Abstract
Purpose
The effects of the route of nutrition on the gut mucosa of patients with shock are unclear. Plasma citrulline concentration is a marker of enterocyte mass, and plasma intestinal fatty acid binding protein (I-FABP) concentration is a marker of enterocyte damage. We aimed to study the effect of the route of nutrition on plasma citrulline concentration measured at day 3 of nutrition.
Materials and methods
Ancillary study of the NUTRIREA-2 trial. Ventilated adults with shock were randomly assigned to receive enteral or parenteral nutrition. Enterocyte biomarkers were measured at baseline, day 3, and day 8 of nutrition.
Result
A total of 165 patients from 13 French ICUs were included in the study: 85 patients in the enteral group and 80 patients in the parenteral group. At baseline, plasma citrulline was low without difference between groups (12.2 µmol L−1 vs 13.3 µmol L−1). At day 3, plasma citrulline concentration was higher in the enteral group than in the parenteral group (18.7 µmol L−1 vs 15.3 µmol L−1, p = 0.01). Plasma I-FABP concentration was increased at baseline, without difference between groups (245 pg mL−1 vs 244 pg mL−1). Plasma I-FABP concentration was higher in the enteral group than in the parenteral group at day 3 and day 8 (158 pg mL−1 vs 50 pg mL−1, p = 0.005 and 225 pg mL−1 vs 50 pg mL−1, p = 0.03).
Conclusion
Plasma citrulline concentration was higher after 3 days of enteral nutrition than after 3 days of parenteral nutrition. This result raises the question of the possibility that enteral nutrition is associated with a more rapid restoration of enterocyte mass than parenteral nutrition.


Similar content being viewed by others
References
Reintam Blaser A, Poeze M, Malbrain MLNG, Björck M, Oudemans-van Straaten HM, Starkopf J et al (2013) Gastrointestinal symptoms during the first week of intensive care are associated with poor outcome: a prospective multicentre study. Intensive Care Med 39(5):899–909
Piton G, Capellier G (2016) Biomarkers of gut barrier failure in the ICU. Curr Opin Crit Care 22(2):152–160
Crenn P, Coudray-Lucas C, Thuillier F, Cynober L, Messing B (2000) Postabsorptive plasma citrulline concentration is a marker of absorptive enterocyte mass and intestinal failure in humans. Gastroenterology 119(6):1496–1505
Crenn P, Vahedi K, Lavergne-Slove A, Cynober L, Matuchansky C, Messing B (2003) Plasma citrulline: a marker of enterocyte mass in villous atrophy-associated small bowel disease. Gastroenterology 124(5):1210–1219
Piton G, Manzon C, Cypriani B, Carbonnel F, Capellier G (2011) Acute intestinal failure in critically ill patients: is plasma citrulline the right marker? Intensive Care Med 37(6):911–917
Noordally SO, Sohawon S, Semlali H, Michely D, Devriendt J, Gottignies P (2012) Is there a correlation between circulating levels of citrulline and intestinal dysfunction in the critically ill? Nutr Clin Pract 27(4):527–532
Fagoni N, Piva S, Marino R, Chiarini G, Ferrari D, Grespi E et al (2017) The IN-PANCIA study: clinical evaluation of gastrointestinal dysfunction and failure, multiple organ failure, and levels of citrulline in critically ill patients. J Intensive Care Med. https://doi.org/10.1177/0885066617742594
Kanda T, Fujii H, Tani T, Murakami H, Suda T, Sakai Y et al (1996) Intestinal fatty acid-binding protein is a useful diagnostic marker for mesenteric infarction in humans. Gastroenterology 110(2):339–343
Thuijls G, van Wijck K, Grootjans J, Derikx JPM, van Bijnen AA, Heineman E et al (2011) Early diagnosis of intestinal ischemia using urinary and plasma fatty acid binding proteins. Ann Surg 253(2):303–308
Reignier J, Boisramé-Helms J, Brisard L, Lascarrou J-B, Ait HA, Anguel N et al (2018) Enteral versus parenteral early nutrition in ventilated adults with shock: a randomised, controlled, multicentre, open-label, parallel-group study (NUTRIREA-2). Lancet 391(10116):133–143
Le Boucher J, Charret C, Coudray-Lucas C, Giboudeau J, Cynober L (1997) Amino acid determination in biological fluids by automated ion-exchange chromatography: performance of Hitachi L-8500A. Clin Chem 43(8 Pt 1):1421–1428
Curis E, Nicolis I, Moinard C, Osowska S, Zerrouk N, Bénazeth S et al (2005) Almost all about citrulline in mammals. Amino Acids 29(3):177–205
Crenn P, Messing B, Cynober L (2008) Citrulline as a biomarker of intestinal failure due to enterocyte mass reduction. Clin Nutr 27(3):328–339
Treskes N, Persoon AM, van Zanten ARH (2017) Diagnostic accuracy of novel serological biomarkers to detect acute mesenteric ischemia: a systematic review and meta-analysis. Intern Emerg Med 12(6):821–836
Piton G, Belon F, Cypriani B, Regnard J, Puyraveau M, Manzon C et al (2013) Enterocyte damage in critically ill patients is associated with shock condition and 28-day mortality. Crit Care Med 41(9):2169–2176
Piton G, Cypriani B, Regnard J, Patry C, Puyraveau M, Capellier G (2015) Catecholamine use is associated with enterocyte damage in critically ill patients. Shock 43(5):437–442
Ludewig S, Jarbouh R, Ardelt M, Mothes H, Rauchfuß F, Fahrner R et al (2017) Bowel ischemia in ICU patients: diagnostic value of I-FABP depends on the interval to the triggering event. Gastroenterol Res Pract 2017:2795176
Coopersmith CM, Stromberg PE, Davis CG, Dunne WM, Amiot DM, Karl IE et al (2003) Sepsis from Pseudomonas aeruginosa pneumonia decreases intestinal proliferation and induces gut epithelial cell cycle arrest. Crit Care Med 31(6):1630–1637
Williams JM, Duckworth CA, Watson AJM, Frey MR, Miguel JC, Burkitt MD et al (2013) A mouse model of pathological small intestinal epithelial cell apoptosis and shedding induced by systemic administration of lipopolysaccharide. Dis Model Mech 6(6):1388–1399
Meng M, Klingensmith NJ, Liang Z, Lyons JD, Fay KT, Chen C-W et al (2019) Regulators of Intestinal Epithelial Migration in Sepsis. Shock 51(1):88–96
Leaphart CL, Qureshi F, Cetin S, Li J, Dubowski T, Baty C et al (2007) Interferon-gamma inhibits intestinal restitution by preventing gap junction communication between enterocytes. Gastroenterology 132(7):2395–2411
Fukatsu K (2014) Impact of the feeding route on gut mucosal immunity. Curr Opin Clin Nutr Metab Care. 17(2):164–170
Wu Y, Kudsk KA, DeWitt RC, Tolley EA, Li J (1999) Route and type of nutrition influence IgA-mediating intestinal cytokines. Ann Surg. 229(5):662–667 (discussion 667–668)
Briassoulis G, Venkataraman S, Thompson A (2010) Cytokines and metabolic patterns in pediatric patients with critical illness. Clin Dev Immunol 2010:354047
Spanaki AM, Tavladaki T, Dimitriou H, Kozlov AV, Duvigneau JC, Meleti E et al (2018) Longitudinal profiles of metabolism and bioenergetics associated with innate immune hormonal inflammatory responses and amino-acid kinetics in severe sepsis and systemic inflammatory response syndrome in children. JPEN J Parenter Enteral Nutr 42(6):1061–1074
Parent BA, Seaton M, Djukovic D, Gu H, Wheelock B, Navarro SL et al (2017) Parenteral and enteral nutrition in surgical critical care: plasma metabolomics demonstrates divergent effects on nitrogen, fatty-acid, ribonucleotide, and oxidative metabolism. J Trauma Acute Care Surg 82(4):704–713
Khalid I, Doshi P, Di Giovine B (2010) Early enteral nutrition and outcomes of critically ill patients treated with vasopressors and mechanical ventilation. Am J Crit Care 19(3):261–268
Ohbe H, Jo T, Yamana H, Matsui H, Fushimi K, Yasunaga H (2018) Early enteral nutrition for cardiogenic or obstructive shock requiring venoarterial extracorporeal membrane oxygenation: a nationwide inpatient database study. Intensive Care Med 44(8):1258–1265
Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP et al (2019) ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr 38(1):48–79
Seidner DL, Joly F, Youssef NN (2015) Effect of teduglutide, a glucagon-like peptide 2 analog, on citrulline levels in patients with short bowel syndrome in two phase III randomized trials. Clin Transl Gastroenterol 6:e93
Poole A, Deane A, Summers M, Fletcher J, Chapman M (2015) The relationship between fasting plasma citrulline concentration and small intestinal function in the critically ill. Crit Care 19(1):16
Piton G, Capellier G (2015) Plasma citrulline in the critically ill: intriguing biomarker, cautious interpretation. Crit Care 19:204
Schellekens DHSM, Grootjans J, Dello SAWG, van Bijnen AA, van Dam RM, Dejong CHC et al (2014) Plasma intestinal fatty acid-binding protein levels correlate with morphologic epithelial intestinal damage in a human translational ischemia-reperfusion model. J Clin Gastroenterol 48(3):253–260
Edinburgh RM, Hengist A, Smith HA, Travers RL, Koumanov F, Betts JA et al (2018) Preexercise breakfast ingestion versus extended overnight fasting increases postprandial glucose flux after exercise in healthy men. Am J Physiol Endocrinol Metab. 315(5):E1062–E1074
March DS, Marchbank T, Playford RJ, Jones AW, Thatcher R, Davison G (2017) Intestinal fatty acid-binding protein and gut permeability responses to exercise. Eur J Appl Physiol 117(5):931–941
Funding
The NUTRIREA-2 study was supported by a Grant from the French Ministry of Health, PHRCN-12-0184.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the ethics committee of the French Intensive Care Society and appropriate French authorities.
Informed consent
According to French law, because the treatments and strategies used in the study were classified as standard care, there was no requirement for signed consent, but the patients or next of kin were informed about the study before enrolment and confirmed this fact in writing.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
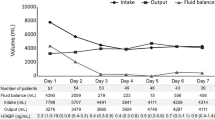
134_2019_5649_MOESM1_ESM.jpg
Supplementary Data, Fig. 1. Flow chart of the study. Among the 2410 patients included in the NUTRIREA-2 trial, 165 patients from 13 French ICUs were included in this substudy: 85 patients in the enteral group and 80 patients in the parenteral group. (JPEG 23 kb)
Rights and permissions
About this article
Cite this article
Piton, G., Le Gouge, A., Brulé, N. et al. Impact of the route of nutrition on gut mucosa in ventilated adults with shock: an ancillary of the NUTRIREA-2 trial. Intensive Care Med 45, 948–956 (2019). https://doi.org/10.1007/s00134-019-05649-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-019-05649-3