles J, Granada R, Vidaur L, Vergara-Serrano JC, Martin M, Figueira JC, Sirvent JM, Blanquer J, Suarez D, Artigas A, Torres A, Diaz E, Rodriguez A (2013) Macrolide-based regimens in absence of bacterial co-infection in critically ill H1N1 patients with primary viral pneumonia. Intensive Care Med 39:693–702
Arabi YM, Deeb AM, Al-Hameed F, Mandourah Y, Almekhlafi GA, Sindi AA, Al-Omari A, Shalhoub S, Mady A, Alraddadi B, Almotairi A, Al Khatib K, Abdulmomen A, Qushmaq I, Solaiman O, Al-Aithan AM, Al-Raddadi R, Ragab A, Al Harthy A, Kharaba A, Jose J, Dabbagh T, Fowler RA, Balkhy HH, Merson L, Hayden FG, Saudi Critical Care Trials g (2019) Macrolides in critically ill patients with Middle East Respiratory Syndrome. Int J Infect Dis 81:184–190
Han K, Ma H, An X, Su Y, Chen J, Lian Z, Zhao J, Zhu BP, Fontaine RE, Feng Z, Zeng G (2011) Early use of glucocorticoids was a risk factor for critical disease and death from pH1N1 infection. Clin Infect Dis 53:326–333
Delaney JW, Pinto R, Long J, Lamontagne F, Adhikari NK, Kumar A, Marshall JC, Cook DJ, Jouvet P, Ferguson ND, Griesdale D, Burry LD, Burns KE, Hutchison J, Mehta S, Menon K, Fowler RA, Canadian Critical Care Trials Group HNC (2016) The influence of corticosteroid treatment on the outcome of influenza A(H1N1pdm09)-related critical illness. Crit Care 20:75
Lee FE, Walsh EE, Falsey AR (2011) The effect of steroid use in hospitalized adults with respiratory syncytial virus-related illness. Chest 140:1155–1161
Lee N, Allen Chan KC, Hui DS, Ng EK, Wu A, Chiu RW, Wong VW, Chan PK, Wong KT, Wong E, Cockram CS, Tam JS, Sung JJ, Lo YM (2004) Effects of early corticosteroid treatment on plasma SARS-associated Coronavirus RNA concentrations in adult patients. J Clin Virol 31:304–309
Arabi YM, Mandourah Y, Al-Hameed F, Sindi AA, Almekhlafi GA, Hussein MA, Jose J, Pinto R, Al-Omari A, Kharaba A, Almotairi A, Al Khatib K, Alraddadi B, Shalhoub S, Abdulmomen A, Qushmaq I, Mady A, Solaiman O, Al-Aithan AM, Al-Raddadi R, Ragab A, Balkhy HH, Al Harthy A, Deeb AM, Al Mutairi H, Al-Dawood A, Merson L, Hayden FG, Fowler RA, Saudi Critical Care Trial G (2018) Corticosteroid therapy for critically ill patients with middle east respiratory syndrome. Am J Respir Crit Care Med 197:757–767
Lee SM, Cheung CY, Nicholls JM, Hui KP, Leung CY, Uiprasertkul M, Tipoe GL, Lau YL, Poon LL, Ip NY, Guan Y, Peiris JS (2008) Hyperinduction of cyclooxygenase-2-mediated proinflammatory cascade: a mechanism for the pathogenesis of avian influenza H5N1 infection. J Infect Dis 198:525–535
Hung IF, Wang To KK, Chan J, Chan KH, Yuen KY. ECCMID 2019. O0815 Treatment of severe influenza A infection with celecoxib. https://www.escmid.org. Accessed 14 Sep 2019
Jia X, Liu B, Bao L, Lv Q, Li F, Li H, An Y, Zhang X, Cao B, Wang C (2018) Delayed oseltamivir plus sirolimus treatment attenuates H1N1 virus-induced severe lung injury correlated with repressed NLRP3 inflammasome activation and inflammatory cell infiltration. PLoS Pathog 14:e1007428
Huang CT, Hung CY, Chen TC, Lin CY, Lin YC, Chang CS, He YC, Huang YL, Dutta A (2017) Rapamycin adjuvant and exacerbation of severe influenza in an experimental mouse model. Sci Rep 7:4136
Wang CH, Chung FT, Lin SM, Huang SY, Chou CL, Lee KY, Lin TY, Kuo HP (2014) Adjuvant treatment with a mammalian target of rapamycin inhibitor, sirolimus, and steroids improves outcomes in patients with severe H1N1 pneumonia and acute respiratory failure. Crit Care Med 42:313–321
McAuley DF, Laffey JG, O’Kane CM, Perkins GD, Mullan B, Trinder TJ, Johnston P, Hopkins PA, Johnston AJ, McDowell C, McNally C, Investigators H-, Irish Critical Care Trials G (2014) Simvastatin in the acute respiratory distress syndrome. N Engl J Med 371:1695–1703
Calfee CS, Delucchi KL, Sinha P, Matthay MA, Hackett J, Shankar-Hari M, McDowell C, Laffey JG, O’Kane CM, McAuley DF, Irish Critical Care Trials G (2018) Acute respiratory distress syndrome subphenotypes and differential response to simvastatin: secondary analysis of a randomised controlled trial. Lancet Respir Med 6:691–698
Hung IF, To KK, Lee CK, Lee KL, Yan WW, Chan K, Chan WM, Ngai CW, Law KI, Chow FL, Liu R, Lai KY, Lau CC, Liu SH, Chan KH, Lin CK, Yuen KY (2013) Hyperimmune IV immunoglobulin treatment: a multicenter double-blind randomized controlled trial for patients with severe 2009 influenza A(H1N1) infection. Chest 144:464–473
Davey RT, Jr., Fernández-Cruz E, Markowitz N, Pett S, Babiker AG, Wentworth D, Khurana S, Engen N, Gordin F, Jain MK, Kan V, Polizzotto MN, Riska P, Ruxrungtham K, Temesgen Z, Lundgren J, Beigel JH, Lane HC, Neaton JD, Davey RT, Fernández-Cruz E, Markowitz N, Pett S, Babiker AG, Wentworth D, Khurana S, Engen N, Gordin F, Jain MK, Kan V, Polizzotto MN, Riska P, Ruxrungtham K, Temesgen Z, Lundgren J, Beigel JH, Lane HC, Neaton JD, Butts J, Denning E, DuChene A, Krum E, Harrison M, Meger S, Peterson R, Quan K, Shaughnessy M, Thompson G, Vock D, Metcalf J, Dewar R, Rehman T, Natarajan V, McConnell R, Flowers E, Smith K, Hoover M, Coyle EM, Munroe D, Aagaard B, Pearson M, Cursley A, Webb H, Hudson F, Russell C, Sy A, Purvis C, Jackson B, Collaco-Moraes Y, Carey D, Robson R, Sánchez A, Finley E, Conwell D, Losso MH, Gambardella L, Abela C, Lopez P, Alonso H, Touloumi G, Gioukari V, Anagnostou O, Avihingsanon A, Pussadee K, Ubolyam S, Omotosho B, Solórzano C, Petersen T, Vysyaraju K, Rizza SA, Whitaker JA, Nahra R, Baxter J, Coburn P, Gardner EM, Scott JA, Faber L, Pastor E, Makohon L, MacArthur RA, Hillman LM, Farrough MJ, Polenakovik HM, Clark LA, Colon RJ, Kunisaki KM, DeConcini M, Johnson SA, Wolfe CR, Mkumba L, Carbonneau JY, Morris A, Fitzpatrick ME, Kessinger CJ, Salata RA, Arters KA, Tasi CM, Panos RJ, Lach LA, Glesby MJ, Ham KA, Hughes VG, Schooley RT, Crouch D, Muttera L, Novak RM, Bleasdale SC, Zuckerman AE, Manosuthi W, Thaonyen S, Chiewcharn T, Suwanpimolkul G, Gatechumpol S, Bunpasang S, Angus BJ, Anderson M, Morgan M, Minton J, Gkamaletsou MN, Hambleton J, Price DA, Llewelyn MJ, Sweetman J, Carbone J, Arribas JR, Montejano R, Lobo Beristain JL, Martinez IZ, Barberan J, Hernandez P, Dwyer DE, Kok J, Borges A, Brandt CT, Knudsen LS, Sypsas N, Constantinou C, Markogiannakis A, Zakynthinos S, Katsaounou P, Kalomenidis I, Mykietiuk A, Alzogaray MF, Obed M, Macias LM, Ebensrtejin J, Burgoa P, Nannini E, Lahitte M, Perez-Patrigeon S, Martínez-Orozco JA, Ramírez-Hinojosa JP (2019) Anti-influenza hyperimmune intravenous immunoglobulin for adults with influenza A or B infection (FLU-IVIG): a double-blind, randomised, placebo-controlled trial. Lancet Respir Med. 7:951–963. https://doi.org/10.1016/S2213-2600(19)30253-X
Beigel JH, Aga E, Elie-Turenne M-C, Cho J, Tebas P, Clark CL, Metcalf JP, Ozment C, Raviprakash K, Beeler J, Holley HP, Jr., Warner S, Chorley C, Lane HC, Hughes MD, Davey RT, Jr., Beigel JH, Aga E, Elie-Turenne M-C, Cho J, Tebas P, Clark CL, Metcalf JP, Ozment C, Raviprakash K, Beeler J, Holley HP, Jr., Warner S, Chorley C, Lane HC, Hughes MD, Davey RT, Barron M, Bastani A, Bauer P, Borkowsky W, Cairns C, Deville J, Elie M-C, Fichtenbaum C, Finberg R, Jain M, Kaufman D, Lin M, Lin J, Maves R, Morrow L, Nguyen M-H, Park P, Polk C, Randolph A, Rao S, Rubinson L, Schofield C, Shoham S, Stalets E, Stapleton RD (2019) Anti-influenza immune plasma for the treatment of patients with severe influenza A: a randomised, double-blind, phase 3 trial. Lancet Respir Med. 7:941–950. https://doi.org/10.1016/S2213-2600(19)30199-7
Fowler AA 3rd, Truwit JD, Hite RD, Morris PE, DeWilde C, Priday A, Fisher B, Thacker LR 2nd, Natarajan R, Brophy DF, Sculthorpe R, Nanchal R, Syed A, Sturgill J, Martin GS, Sevransky J, Kashiouris M, Hamman S, Egan KF, Hastings A, Spencer W, Tench S, Mehkri O, Bindas J, Duggal A, Graf J, Zellner S, Yanny L, McPolin C, Hollrith T, Kramer D, Ojielo C, Damm T, Cassity E, Wieliczko A, Halquist M (2019) Effect of vitamin c infusion on organ failure and biomarkers of inflammation and vascular injury in patients with sepsis and severe acute respiratory failure: the CITRIS-ALI Randomized clinical trial. JAMA 322:1261–1270
Verweij PE, Bruggemann RJM, Wauters J, Rijnders BJA, Chiller T, van de Veerdonk F (2019) Influenza coinfection: be(a)ware of invasive aspergillosis. Clin Infect Dis 70:349–350
Rochwerg B, Brochard L, Elliott MW, Hess D, Hill NS, Nava S, Navalesi PMOTSC, Antonelli M, Brozek J, Conti G, Ferrer M, Guntupalli K, Jaber S, Keenan S, Mancebo J, Mehta S, Raoof SMOTTF (2017) Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J 50:1602426
Kumar A, Zarychanski R, Pinto R, Cook DJ, Marshall J, Lacroix J, Stelfox T, Bagshaw S, Choong K, Lamontagne F, Turgeon AF, Lapinsky S, Ahern SP, Smith O, Siddiqui F, Jouvet P, Khwaja K, McIntyre L, Menon K, Hutchison J, Hornstein D, Joffe A, Lauzier F, Singh J, Karachi T, Wiebe K, Olafson K, Ramsey C, Sharma S, Dodek P, Meade M, Hall R, Fowler RA, Canadian Critical Care Trials Group HNC (2009) Critically ill patients with 2009 influenza A(H1N1) infection in Canada. JAMA 302:1872–1879
Rodriguez A, Ferri C, Martin-Loeches I, Diaz E, Masclans JR, Gordo F, Sole-Violan J, Bodi M, Aviles-Jurado FX, Trefler S, Magret M, Moreno G, Reyes LF, Marin-Corral J, Yebenes JC, Esteban A, Anzueto A, Aliberti S, Restrepo MI, Grupo Espanol de Trabajo Gripe A Grave/Sociedad Espanola de Medicina Intensiva CyUCWG, investigators HNSWG (2017) Risk factors for noninvasive ventilation failure in critically ill subjects with confirmed influenza infection. Respir Care 62:1307–1315
Cheung TM, Yam LY, So LK, Lau AC, Poon E, Kong BM, Yung RW (2004) Effectiveness of noninvasive positive pressure ventilation in the treatment of acute respiratory failure in severe acute respiratory syndrome. Chest 126:845–850
Fowler RA, Guest CB, Lapinsky SE, Sibbald WJ, Louie M, Tang P, Simor AE, Stewart TE (2004) Transmission of severe acute respiratory syndrome during intubation and mechanical ventilation. Am J Respir Crit Care Med 169:1198–1202
Alraddadi BM, Qushmaq I, Al-Hameed FM, Mandourah Y, Almekhlafi GA, Jose J, Al-Omari A, Kharaba A, Almotairi A, Al Khatib K, Shalhoub S, Abdulmomen A, Mady A, Solaiman O, Al-Aithan AM, Al-Raddadi R, Ragab A, Balkhy HH, Al Harthy A, Sadat M, Tlayjeh H, Merson L, Hayden FG, Fowler RA, Arabi YM, Saudi Critical Care Trials G (2019) Noninvasive ventilation in critically ill patients with the Middle East respiratory syndrome. Influenza Other Respir Viruses 13:382–390
Patel BK, Wolfe KS, Pohlman AS, Hall JB, Kress JP (2016) Effect of noninvasive ventilation delivered by helmet vs face mask on the rate of endotracheal intubation in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA 315:2435–2441
Frat JP, Thille AW, Mercat A, Girault C, Ragot S, Perbet S, Prat G, Boulain T, Morawiec E, Cottereau A, Devaquet J, Nseir S, Razazi K, Mira JP, Argaud L, Chakarian JC, Ricard JD, Wittebole X, Chevalier S, Herbland A, Fartoukh M, Constantin JM, Tonnelier JM, Pierrot M, Mathonnet A, Beduneau G, Deletage-Metreau C, Richard JC, Brochard L, Robert R, Group FS, Network R (2015) High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med 372:2185–2196
Rello J, Perez M, Roca O, Poulakou G, Souto J, Laborda C, Balcells J, Serra J, Masclans JR, Investigators C (2012) High-flow nasal therapy in adults with severe acute respiratory infection: a cohort study in patients with 2009 influenza A/H1N1v. J Crit Care 27:434–439
Briel M, Meade M, Mercat A, Brower RG, Talmor D, Walter SD, Slutsky AS, Pullenayegum E, Zhou Q, Cook D, Brochard L, Richard JC, Lamontagne F, Bhatnagar N, Stewart TE, Guyatt G (2010) Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA 303:865–873
Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial I, Cavalcanti AB, Suzumura EA, Laranjeira LN, Paisani DM, Damiani LP, Guimaraes HP, Romano ER, Regenga MM, Taniguchi LNT, Teixeira C, Pinheiro de Oliveira R, Machado FR, Diaz-Quijano FA, Filho MSA, Maia IS, Caser EB, Filho WO, Borges MC, Martins PA, Matsui M, Ospina-Tascon GA, Giancursi TS, Giraldo-Ramirez ND, Vieira SRR, Assef M, Hasan MS, Szczeklik W, Rios F, Amato MBP, Berwanger O, Ribeiro de Carvalho CR, (2017) Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs low PEEP on Mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA 318:1335–1345
Boots RJ, Lipman J, Lassig-Smith M, Stephens DP, Thomas J, Shehabi Y, Bass F, Anthony A, Long D, Seppelt IM, Weisbrodt L, Erickson S, Beca J, Sherring C, McGuiness S, Parke R, Stachowski ER, Boyd R, Howet B (2011) Experience with high frequency oscillation ventilation during the 2009 H1N1 influenza pandemic in Australia and New Zealand. Anaesth Intensive Care 39:837–846
Ferguson ND, Cook DJ, Guyatt GH, Mehta S, Hand L, Austin P, Zhou Q, Matte A, Walter SD, Lamontagne F, Granton JT, Arabi YM, Arroliga AC, Stewart TE, Slutsky AS, Meade MO, Investigators OT, Investigators OT, Canadian Critical Care Trials G (2013) High-frequency oscillation in early acute respiratory distress syndrome. N Engl J Med 368:795–805
Young D, Lamb SE, Shah S, MacKenzie I, Tunnicliffe W, Lall R, Rowan K, Cuthbertson BH, Group OS (2013) High-frequency oscillation for acute respiratory distress syndrome. N Engl J Med 368:806–813
Meade MO, Young D, Hanna S, Zhou Q, Bachman TE, Bollen C, Slutsky AS, Lamb SE, Adhikari NKJ, Mentzelopoulos SD, Cook DJ, Sud S, Brower RG, Thompson BT, Shah S, Stenzler A, Guyatt G, Ferguson ND (2017) Severity of hypoxemia and effect of high-frequency oscillatory ventilation in acute respiratory distress syndrome. Am J Respir Crit Care Med 196:727–733
Guerin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, Mercier E, Badet M, Mercat A, Baudin O, Clavel M, Chatellier D, Jaber S, Rosselli S, Mancebo J, Sirodot M, Hilbert G, Bengler C, Richecoeur J, Gainnier M, Bayle F, Bourdin G, Leray V, Girard R, Baboi L, Ayzac L, Group PS (2013) Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 368:2159–2168
Xu Y, Deng X, Han Y, Zhou L, He W, Chen S, Nong L, Huang H, Zhang Y, Yu T, Li Y, Liu X (2015) A multicenter retrospective review of prone position ventilation (PPV) in treatment of severe human H7N9 avian flu. PLoS One 10:e0136520
Papazian L, Forel JM, Gacouin A, Penot-Ragon C, Perrin G, Loundou A, Jaber S, Arnal JM, Perez D, Seghboyan JM, Constantin JM, Courant P, Lefrant JY, Guerin C, Prat G, Morange S, Roch A, Investigators AS (2010) Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med 363:1107–1116
National Heart L, Blood Institute PCTN, Moss M, Huang DT, Brower RG, Ferguson ND, Ginde AA, Gong MN, Grissom CK, Gundel S, Hayden D, Hite RD, Hou PC, Hough CL, Iwashyna TJ, Khan A, Liu KD, Talmor D, Thompson BT, Ulysse CA, Yealy DM, Angus DC (2019) Early neuromuscular blockade in the acute respiratory distress syndrome. N Engl J Med 380:1997–2008
Combes A, Hajage D, Capellier G, Demoule A, Lavoue S, Guervilly C, Da Silva D, Zafrani L, Tirot P, Veber B, Maury E, Levy B, Cohen Y, Richard C, Kalfon P, Bouadma L, Mehdaoui H, Beduneau G, Lebreton G, Brochard L, Ferguson ND, Fan E, Slutsky AS, Brodie D, Mercat A, Eolia Trial Group R, Ecmonet (2018) Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med 378:1965–1975
Goligher EC, Tomlinson G, Hajage D, Wijeysundera DN, Fan E, Juni P, Brodie D, Slutsky AS, Combes A (2018) Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome and posterior probability of mortality benefit in a post hoc bayesian analysis of a randomized clinical trial. JAMA 320:2251–2259
Noah MA, Peek GJ, Finney SJ, Griffiths MJ, Harrison DA, Grieve R, Sadique MZ, Sekhon JS, McAuley DF, Firmin RK, Harvey C, Cordingley JJ, Price S, Vuylsteke A, Jenkins DP, Noble DW, Bloomfield R, Walsh TS, Perkins GD, Menon D, Taylor BL, Rowan KM (2011) Referral to an extracorporeal membrane oxygenation center and mortality among patients with severe 2009 influenza A(H1N1). JAMA 306:1659–1668
Alshahrani MS, Sindi A, Alshamsi F, Al-Omari A, El Tahan M, Alahmadi B, Zein A, Khatani N, Al-Hameed F, Alamri S, Abdelzaher M, Alghamdi A, Alfousan F, Tash A, Tashkandi W, Alraddadi R, Lewis K, Badawee M, Arabi YM, Fan E, Alhazzani W (2018) Extracorporeal membrane oxygenation for severe Middle East respiratory syndrome coronavirus. Ann Intensive Care 8:3
National Heart L, Blood Institute Acute Respiratory Distress Syndrome Clinical Trials N, Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF, Jr., Hite RD, Harabin AL, (2006) Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 354:2564–2575
Brown SM, Pittman J, Miller Iii RR, Horton KD, Markewitz B, Hirshberg E, Jones J, Grissom CK (2011) Right and left heart failure in severe H1N1 influenza A infection. Eur Respir J 37:112–118
Paddock CD, Liu L, Denison AM, Bartlett JH, Holman RC, Deleon-Carnes M, Emery SL, Drew CP, Shieh WJ, Uyeki TM, Zaki SR (2012) Myocardial injury and bacterial pneumonia contribute to the pathogenesis of fatal influenza B virus infection. J Infect Dis 205:895–905
Kwong JC, Schwartz KL, Campitelli MA, Chung H, Crowcroft NS, Karnauchow T, Katz K, Ko DT, McGeer AJ, McNally D, Richardson DC, Rosella LC, Simor A, Smieja M, Zahariadis G, Gubbay JB (2018) Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med 378:345–353
Chacko B, Peter JV, Pichamuthu K, Ramakrishna K, Moorthy M, Karthik R, John G (2012) Cardiac manifestations in patients with pandemic (H1N1) 2009 virus infection needing intensive care. J Crit Care 27(106):e101–e106
Mohite PN, Popov AF, Bartsch A, Zych B, Dhar D, Moza A, Krueger H, Simon AR (2011) Successful treatment of novel H1N1 influenza related fulminant myocarditis with extracorporeal life support. J Cardiothorac Surg 6:164
Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J (2012) Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One 7:e35797
Radonovich LJ Jr, Simberkoff MS, Bessesen MT, Brown AC, Cummings DAT, Gaydos CA, Los JG, Krosche AE, Gibert CL, Gorse GJ, Nyquist AC, Reich NG, Rodriguez-Barradas MC, Price CS, Perl TM, Pi Res (2019) N95 respirators vs medical masks for preventing influenza among health care personnel: a randomized clinical trial. JAMA 322:824–833
Loeb M, Dafoe N, Mahony J, John M, Sarabia A, Glavin V, Webby R, Smieja M, Earn DJ, Chong S, Webb A, Walter SD (2009) Surgical mask vs N95 respirator for preventing influenza among health care workers: a randomized trial. JAMA 302:1865–1871
MacIntyre CR, Seale H, Dung TC, Hien NT, Nga PT, Chughtai AA, Rahman B, Dwyer DE, Wang Q (2015) A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open 5:e006577
Hirose R, Nakaya T, Naito Y, Daidoji T, Bandou R, Inoue K, Dohi O, Yoshida N, Konishi H, Itoh Y (2019) Situations leading to reduced effectiveness of current hand hygiene against infectious mucus from influenza virus-infected patients. mSphere 4:e00474–e00479
WHO public health research agenda for influenza. https://www.who.int/influenza/resources/research/en/. Last accessed Jan 4-2020
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Arabi is the principal investigator on a clinical trial for lopinavir/ritonavir and interferon in Middle East respiratory syndrome (MERS) and that he was a non-paid consultant on antiviral active for MERS-coronavirus (CoV) for Gilead Sciences and SAB Biotherapeutics. Dr. Hayden’s institution received funding from GlaxoSmithKline (Data Safety Monitoring Board [DSMB] member for influenza randomized-controlled trial [RCT]), Celltrion (DSMB chair for influenza RCT), and Vaccitech (DSMB chair for influenza RCTs); he received honoraria from World Health Organization (consultant on influenza and emerging viral infections) and the University of Alabama (Scientific Advisory Board member for National Institutes of Health-sponsored Antiviral Discovery and Development Consortium); he disclosed that he has been a non-paid consultant on antivirals active for MERS-CoV for Gilead Sciences, SAB Biotherapeutics, and Regeneron, and for multiple companies on influenza therapeutics; Cidara, Shionogi, Seqirus, and resTORbio have made charitable contributions to the Ford Haitian Orphanage and School for his consulting time; Shionogi and Roche have provided meeting travel support.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Arabi, Y.M., Fowler, R. & Hayden, F.G. Critical care management of adults with community-acquired severe respiratory viral infection. Intensive Care Med 46, 315–328 (2020). https://doi.org/10.1007/s00134-020-05943-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-020-05943-5