Abstract
Purpose
This study aimed to elucidate the impact of protocolized family support intervention on length of stay (LOS) in the intensive care unit (ICU) through a systematic review and meta-analysis.
Methods
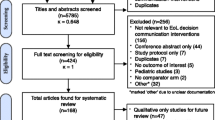
Medline, EMBASE, the Cochrane Central Register of Controlled Trials, and other web-based databases were referenced since inception until November 26, 2018. We included randomized-controlled trials wherein protocolized family support interventions were conducted for enhanced communication and shared medical decision-making. LOS (in days) and mortality were evaluated using a random-effects model, and adjusted LOS was estimated using a mixed-effects model.
Results
We included seven randomized-controlled trials with 3477 patients. Protocolized family support interventions were found to significantly reduce the ICU LOS {mean difference = − 0.89 [95% confidence interval (CI) = − 1.50 to − 0.27]} and hospital LOS [mean difference = − 3.78 (95% CI = − 5.26 to − 2.29)]; the results of the mixed-effect model showed that they significantly reduced ICU LOS after adjusting for the therapeutic goal [mean difference = − 1.30 (95% CI = − 2.35 to − 0.26)], methods of measurement [mean difference = − 0.89 (95% CI = − 1.55 to − 0.22)], and timing of intervention [mean difference = − 1.05 (95% CI = − 2.05 to − 0.05)]. Similar results were found after adjusting for patients’ disease severity [mean difference = − 1.21 (95% CI = − 2.03 to − 0.39)] and the trim-and-fill method [mean difference = − 0.86 (95% CI = − 1.44 to − 0.28)]. There was no difference in mortality rate in ICU and hospital between the protocolized intervention and control groups.
Conclusions
Protocolized family support intervention for enhanced communication and shared decision-making with the family reduced ICU LOS in critically ill patients without impacting mortality.




Similar content being viewed by others
Availability of data and material
The data sets used and/or analyzed can be obtained from the corresponding author on reasonable request.
Change history
08 October 2019
The original version of this article unfortunately contained a mistake. One of the affiliations was incorrect: Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Veterans Health Service Medical Center, Portland, USA.
08 October 2019
The original version of this article unfortunately contained a mistake. One of the affiliations was incorrect: Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Veterans Health Service Medical Center, Portland, USA.
References
Kynoch K, Chang A, Coyer F, McArdle A (2016) The effectiveness of interventions to meet family needs of critically ill patients in an adult intensive care unit: a systematic review update. JBI Database Syst Rev Implement Rep 14:181–234
Goldfarb MJ, Bibas L, Bartlett V, Jones H, Khan N (2017) Outcomes of patient- and family-centered care interventions in the ICU: a systematic review and meta-analysis. Crit Care Med 45:1751–1761
Kyeremanteng K, Gagnon LP, Thavorn K, Heyland D, D’Egidio G (2018) The impact of palliative care consultation in the ICU on length of stay: a systematic review and cost evaluation. J Intensive Care Med 33:346–353
Wendler D, Rid A (2011) Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med 154:336–346
Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, Annane D, Bleichner G, Bollaert PE, Darmon M, Fassier T, Galliot R, Garrouste-Orgeas M, Goulenok C, Goldgran-Toledano D, Hayon J, Jourdain M, Kaidomar M, Laplace C, Larche J, Liotier J, Papazian L, Poisson C, Reignier J, Saidi F, Schlemmer B (2005) Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 171:987–994
Gries CJ, Engelberg RA, Kross EK, Zatzick D, Nielsen EL, Downey L, Curtis JR (2010) Predictors of symptoms of posttraumatic stress and depression in family members after patient death in the ICU. Chest 137:280–287
Kon AA, Davidson JE, Morrison W, Danis M, White DB (2016) Shared decision making in ICUs: an American College of critical care medicine and american thoracic society policy statement. Crit Care Med 44:188–201
Davidson JE, Aslakson RA, Long AC, Puntillo KA, Kross EK, Hart J, Cox CE, Wunsch H, Wickline MA, Nunnally ME, Netzer G, Kentish-Barnes N, Sprung CL, Hartog CS, Coombs M, Gerritsen RT, Hopkins RO, Franck LS, Skrobik Y, Kon AA, Scruth EA, Harvey MA, Lewis-Newby M, White DB, Swoboda SM, Cooke CR, Levy MM, Azoulay E, Curtis JR (2017) Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med 45:103–128
Adanir T, Erdogan I, Hunerli G, Unveren G, Dasci H, Cetin HY, Ozsan I, Aydin U (2014) The effect of psychological support for the relatives of intensive care unit patients on cadaveric organ donation rate. Transpl Proc 46:3249–3252
Campbell ML, Guzman JA (2003) Impact of a proactive approach to improve end-of-life care in a medical ICU. Chest 123:266–271
Lilly CM, De Meo DL, Sonna LA, Haley KJ, Massaro AF, Wallace RF, Cody S (2000) An intensive communication intervention for the critically ill. Am J Med 109:469–475
Wong DT, Gomez M, McGuire GP, Kavanagh B (1999) Utilization of intensive care unit days in a Canadian medical-surgical intensive care unit. Crit Care Med 27:1319–1324
Stricker K, Rothen HU, Takala J (2003) Resource use in the ICU: short- vs. long-term patients. Acta Anaesthesiol Scand 47:508–515
Zimmerman JE, Kramer AA, McNair DS, Malila FM, Shaffer VL (2006) Intensive care unit length of stay: benchmarking based on Acute Physiology and Chronic Health Evaluation (APACHE) IV. Crit Care Med 34:2517–2529
Bagshaw SM, Opgenorth D, Potestio M, Hastings SE, Hepp SL, Gilfoyle E, McKinlay D, Boucher P, Meier M, Parsons-Leigh J, Gibney RT, Zygun DA, Stelfox HT (2017) Healthcare provider perceptions of causes and consequences of ICU capacity strain in a large publicly funded integrated health region: a qualitative study. Crit Care Med 45:e347–e356
Clay AM, Parsh B (2016) Patient- and family-centered care: it’s not just for pediatrics anymore. AMA J Ethics 18:40–44
Gruenberg DA, Shelton W, Rose SL, Rutter AE, Socaris S, McGee G (2006) Factors influencing length of stay in the intensive care unit. Am J Critical Care 15:502–509
Lautrette A, Darmon M, Megarbane B, Joly LM, Chevret S, Adrie C, Barnoud D, Bleichner G, Bruel C, Choukroun G, Curtis JR, Fieux F, Galliot R, Garrouste-Orgeas M, Georges H, Goldgran-Toledano D, Jourdain M, Loubert G, Reignier J, Saidi F, Souweine B, Vincent F, Barnes NK, Pochard F, Schlemmer B, Azoulay E (2007) A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 356:469–478
Hutchison PJ, McLaughlin K, Corbridge T, Michelson KN, Emanuel L, Sporn PH, Crowley-Matoka M (2016) Dimensions and role-specific mediators of surrogate trust in the ICU. Crit Care Med 44:2208–2214
Mosenthal AC, Murphy PA, Barker LK, Lavery R, Retano A, Livingston DH (2008) Changing the culture around end-of-life care in the trauma intensive care unit. J Trauma 64:1587–1593
Schneiderman LJ, Gilmer T, Teetzel HD, Dugan DO, Blustein J, Cranford R, Briggs KB, Komatsu GI, Goodman-Crews P, Cohn F, Young EW (2003) Effect of ethics consultations on nonbeneficial life-sustaining treatments in the intensive care setting: a randomized controlled trial. JAMA 290:1166–1172
Khandelwal N, Kross EK, Engelberg RA, Coe NB, Long AC, Curtis JR (2015) Estimating the effect of palliative care interventions and advance care planning on ICU utilization: a systematic review. Crit Care Med 43:1102–1111
White DB, Angus DC, Shields AM, Buddadhumaruk P, Pidro C, Paner C, Chaitin E, Chang CH, Pike F, Weissfeld L, Kahn JM, Darby JM, Kowinsky A, Martin S, Arnold RM (2018) A randomized trial of a family-support intervention in intensive care units. N Engl J Med 378:2365–2375
Curtis JR, Treece PD, Nielsen EL, Gold J, Ciechanowski PS, Shannon SE, Khandelwal N, Young JP, Engelberg RA (2016) Randomized trial of communication facilitators to reduce family distress and intensity of end-of-life care. Am J Respir Crit Care Med 193:154–162
Carson SS, Cox CE, Wallenstein S, Hanson LC, Danis M, Tulsky JA, Chai E, Nelson JE (2016) Effect of palliative care-led meetings for families of patients with chronic critical illness: a randomized clinical trial. JAMA 316:51–62
Garrouste-Orgeas M, Max A, Lerin T, Gregoire C, Ruckly S, Kloeckner M, Brochon S, Pichot E, Simons C, El-Mhadri M, Bruel C, Philippart F, Fournier J, Tiercelet K, Timsit JF, Misset B (2016) Impact of proactive nurse participation in ICU family conferences: a mixed-method study. Crit Care Med 44:1116–1128
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6:e1000100
Brown SM, Rozenblum R, Aboumatar H, Fagan MB, Milic M, Lee BS, Turner K, Frosch DL (2015) Defining patient and family engagement in the intensive care unit. Am J Respir Crit Care Med 191:358–360
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C (2016) PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol 75:40–46
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Higgins JP, Green S (2011) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The cochrane collaboration. Available at https://handbook-5-1.cochrane.org/. Accessed 30 June 2019
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed) 343:d5928
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56:455–463
Viechtbauer WJJoss (2010) Conducting meta-analyses in R with the metafor package. Available at https://www.jstatsoft.org/article/view/v036i03. Accessed 30 June 2019
Curtis JR, Nielsen EL, Treece PD, Downey L, Dotolo D, Shannon SE, Back AL, Rubenfeld GD, Engelberg RA (2011) Effect of a quality-improvement intervention on end-of-life care in the intensive care unit: a randomized trial. Am J Respir Crit Care Med 183:348–355
Oostenbrink JB, Buijs-Van der Woude T, van Agthoven M, Koopmanschap MA, Rutten FF (2003) Unit costs of inpatient hospital days. PharmacoEconomics 21:263–271
Hughes M, MacKirdy FN, Norrie J, Grant IS (2001) Outcome of long-stay intensive care patients. Intensive Care Med 27:779–782
Aslakson R, Cheng J, Vollenweider D, Galusca D, Smith TJ, Pronovost PJ (2014) Evidence-based palliative care in the intensive care unit: a systematic review of interventions. J Palliat Med 17:219–235
Nelson JE, Walker AS, Luhrs CA, Cortez TB, Pronovost PJ (2009) Family meetings made simpler: a toolkit for the intensive care unit. J Crit Care 24:626.e627-614
Martins B, Oliveira RA, Cataneo AJM (2017) Palliative care for terminally ill patients in the intensive care unit: systematic review and metaanalysis. Palliat Support Care 15:376–383
Long AC, Kross EK, Engelberg RA, Downey L, Nielsen EL, Back AL, Curtis JR (2014) Quality of dying in the ICU: is it worse for patients admitted from the hospital ward compared to those admitted from the emergency department? Intensive Care Med 40:1688–1697
Gries CJ, Curtis JR, Wall RJ, Engelberg RA (2008) Family member satisfaction with end-of-life decision making in the ICU. Chest 133:704–712
Gerstel E, Engelberg RA, Koepsell T, Curtis JR (2008) Duration of withdrawal of life support in the intensive care unit and association with family satisfaction. Am J Respir Crit Care Med 178:798–804
Glavan BJ, Engelberg RA, Downey L, Curtis JR (2008) Using the medical record to evaluate the quality of end-of-life care in the intensive care unit. Crit Care Med 36:1138–1146
Lamba S, Murphy P, McVicker S, Harris Smith J, Mosenthal AC (2012) Changing end-of-life care practice for liver transplant service patients: structured palliative care intervention in the surgical intensive care unit. J Pain Symptom Manag 44:508–519
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Funding
The authors declare that they have taken no support from any organization for the submitted work. The authors also have no conflicts of interest to declare.
Author information
Authors and Affiliations
Contributions
Study concept and design: HWL and YJL. Data acquisition: HWL and YKP. Data analysis and interpretation: HWL and EJJ. Drafting of the manuscript: HWL. Critical revision of the manuscript and important intellectual content: HWL and YJL. Study supervision: YJL.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
134_2019_5681_MOESM4_ESM.tiff
Supplementary appendix 4. Forest plot of subgroup analysis for the intensive care unit length of stay by therapeutic goal (TIFF 1154 kb)
134_2019_5681_MOESM5_ESM.tiff
Supplementary appendix 5. Forest plot of subgroup analysis for the intensive care unit length of stay by method of measurement (TIFF 1160 kb)
134_2019_5681_MOESM6_ESM.tiff
Supplementary appendix 6. Forest plot of subgroup analysis for the intensive care unit length of stay by timing of intervention (TIFF 1205 kb)
Rights and permissions
About this article
Cite this article
Lee, H.W., Park, Y., Jang, E.J. et al. Intensive care unit length of stay is reduced by protocolized family support intervention: a systematic review and meta-analysis. Intensive Care Med 45, 1072–1081 (2019). https://doi.org/10.1007/s00134-019-05681-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-019-05681-3