Abstract
Purpose
Mechanisms of circulatory failure are complex and frequently intricate in septic shock. Better characterization could help to optimize hemodynamic support.
Methods
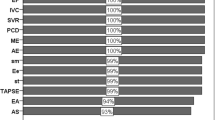
Two published prospective databases from 12 different ICUs including echocardiographic monitoring performed by a transesophageal route at the initial phase of septic shock were merged for post hoc analysis. Hierarchical clustering in a principal components approach was used to define cardiovascular phenotypes using clinical and echocardiographic parameters. Missing data were imputed.
Findings
A total of 360 patients (median age 64 [55; 74]) were included in the analysis. Five different clusters were defined: patients well resuscitated (cluster 1, n = 61, 16.9%) without left ventricular (LV) systolic dysfunction, right ventricular (RV) failure or fluid responsiveness, patients with LV systolic dysfunction (cluster 2, n = 64, 17.7%), patients with hyperkinetic profile (cluster 3, n = 84, 23.3%), patients with RV failure (cluster 4, n = 81, 22.5%) and patients with persistent hypovolemia (cluster 5, n = 70, 19.4%). Day 7 mortality was 9.8%, 32.8%, 8.3%, 27.2%, and 23.2%, while ICU mortality was 21.3%, 50.0%, 23.8%, 42.0%, and 38.6% in clusters 1, 2, 3, 4, and 5, respectively (p < 0.001 for both).
Conclusion
Our clustering approach on a large population of septic shock patients, based on clinical and echocardiographic parameters, was able to characterize five different cardiovascular phenotypes. How this could help physicians to optimize hemodynamic support should be evaluated in the future.



Similar content being viewed by others
References
Hess ML, Hastillo A, Greenfield LJ (1981) Spectrum of cardiovascular function during gram-negative sepsis. Prog Cardiovasc Dis 23:279–298
Parker MM, Shelhamer JH, Bacharach SL et al (1984) Profound but reversible myocardial depression in patients with septic shock. Ann Intern Med 100:483–490
De Backer D, Bakker J, Cecconi M et al (2018) Alternatives to the Swan–Ganz catheter. Intensive Care Med 44:730–741. https://doi.org/10.1007/s00134-018-5187-8
Vieillard-Baron A, Schmitt JM, Beauchet A et al (2001) Early preload adaptation in septic shock? A transesophageal echocardiographic study. Anesthesiology 94:400–406
Bégot E, Dalmay F, Etchecopar C et al (2015) Hemodynamic assessment of ventilated ICU patients with cardiorespiratory failure using a miniaturized multiplane transesophageal echocardiography probe. Intensive Care Med 41:1886–1894. https://doi.org/10.1007/s00134-015-3998-4
Vieillard-Baron A, Caille V, Charron C et al (2008) Actual incidence of global left ventricular hypokinesia in adult septic shock. Crit Care Med 36:1701–1706. https://doi.org/10.1097/CCM.0b013e318174db05
Coopersmith CM, De Backer D, Deutschman CS et al (2018) Surviving Sepsis Campaign: research priorities for sepsis and septic shock. Intensive Care Med 44:1400–1426. https://doi.org/10.1007/s00134-018-5175-z
Perner A, Cecconi M, Cronhjort M et al (2018) Expert statement for the management of hypovolemia in sepsis. Intensive Care Med 44:791–798. https://doi.org/10.1007/s00134-018-5177-x
Macdonald SPJ, Keijzers G, Taylor DM et al (2018) Restricted fluid resuscitation in suspected sepsis associated hypotension (REFRESH): a pilot randomised controlled trial. Intensive Care Med 44:2070–2078. https://doi.org/10.1007/s00134-018-5433-0
Vieillard-Baron A, Prin S, Chergui K et al (2003) Hemodynamic instability in sepsis: bedside assessment by Doppler echocardiography. Am J Respir Crit Care Med 168:1270–1276. https://doi.org/10.1164/rccm.200306-816CC
Åneman A, Vieillard-Baron A (2016) Cardiac dysfunction in sepsis. Intensive Care Med 42:2073–2076. https://doi.org/10.1007/s00134-016-4503-4
Vignon P, Bégot E, Mari A et al (2018) Hemodynamic assessment of patients with septic shock using transpulmonary thermodilution and critical care echocardiography: a comparative study. Chest 153:55–64. https://doi.org/10.1016/j.chest.2017.08.022
Vignon P, Repesse X, Bégot E et al (2017) Comparison of echocardiographic indices used to predict fluid responsiveness in ventilated patients. Am J Respir Crit Care Med 195:1022–1032. https://doi.org/10.1164/rccm.201604-0844OC
Huang SJ, Nalos M, McLean AS (2013) Is early ventricular dysfunction or dilatation associated with lower mortality rate in adult severe sepsis and septic shock? A meta-analysis. Crit Care 17:R96. https://doi.org/10.1186/cc12741
Landesberg G, Gilon D, Meroz Y et al (2012) Diastolic dysfunction and mortality in severe sepsis and septic shock. Eur Heart J 33:895–903. https://doi.org/10.1093/eurheartj/ehr351
Vieillard-Baron A, Naeije R, Haddad F et al (2018) Diagnostic workup, etiologies and management of acute right ventricle failure. Intensive Care Med 44:774–790. https://doi.org/10.1007/s00134-018-5172-2
Vieillard-Baron A, Chergui K, Rabiller A et al (2004) Superior vena caval collapsibility as a gauge of volume status in ventilated septic patients. Intensive Care Med 30:1–6. https://doi.org/10.1007/s00134-004-2361-y
Wetterslev M, Møller-Sørensen H, Johansen RR, Perner A (2016) Systematic review of cardiac output measurements by echocardiography vs. thermodilution: the techniques are not interchangeable. Intensive Care Med 42:1223–1233. https://doi.org/10.1007/s00134-016-4258-y
Lê S, Josse J, Husson F (2008) FactoMineR: an R package for multivariate analysis. J Stat Soft 25:1–18
Husson F, Josse J, Pagès J (2010) Principal component methods—hierarchical clustering—partitional clustering: why would be need to choose for visualizing data? Technical report, pp 1–17
Josse J, Pagès J, Husson F (2011) Multiple imputation in principal component analysis. Adv Data Anal Classif 5:231–246. https://doi.org/10.1007/s11634-011-0086-7
Barraud D, Faivre V, Damy T et al (2007) Levosimendan restores both systolic and diastolic cardiac performance in lipopolysaccharide-treated rabbits: comparison with dobutamine and milrinone. Crit Care Med 35:1376–1382. https://doi.org/10.1097/01.CCM.0000261889.18102.84
Robotham JL, Takata M, Berman M, Harasawa Y (1991) Ejection fraction revisited. Anesthesiology 74:172–183. https://doi.org/10.1097/00000542-199101000-00026
Jardin F, Brun-Ney D, Auvert B et al (1990) Sepsis-related cardiogenic shock. Crit Care Med 18:1055–1060. https://doi.org/10.1097/00003246-199010000-00001
Boissier F, Razazi K, Seemann A et al (2017) Left ventricular systolic dysfunction during septic shock: the role of loading conditions. Intensive Care Med 43:633–642. https://doi.org/10.1007/s00134-017-4698-z
Vignon P, Allot V, Lesage J et al (2007) Diagnosis of left ventricular diastolic dysfunction in the setting of acute changes in loading conditions. Crit Care 11:R43. https://doi.org/10.1186/cc5736
Suffredini AF, Fromm RE, Parker MM et al (1989) The cardiovascular response of normal humans to the administration of endotoxin. N Engl J Med 321:280–287. https://doi.org/10.1056/NEJM198908033210503
Perner A, Vieillard-Baron A, Bakker J (2015) Fluid resuscitation in ICU patients: Quo vadis? Intensive Care Med 41:1667–1669. https://doi.org/10.1007/s00134-015-3900-4
Murakawa K, Kobayashi A (1988) Effects of vasopressors on renal tissue gas tensions during hemorrhagic shock in dogs. Crit Care Med 16:789–792
Vieillard-Baron A, Naeije R, Haddad F et al (2018) Diagnostic workup, etiologies and management of acute right ventricle failure. Intensive Care Med 44:774–790. https://doi.org/10.1007/s00134-018-5172-2
Harjola V-P, Mebazaa A, Čelutkienė J et al (2016) Contemporary management of acute right ventricular failure: a statement from the Heart Failure Association and the Working Group on Pulmonary Circulation and Right Ventricular Function of the European Society of Cardiology. Eur J Heart Fail 18:226–241. https://doi.org/10.1002/ejhf.478
Lahm T, Douglas IS, Archer SL et al (2018) Assessment of right ventricular function in the research setting: knowledge gaps and pathways forward. An official American Thoracic Society Research Statement. Am J Respir Crit Care Med 198:e15–e43. https://doi.org/10.1164/rccm.201806-1160ST
Vieillard-Baron A, Matthay M, Teboul JL et al (2016) Experts’ opinion on management of hemodynamics in ARDS patients: focus on the effects of mechanical ventilation. Intensive Care Med 42:739–749. https://doi.org/10.1007/s00134-016-4326-3
Mahjoub Y, Pila C, Friggeri A et al (2009) Assessing fluid responsiveness in critically ill patients: false-positive pulse pressure variation is detected by Doppler echocardiographic evaluation of the right ventricle. Crit Care Med 37:2570–2575. https://doi.org/10.1097/CCM.0b013e3181a380a3
Peters G, Crespo F, Lingras P, Weber R (2013) Soft clustering—fuzzy and rough approaches and their extensions and derivatives. Int J Approx Reason 54:307–322. https://doi.org/10.1016/j.ijar.2012.10.003
Charron C, Vignon P, Prat G et al (2013) Number of supervised studies required to reach competence in advanced critical care transesophageal echocardiography. Intensive Care Med 39:1019–1024. https://doi.org/10.1007/s00134-013-2838-7
Acknowledgements
The authors thank Mr. David Marsh for his English editing and Dr. Ana Catalina Hernandez Padilla for her help in the data management.
Funding
The Hemosepsis study was financially supported by the Programme de Recherche Clinique Inter-régional (academic financial support provided by the French Ministry of Health). The Hemopred study was financially supported by the CIC-P 1435, CHU Limoges.
Author information
Authors and Affiliations
Contributions
GG, PV, AA and AVB designed the study and drafted the manuscript. PV, AA, ALF, CC, SS, XR and AVB collected the data. GG conducted the statistical analysis. AA, ALF, CC, SS and XR carefully revised the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
GG, PV, AU, ALF, CC, SS, XR declared no conflict of interest. AVB has received grant from GSK for conducting clinical research and is a member of the scientific advisory board.
Ethical approval
Both cohorts (Hemosepsis and Hemopred) received Limoges ethics committee approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Geri, G., Vignon, P., Aubry, A. et al. Cardiovascular clusters in septic shock combining clinical and echocardiographic parameters: a post hoc analysis. Intensive Care Med 45, 657–667 (2019). https://doi.org/10.1007/s00134-019-05596-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-019-05596-z