Abstract
Purpose
High-flow nasal cannula (HFNC) therapy is increasingly proposed as first-line respiratory support for infants with acute viral bronchiolitis (AVB). Most teams use 2 L/kg/min, but no study compared different flow rates in this setting. We hypothesized that 3 L/kg/min would be more efficient for the initial management of these patients.
Methods
A randomized controlled trial was performed in 16 pediatric intensive care units (PICUs) to compare these two flow rates in infants up to 6 months old with moderate to severe AVB and treated with HFNC. The primary endpoint was the percentage of failure within 48 h of randomization, using prespecified criteria of worsening respiratory distress and discomfort.
Results
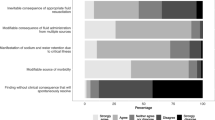
From November 2016 to March 2017, 142 infants were allocated to the 2-L/kg/min (2L) flow rate and 144 to the 3-L/kg/min (3L) flow rate. Failure rate was comparable between groups: 38.7% (2L) vs. 38.9% (3L; p = 0.98). Worsening respiratory distress was the most common cause of failure in both groups: 49% (2L) vs. 39% (3L; p = 0.45). In the 3L group, discomfort was more frequent (43% vs. 16%, p = 0.002) and PICU stays were longer (6.4 vs. 5.3 days, p = 0.048). The intubation rates [2.8% (2L) vs. 6.9% (3L), p = 0.17] and durations of invasive [0.2 (2L) vs. 0.5 (3L) days, p = 0.10] and noninvasive [1.4 (2L) vs. 1.6 (3L) days, p = 0.97] ventilation were comparable. No patient had air leak syndrome or died.
Conclusion
In young infants with AVB supported with HFNC, 3 L/kg/min did not reduce the risk of failure compared with 2 L/kg/min. This clinical trial was recorded on the National Library of Medicine registry (NCT02824744).



Similar content being viewed by others
References
Meissner HC (2016) Viral bronchiolitis in children. N Engl J Med 374:62–72
Franklin D, Babl FE, Schlapbach LJ et al (2018) A randomized trial of high-flow oxygen therapy in infants with bronchiolitis. N Engl J Med 378:1121–1131
Thia LP, McKenzie SA, Blyth TP, Minasian CC, Kozlowska WJ, Carr SB (2008) Randomised controlled trial of nasal continuous positive airways pressure (CPAP) in bronchiolitis. Arch Dis Child 93:45–47
Cambonie G, Milési C, Jaber S et al (2008) Nasal continuous positive airway pressure decreases respiratory muscles overload in young infants with severe acute viral bronchiolitis. Intensive Care Med 34:1865–1872
Essouri S, Durand P, Chevret L et al (2011) Optimal level of nasal continuous positive airway pressure in severe viral bronchiolitis. Intensive Care Med 37:2002–2007
Milési C, Matecki S, Jaber S et al (2013) 6 cmH2O continuous positive airway pressure versus conventional oxygen therapy in severe viral bronchiolitis: a randomized trial. Pediatr Pulmonol 48:45–51
Milési C, Baleine J, Matecki S et al (2013) Is treatment with a high flow nasal cannula effective in acute viral bronchiolitis? A physiologic study. Intensive Care Med 39:1088–1094
Hough JL, Pham TM, Schibler A (2014) Physiologic effect of high-flow nasal cannula in infants with bronchiolitis. Pediatr Crit Care Med 15:e214–e219
Pham TM, O’Malley L, Mayfield S, Martin S, Schibler A (2015) The effect of high flow nasal cannula therapy on the work of breathing in infants with bronchiolitis. Pediatr Pulmonol 50:713–720
Sinha IP, McBride AKS, Smith R, Fernandes RM (2015) CPAP and high-flow nasal cannula oxygen in bronchiolitis. Chest 148:810–823
Milési C, Essouri S, Pouyau R et al (2017) High flow nasal cannula (HFNC) versus nasal continuous positive airway pressure (nCPAP) for the initial respiratory management of acute viral bronchiolitis in young infants: a multicenter randomized controlled trial (TRAMONTANE study). Intensive Care Med 43:209–216
Milési C, Boubal M, Jacquot A et al (2014) High-flow nasal cannula: recommendations for daily practice in pediatrics. Ann Intensive Care 4:29
Essouri S, Laurent M, Chevret L et al (2014) Improved clinical and economic outcomes in severe bronchiolitis with pre-emptive nCPAP ventilatory strategy. Intensive Care Med 40:84–91
Ralston SL, Lieberthal AS, Meissner HC et al (2014) Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics 134:e1474–e1502
Hollman G, Shen G, Zeng L et al (1998) Helium-oxygen improves Clinical Asthma Scores in children with acute bronchiolitis. Crit Care Med 26:1731–1736
Debillon T, Zupan V, Ravault N, Magny JF, Dehan M (2001) Development and initial validation of the EDIN scale, a new tool for assessing prolonged pain in preterm infants. Arch Dis Child Fetal Neonatal Ed 85:F36–F41
Black J, Baharestani MM, Cuddigan J et al (2007) National Pressure Ulcer Advisory Panel’s updated pressure ulcer staging system. Adv Skin Wound Care 20:269–274
O’Driscoll BR, Howard LS, Davison AG, British Thoracic Society (2008) BTS guideline for emergency oxygen use in adult patients. Thorax 63(Suppl 6):vi1–vi68. https://doi.org/10.1136/thx.2008.102947
te Pas AB, Wong C, Kamlin CO, Dawson JA, Morley CJ, Davis PG (2009) Breathing patterns in preterm and term infants immediately after birth. Pediatr Res 65:352–356
Schmalisch G, Wilitzki S, Wauer RR (2005) Differences in tidal breathing between infants with chronic lung diseases and healthy controls. BMC Pediatr 5:36
Ramnarayan P, Schibler A (2017) Glass half empty or half full? The story of high-flow nasal cannula therapy in critically ill children. Intensive Care Med 43:246–249
Abboud PA, Roth PJ, Skiles CL, Stolfi A, Rowin ME (2012) Predictors of failure in infants with viral bronchiolitis treated with high-flow, high-humidity nasal cannula therapy. Pediatr Crit Care Med 13:e343–e349
ten Brink F, Duke T, Evans J (2013) High-flow nasal prong oxygen therapy or nasopharyngeal continuous positive airway pressure for children with moderate-to-severe respiratory distress? Pediatr Crit Care Med 14:e326–e331
Bressan S, Balzani M, Krauss B, Pettenazzo A, Zanconato S, Baraldi E (2013) High-flow nasal cannula oxygen for bronchiolitis in a pediatric ward: a pilot study. Eur J Pediatr 172:1649–1656
Mayfield S, Bogossian F, O’Malley L, Schibler A (2014) High-flow nasal cannula oxygen therapy for infants with bronchiolitis: pilot study. J Paediatr Child Health 50:373–378
Kepreotes E, Whitehead B, Attia J et al (2017) High-flow warm humidified oxygen versus standard low-flow nasal cannula oxygen for moderate bronchiolitis (HFWHO RCT): an open, phase 4, randomised controlled trial. Lancet 389:930–939
Collins CL, Holberton JR, Barfield C, Davis PG (2013) A randomized controlled trial to compare heated humidified high-flow nasal cannulae with nasal continuous positive airway pressure postextubation in premature infants. J Pediatr 162(949–954):e1
Manley BJ, Owen LS, Doyle LW et al (2013) High-flow nasal cannulae in very preterm infants after extubation. N Engl J Med 369:1425–1433
Mauri T, Alban L, Turrini C et al (2017) Optimum support by high-flow nasal cannula in acute hypoxemic respiratory failure: effects of increasing flow rates. Intensive Care Med 43:1453–1463
Hammer J, Numa A, Newth CJ (1997) Acute respiratory distress syndrome caused by respiratory syncytial virus. Pediatr Pulmonol 23:176–183
Lee JH, Rehder KJ, Williford L, Cheifetz IM, Turner DA (2013) Use of high flow nasal cannula in critically ill infants, children, and adults: a critical review of the literature. Intensive Care Med 39:247–257
Frizzola M, Miller TL, Rodriguez ME et al (2011) High-flow nasal cannula: impact on oxygenation and ventilation in an acute lung injury model. Pediatr Pulmonol 46:67–74
Yoder BA, Stoddard RA, Li M, King J, Dirnberger DR, Abbasi S (2013) Heated, humidified high-flow nasal cannula versus nasal CPAP for respiratory support in neonates. Pediatrics 131:e1482–e1490
Kugelman A, Riskin A, Said W, Shoris I, Mor F, Bader D (2015) A randomized pilot study comparing heated humidified high-flow nasal cannulae with NIPPV for RDS. Pediatr Pulmonol 50:576–583
Betters KA, Hebbar KB, McCracken C, Heitz D, Sparacino S, Petrillo T (2017) A novel weaning protocol for high-flow nasal cannula in the PICU. Pediatr Crit Care Med 18:e274–e280
Acknowledgements
Members of the GFRUP Respiratory Study Group contributed substantially to the study design, data interpretation, manuscript revision, and final approval. The Group includes, in addition to the authors of the manuscript, the following members: Guillaume Emeriaud, MD, PhD (Division of Pediatric Critical Care, Department of Pediatrics, Sainte-Justine University Hospital, University of Montréal, Montréal, QC, Canada); Philippe Jouvet, MD, PhD (Division of Pediatric Critical Care, Department of Pediatrics, Sainte-Justine University Hospital, University of Montréal, QC, Canada); Marti Pons Odena, MD, PhD (Pediatric Intensive Care Unit, Hospital Universitario Sant Joan de Deu University Hospital, Barcelona, Spain); Florent Baudin, MD (Pediatric Intensive Care Unit, Women-Mothers & Children’s University Hospital, Lyon, France); Chloe Genier, GN (Pediatric Intensive Care Unit, Women & Children’s University Hospital, Nantes, France); and Ingrid Nissen, MD (Pediatric Intensive Care Unit, St. Olav's University Hospital, Trondheim, Norway).
Funding
All phases of this study were supported by the University Hospital Center of Montpellier (Grant: research contract 2012–2015).
Author information
Authors and Affiliations
Consortia
Contributions
CM, JB, SD, and GC conceptualized and designed the study, coordinated and supervised the data collection at their respective investigation sites, drafted the initial manuscript, and approved the final manuscript as submitted. AD carried out the initial analyses, reviewed and revised the manuscript, and approved the final manuscript as submitted. AFP, AD, RP, JML, CG, ASG, JR, AM, MA, JG, MG, TM, JB, FM, MOM, PD, SD, EJ, AP, SL, OB, and SR coordinated and supervised the data collection at their respective investigation sites, critically reviewed the manuscript, and approved the final manuscript as submitted. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no financial relationships and no potential conflicts of interest relevant to this article to disclose.
Additional information
The members of the GFRUP Respiratory Study Group are listed in the Acknowledgements.
Rights and permissions
About this article
Cite this article
Milési, C., Pierre, AF., Deho, A. et al. A multicenter randomized controlled trial of a 3-L/kg/min versus 2-L/kg/min high-flow nasal cannula flow rate in young infants with severe viral bronchiolitis (TRAMONTANE 2). Intensive Care Med 44, 1870–1878 (2018). https://doi.org/10.1007/s00134-018-5343-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-018-5343-1