Abstract
Purpose
To assess the feasibility, image quality, diagnostic accuracy, therapeutic impact and tolerance of diagnostic and hemodynamic assessment using a novel miniaturized multiplane transesophageal echocardiography (TEE) probe in ventilated ICU patients with cardiopulmonary compromise.
Study design
Prospective, descriptive, single-center study.
Methods
Fifty-seven ventilated patients with acute circulatory or respiratory failure were assessed, using a miniaturized multiplane TEE probe and a standard TEE probe used as reference, randomly by two independent experienced operators. Measurements of hemodynamic parameters were independently performed off-line by a third expert. Diagnostic groups of acute circulatory failure (n = 5) and of acute respiratory failure (n = 3) were distinguished. Hemodynamic monitoring was performed in 9 patients using the miniaturized TEE probe. TEE tolerance and therapeutic impact were reported.
Results
The miniaturized TEE probe was easier to insert than the standard TEE probe. Despite lower imaging quality of the miniaturized TEE probe, the two probes had excellent diagnostic agreement in patients with acute circulatory failure (Kappa: 0.95; 95 % CI: 0.85–1) and with acute respiratory failure (Kappa: 1; 95 % CI: 1.0–1.0). Accordingly, therapeutic strategies derived from both TEE examinations were concordant (Kappa: 0.82; 95 % CI: 0.66–0.97). The concordance between quantitative hemodynamic parameters obtained with both TEE probes was also excellent. No relevant complication secondary to TEE probes insertion occurred.
Conclusions
Hemodynamic assessment of ventilated ICU patients with cardiopulmonary compromise using a miniaturized multiplane TEE probe appears feasible, well-tolerated, and relevant in terms of diagnostic information and potential therapeutic impact. Further larger-scale studies are needed to confirm these preliminary results.
Similar content being viewed by others
Introduction
Echocardiography has become a first-line imaging modality for the hemodynamic assessment of patients admitted to the intensive care unit (ICU) with severe cardiopulmonary diseases [1]. Particularly in mechanically ventilated ICU patients, transesophageal echocardiography (TEE) has greater diagnostic capability and therapeutic impact, when compared to transthoracic echocardiography (TTE) [2]. In addition, TEE allows hemodynamic monitoring in real time to assess both the efficacy and tolerance of acute therapeutic changes in unstable ventilated patients [3]. In patients with septic shock, the most common cause of circulatory failure in the ICU [4], TEE provides crucial information to aid the intensivist in the management of these unstable patients [5]. Recent international recommendations from Scientific Societies of Critical Care Medicine have defined how to achieve competence in basic and advanced critical care echocardiography (CCE) which is mainly performed in ICU settings in patients with cardiopulmonary compromise [1, 6, 7].
A single-use indwelling TEE monoplane probe has been recently successfully used in ventilated ICU patients for the serial assessment of cardiopulmonary compromise [8]. Potential advantages of miniaturized TEE probes are facilitated insertion and improved tolerance, which can enable their use for hemodynamic monitoring in unstable ventilated patients [9]. The diagnostic accuracy and therapeutic impact of miniaturized multiplane TEE probes have been scarcely reported, while their use in ventilated ICU patients has not yet been evaluated. Accordingly, we sought to prospectively assess the feasibility, diagnostic accuracy, therapeutic impact and tolerance of diagnostic assessment and hemodynamic monitoring performed using a miniaturized multiplane TEE probe in ventilated ICU patients with severe cardiopulmonary compromise. Preliminary results of the current study have been previously published in an abstract form [10].
Methods
We routinely use echocardiography as a first-line modality for the hemodynamic assessment of ventilated patients with acute circulatory or respiratory failure [2]. Serial TEE assessments, and potentially prolonged examination when deemed indicated by the attending physician [8], constitute the standard of care in our medical-surgical ICU for hemodynamic monitoring. Accordingly, this observational prospective study was accepted by our local Ethics Committee which waived the need for informed consent, and the absence of opposition to participate in this study was orally obtained from the patient or his relatives [11].
Patients
Mechanically ventilated adult patients who required hemodynamic assessment for acute circulatory or respiratory failure were eligible. Acute circulatory failure was defined as sustained hypotension (systolic arterial pressure <90 mmHg or mean arterial pressure <65 mmHg) associated with clinical signs (oliguria <0.5 ml/kg/h for more than 3 h, skin mottling, encephalopathy) and biological signs (pH < 7.38 and base excess >−4 mmol/L, lactate >2 mmol/L, ScvO2 <70 %) of tissue hypoperfusion [12]. Acute respiratory failure was defined as acute onset of respiratory signs associated with radiological infiltrates and hypoxemia reflected by a PaO2/FiO2 ≤300. Patients with contra-indications for TEE were excluded [13]. Demographic characteristics, reasons for ICU admission, and Simplified Acute Physiological Score (SAPS) II [14] were recorded.
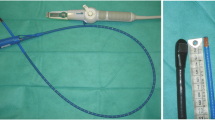
Transesophageal echocardiography
Patients successively underwent two TEE examinations: one using a standard multiplane probe (diameter: 10 mm, 7.5 MHz) and a second one using a miniaturized multiplane probe (size of the digital sensor: 7.5 × 5.5 mm; diameter endoscope shaft: 5.2 mm; multifrequency 3–8 MHz; phased-array 32-element probe). The two TEE probes were successively connected to the same upper-end platform (iE33; Philips Healthcare) (Fig. 1). The miniaturized TEE probe has two-dimensional imaging, color Doppler mapping and spectral Doppler capabilities, but no tissue Doppler imaging. TEE examinations were performed independently by two distinct intensivists with expertise in CCE, in random order according to operators’ availability, and immediately one following the other. Investigators used the standard or the miniaturized TEE probe interchangeably. TEE probes were inserted blindly after an intravenous bolus of 5 mg of Midazolam. If unsuccessful after a single attempt, muscle paralysis was performed in order to enable a laryngoscope-guided esophageal insertion with an injection of 50 mg of vecuronium bromide. Since the second TEE examination was performed immediately after the first, additional sedation was not required. During this period, all patients had stabilized hemodynamic status and no therapeutic changes were therefore initiated. Single-use protection sheaths were only used with the traditional TEE probe, as a standard of care, and the gastric tubes were temporarily removed when necessary to improve the contact between the tip of the esophageal probe and the esophageal mucosa. TEE examinations included two-dimensional imaging of the heart and great vessels, color Doppler mapping and spectral Doppler interrogation of the mitral valve, aortic valve, main pulmonary artery and left upper pulmonary vein. Two-dimensional imaging quality was ranged as follows: 0, when no images were obtained; poor, 1, when less than 50 % of the ventricular borders were visualized; good, 2, when more than 50 % of the ventricular borders were visualized; and excellent, 3, when all ventricular borders were visualized [15]. Color and spectral Doppler grading was as follows: 0, when no Doppler signal was obtained; poor, 1, when a partial Doppler signal was obtained; good, 2, when a full Doppler signal was obtained.
Each operator interpreted the TEE examination in real-time and proposed therapeutic changes on a dedicated clinical research form at the bedside. Only the information derived from the standard TEE examination was used for patient’s care. Acute circulatory failure was related to one of the five following mechanisms: (1) preload-dependence when the superior vena cava (SVC) collapsibility index was >36 % [16]; (2) left ventricular (LV) dysfunction when LV ejection fraction (LVEF) was <40 % in the absence of preload-dependence [5]; (3) acute cor pulmonale when the right ventricular (RV) end-diastolic area (RVEDA) and LV end-diastolic area (LVEDA) ratio was >0.6 and associated with the presence of paradoxical septal motion [17]; (4) tamponade when a large, circumferential pericardial effusion was associated with the diastolic compression of right cardiac cavities [18] or in the presence of a compressive mediastinal hematoma [19]; or (5) vasoplegia when none of these abnormalities were present in a hypotensive patient [20]. Acute respiratory failure was related to one of the following three mechanisms: (1) cardiogenic pulmonary edema in the presence of increased LV filling pressures reflected by a lateral E/E’ ratio >14 [21] regardless of LVEF value, and underlying heart disease known to be associated with LV diastolic dysfunction [22]; (2) ARDS in the presence of a lateral E/E’ ratio <8 [23], normal left heart [24] and potentially associated acute cor pulmonale [25]; or (3) acute massive left valvular regurgitation. Acute massive mitral insufficiency was defined by the presence of a regurgitant flow color Doppler area >8 cm2, a mitral E wave >1.5 m/s, a blurred or reversed S pulmonary vein wave, and a non-dilated LV with preserved LVEF [26]. Acute massive aortic insufficiency was defined by the presence of a regurgitant flow extending to the LV apex using color Doppler mapping, a maximal aortic Doppler velocity >2 m/s, and a non-dilated LV with preserved LVEF [26]. In the presence of combined cardiopulmonary compromise, the distinct leading mechanism of each organ failure was identified in the same patient.
In patients who required serial hemodynamic assessments, the decision to use the miniaturized TEE probe to monitor the effects of therapeutic changes was left to the discretion of the attending physician. To assess TEE tolerance, hemodynamic events (arrhythmias, increase of systolic blood pressure >30 mmHg or hypotension <95 mmHg), respiratory events (arterial desaturation in oxygen <90 %, aspiration) and digestive complications (vomiting, oropharyngeal bleeding) were systematically screened [9, 27].
Off-line measurements
Images were recorded and stored in digital format for off-line measurement of quantitative hemodynamic parameters by a third independent investigator who was not involved in the study, had expertise in echocardiography, and was blinded to the patients’ clinical data. Hemodynamic parameters were not measured in a paired fashion but rather successively on images recorded with the standard TEE probe, and subsequently on images obtained with the miniaturized TEE probe. Images were not anonymized since their origin was easily identifiable on a screen display. The following measurements were performed in triplicate and averaged: SVC collapsibility index [16], RVEDA/LVEDA [17] and LVEF using the monoplane modified Simpson’s rule [28], LV eccentricity index at end-systole [29] and LV fractional area change (LVFAC), mitral Doppler E/A ratio, E wave deceleration time, pulmonary vein S/D ratio and systolic fraction [30], LV outflow tract (LVOT) area and end-expiratory velocity–time integral (VTI) of LVOT Doppler flow to obtain LV stroke volume and cardiac output [31]. E’ maximal velocity was measured on the lateral mitral annulus using TTE in all patients [32].
Statistical analysis
Continuous variables were expressed as means ± standard deviations and qualitative variables were expressed as percentages. Quantitative parameters were compared using the Student’s t test or the Wilcoxon rank sum test according to data distribution, and proportions were compared using the chi-squared test or Fisher’s exact test, when necessary. The agreement of diagnostic groups and therapeutic proposals derived from the two TEE examinations was assessed using the Cohen’s Kappa coefficient and its 95 % confidence intervals (CI) [33]. The concordance of measurements of hemodynamic indices performed on images acquired with the standard and the miniaturized TEE probes was assessed using the intraclass correlation coefficient and its 95 % CI [34]. In addition, the mean difference (estimated bias) between the values of hemodynamic parameters obtained with the miniaturized TEE probe and the standard TEE probe, used as reference, and the 95 % confidence intervals (±1.96 standard deviation of the difference) were determined using the Blant–Altman method [35]. A p value < 0.05 was considered statistically significant.
Results
Of 62 eligible patients, 5 were excluded due to contra-indication for TEE (n = 4) or a moribund status (n = 1). Finally, 57 ventilated patients were studied (39 men; age: 66 ± 11 years; SAPS II: 51 ± 15; body mass index: 27 ± 7 kg/m2; tidal volume: 450 ± 51 mL; positive end-expiratory pressure: 7 ± 3 cmH2O; plateau pressure: 21 ± 4 cmH2O; PaO2/FiO2: 194 ± 106). Patients were admitted to the ICU for septic shock (n = 17), resuscitated cardiac arrest (n = 13), shock after cardiac surgery (n = 6), ARDS (n = 5), severe sepsis due to a pneumonia (n = 2), acute pulmonary edema (n = 6), and other reasons (n = 8). No exacerbation of chronic obstructive pulmonary disease was noted. At the time of TEE assessment, 40 patients (70 %) were under vasopressor and mean lactate level was 4.2 ± 3.5 mmol/L. ICU mortality was 33 %.
No insertion failure of TEE probes was reported. Esophageal insertion of the miniaturized TEE probe less frequently required a laryngoscopic guidance than the standard TEE probe (26/57 vs. 57/57, p < 0.0001) and tended to require less use of additional sedation and muscle relaxant agents (23/57 vs. 33/57; p = 0.09). Mean durations of echocardiographic examinations were similar irrespective of TEE probe used (12 ± 4 vs. 12 ± 5 min, p = 1). Two-dimensional imaging, color Doppler mapping, and spectral Doppler signal were significantly better with the standard TEE probe, as reflected by a greater proportion of patients with good-to-excellent image quality (49/57 vs. 29/57, p < 0.0001; 37/57 vs. 22/57, p = 0.008; 36/57 vs. 24/57, p = 0.04, respectively). Measurement feasibility was therefore lower for certain commonly used hemodynamic parameters, such as LVEF, LVFAC, RVEDA/LVEDA ratio, and LVOT VTI (Table 1). When images recorded with the miniaturized TEE probe were suitable for quantitative assessment and values compared to those obtained with standard TEE probe, the mean bias was uniformly low and 95 % limits of agreement were narrow and useful for clinical use (Supplementary Table 1). Accordingly, the concordance between quantitative hemodynamic parameters independently measured on still-images obtained with both TEE probes was excellent, as reflected by the high intra-class correlation coefficients obtained (Table 1).
The agreement for the diagnostic classification of acute circulatory and respiratory failure using the miniaturized and the standard TEE probes was excellent, as shown by a Kappa coefficient of 0.95 (95 % CI: 0.85–1.0) and 1.0 (95 % CI: 1.0–1.0), respectively. In a single patient with shock, the miniaturized TEE probe did not allow the operator to identify relevant hypovolemia due to inadequate imaging quality. In 33 patients (58 %), the standard TEE provided relevant additional information regarding the cause of the circulatory or respiratory failure: infective endocarditis (n = 4), ruptured papillary muscle (n = 1), hypertrophic cardiomyopathy (n = 5), regional wall motion abnormality secondary to an acute myocardial infarction (n = 5). None of these diagnoses was missed using the miniaturized TEE probe which otherwise yielded no false positive results (Fig. 2). Therapeutic proposals resulting from bedside interpretation of TEE examinations are summarized in Table 2. Although overall agreement was excellent (Kappa: 0.82; 95 % CI: 0.66–0.97), inter-observer discrepancies were observed for almost all therapeutic proposals, including the indication for prompt cardiac valve surgery (Table 2).
Two illustrative examples of acute massive mitral regurgitations identified using the miniaturized multiplane TEE probe in patients requiring mechanical ventilation for hypoxic acute pulmonary edema. In the first patient, ruptured anterolateral papillary muscle was depicted in the four-chamber view both at end-systole (upper left panel, arrow) and at end-diastole (middle left panel, arrow) and resulted in a massive, acute, excentric mitral regurgitation (lower left panel, arrow). In the second patient, a large and mobile vegetation was evidenced in the four-chamber view (upper right panel, arrow). Acute mitral endocarditis was complicated by a massive, excentric mitral regurgitation clearly depicted by color Doppler mapping (middle right panel, arrow). A reversal of systolic Doppler wave was evidenced in the upper-left pulmonary vein (lower right panel, arrows). LA left atrium, LV left ventricle, RA right atrium, RV right ventricle
Nine patients (15 %) underwent hemodynamic monitoring using the miniaturized TEE probe. Mean monitoring duration was 72 min (range: 7–120 min). Indications were: severe hypovolemia (n = 6), major LV dysfunction resulting in low cardiac output (n = 1), and ARDS-induced acute cor pulmonale (n = 2) (Fig. 3). No complication attributable to the use of the miniaturized TEE probe was reported, even during the periods of hemodynamic monitoring, whereas 4 mild complications were observed when using the standard TEE probe (oropharyngeal bleeding: n = 1; transient high blood pressure: n = 3) (p = 0.12).
Hemodynamic monitoring using the miniaturized multiplane TEE probe in a ventilated patient presenting with shock. At baseline, end-diastolic left ventricular cavity size assessed in the transgastric short-axis view was reduced (upper left panel) and became virtual during systole, as depicted by M-mode tracing (upper middle panel). This severe hypovolemia resulted in a significantly decrease left ventricular stroke volume reflected by a decreased outflow tract velocity time integral (upper right panel). Serial fluid challenges progressively increased left ventricular preload (middle and lower left panels), reversed the systolic obliteration of left ventricular cavity (middle and lower middle panels), and resulted in larger stroke volumes (middle and lower right panels). LV left ventricle, VTI velocity–time integral of left ventricular outflow tract
Discussion
The present study showed the feasibility, diagnostic capability, therapeutic impact and tolerance of hemodynamic assessment and monitoring using a miniaturized multiplane TEE probe in ICU ventilated adult patients sustaining an acute circulatory or respiratory failure. Data were compared with information obtained with a standard TEE, which was used as the reference standard. As expected, the miniaturized TEE probe was easier to insert orally than the standard esophageal probe, as reflected by a less frequent need for laryngoscopic guidance and use of muscle paralysis agents. This result may partially be explained by our routine use of laryngoscopic guidance for esophageal insertion of a standard TEE probe after a single failure of blinded insertion in order to reduce the risk of injury. Similar results were previously reported by Spencer et al. [9] who used a similar miniaturized monoplane TEE probe in spontaneously ventilated cardiology patients, reporting no failure of oral intubation, whereas the examination using a standard TEE probe was not possible in three cases. We also recently reported an easy esophageal insertion of a miniaturized single-use monoplane TEE probe in ventilated ICU patients [8]. In the present study, no clinically relevant complications were observed even when the miniaturized multiplane TEE probe was used for hemodynamic monitoring. Spencer et al. [9] also reported a good tolerance with the miniaturized TEE probe in spontaneously breathing patients, even when inserted trans-nasally. Nevertheless, gastric and oral lesions have been described after prolonged esophageal insertion of a miniaturized TEE probe for the purpose of hemodynamic monitoring [8]. Both the duration of esophageal insertion and TEE probe characteristics, such as probe stiffness and distal tip design, may play a role in the development of mucosal injuries [8]. Although it has been shown that the prolonged insertion (up to 12 h) of a standard TEE probe in dogs generated esophageal pressure <10 mmHg without gross or microscopic damage to the esophageal mucosae on pathologic examination [36], TEE is currently neither used for nor considered as a true long-term hemodynamic monitoring system. Nevertheless, the miniaturized TEE probe tested here appears safe for a prolonged insertion in sedated ICU patients under ventilator who require hemodynamic monitoring.
Although the miniaturized multiplane TEE probe tested in the present study yielded significantly lower two-dimensional and Doppler imaging quality when compared to a standard TEE probe, it allowed accurate identification of the leading mechanism of the acute circulatory or respiratory failure in our ICU patients, as reflected by an excellent diagnostic agreement between the two independently conducted examinations. Similarly, the concordance of quantitative measurements was excellent, as demonstrated by high intraclass correlation coefficients. Nevertheless, certain commonly used hemodynamic parameters could not be measured in up to one-third of the patients, and all measurements were performed off-line by an expert in critical care TEE [1]. This may have positively influenced the accuracy of performed measurements on still frames of lower quality obtained by the miniaturized TEE probe, and the present results should therefore not be extrapolated to less experienced operators. Similarly, both the acquisition and on-line interpretation of TEE examinations by experts in CCE presumably explain the absence of false negative results when using the miniaturized TEE probe, including acute infective endocarditis or ruptured papillary muscle, and the excellent agreement of therapeutic proposals irrespective of the type of esophageal probe used. Importantly, we used simple yet robust diagnostic criteria to identify hemodynamic profiles, while more subtle and relevant findings could be missed by the miniaturized TEE probe due to lower image quality.
The miniaturized TEE probe used in the present study has been previously used successfully in the setting of pediatric cardiac surgery [37–40]. No major complications were encountered and the TEE examination yielded clinically relevant information, including immediate re-intervention due to unsatisfactory surgical results [38]. These results were confirmed by other clinical studies performed in the peri-operative settings [39, 40]. Interestingly, degradation of imaging quality was reported in larger infants, typically >10 kg [38, 39]. These results are in keeping with the inferior overall quality of images provided by the miniaturized multiplane TEE probe in our adult patients, when compared to standard TEE. Spencer et al. [9] reported an accurate identification of valvular, cardiac or aortic abnormalities using the miniaturized probe in a population of 128 awake patients referred for a TEE examination to an echocardiography laboratory. As far as we know, two types of miniaturized TEE probes are currently available. Although of slightly larger size, the miniaturized TEE probe used in the present study has the advantage of providing multiplane scanning and having color and spectral Doppler capabilities. As such, it allows measurement of a large panel of parameters useful for the hemodynamic assessment of ventilated ICU patients with cardiopulmonary compromise. The other miniaturized TEE probe is of even smaller size (diameter: 5.5 mm), Federal Drug Agency-approved and European Community-marked for 72 h of continuous use, and is single-use, but it only allows monoplane scanning and has no spectral Doppler capabilities [8]. Measurements are limited to distances and surfaces on two-dimensional images. Accordingly, this type of miniaturized probe appears adequately suited only for qualitative or semi-quantitative diagnostic approaches [8], as previously validated in septic shock patients [41]. In contrast, the miniaturized multiplane TEE probe tested in the present study promises to become an alternative to the use of standard probes for diagnostic but also monitoring purposes, providing further improvement in image quality.
The present study suffers from several limitations. TEE images were acquired and interpreted by two independent experienced intensivists who had expertise in CCE. Accordingly, the present results obtained with the miniaturized TEE probe cannot be extrapolated to less experienced operators [7]. Two methodological aspects potentially biased our results towards concordance: the absence of anonymization of echocardiographic images and the successive, rather than random, measurement of hemodynamic parameters on images recorded with the standard and miniaturized TEE probes. Only a few of our ventilated patients were monitored using the miniaturized probe, and the duration of hemodynamic monitoring was shorter than that previously reported when using single-use monoplane miniaturized TEE probes [8]. In addition, systematic examination for potential oral or esophageal mucosa injury was not performed. Accordingly, further studies are required in larger sample sizes before incorporating this promising tool into routine clinical practice as a safe hemodynamic monitoring for unstable ventilated ICU patients. Finally, the impact of therapeutic changes related to TEE assessment on patient outcome was not assessed.
Conclusion
Hemodynamic assessment of ICU ventilated patients with acute circulatory or respiratory failure is easily performed using the miniaturized multiplane TEE probe tested here. When the image quality provided by the miniaturized TEE probe is suitable for interpretation and measurements, derived diagnoses and resulting therapeutic proposals are highly concordant with those obtained with the use of standard TEE. In experienced hands, this new miniaturized multiplane TEE probe promises to be of value as an alternative diagnostic tool for the assessment of ventilated patients with cardiopulmonary compromise, providing substantial improvements in image quality. Additional studies are required to confirm the clinical value and safety of miniaturized multiplane TEE probe for the hemodynamic monitoring of unstable ICU patients.
References
Mayo PH, Beaulieu Y, Doelken P, Feller-Kopman D, Harrod C, Kaplan A et al (2009) American College of Chest Physicians/La SRLF. Statement on competence in critical care ultrasonography. Chest 135:1050–1060
Vignon P, Mentec H, Terré S, Gastinne H, Guéret P, Lemaire F (1994) Diagnostic accuracy and therapeutic impact of transthoracic and transesophageal echocardiography in mechanically ventilated patients in the ICU. Chest 106:1829–1834
Vignon P (2005) Hemodynamic assessment of critically ill patients using echocardiography Doppler. Curr Opin Crit Care 11(3):227–234
De Baker D, Biston P, Devriendt J, Madl C, Chochrad D, Aldecoa C et al (2010) Comparison of dopamine and norepinephrine in the treatment of shock. N Engl J Med 362:779–789
Boufferrache K, Amiel JB, Chimot L, Caille V, Charron C, Vignon P et al (2012) Initial ressuscitation guided by the surviving sepsis campaign recommendations and early echocardiography assessment of hemodynamics in intensive care unit septic patients: a pilot study. Crit Care Med 40(10):2821–2827
Expert roundtable on ultrasound in ICU (2011) International expert statement on training standards for critical care echocardiography. Intensive Care Med 37:1077–1083
Expert Round Table on Echocardiography in ICU (2014) International consensus statement on training standards for advanced critical care echocardiography. Intensive Care Med 40:654–666
Vieillard-Baron A, Slama M, Mayo O, Charrou C, Amiel JB, Esterez C et al (2013) A pilot study on safety and clinical utility of a single-use 72-hour indwelling transesophageal echocardiography probe. Intensive Care Med 39:629–635
Spencer KT, Krauss D, Thurn J, Mor-Avi V, Poppas A, Vignon P et al (1997) Transnasal transesophageal echocardiography. J Am Soc Echocardiogr 10:728–737
Vignon P, Amiel JB, François B, Clavel M, Pichon N, Dugard A et al (2011) Evaluation of a miniaturized TEE probe in ventilated ICU patients. Preliminary results. Intensive Care Med 37(Suppl. 1):S242
Kompanje EJ, Maas AI, Menon DK, Kesecioglu J (2014) Medical research in emergency research in the European Union member states: tensions between theory and practice. Intensive Care Med 40:496–503
Antonelli M, Levy M, Andrews PJ, Chastre J, Hudson LD, Manthous C et al (2007) Hemodynamic monitoring in shock and implications for management. International Consensus Conference, Paris, France, 27–28 April 2006. Intensive Care Med 33:575–590
Vignon P, Mayo P (2011) Echocardiography in the critically ill: an overview. In: De Baker D, Cholley B, Slama M, Vieillard-Baron A, Vignon P (eds) Hemodynamic monitoring using echocardiography in the critically ill. Springer, Berlin, pp 1–9
Le Gall JR, Lemeshow S, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Vignon P, Chastagner C, François B, Normand S, Bonnivard M, Gastinne H (2003) Diagnostic ability of hand-held echocardiography in ventilated critically ill patients. Crit Care 7:R84–R91
Vieillard-Baron A, Chergui K, Rabiller A, Peyrouset O, Page B, Beauchet A et al (2004) Superior vena caval collapsibility as a gauge of volume status in ventilated septic patients. Intensive Care Med 30:1734–1739
Jardin F, Dubourg O, Bourdarias JP (1997) Echocardiographic pattern on acute cor pulmonale. Chest 111:209–217
Ward PR, Lang RM (2011) Pericardial tamponade. In: Lang RM, Goldstein SA, Kronzon I, Khandheria BK (eds) Dynamic echocardiography. Saunders, Saint Louis, pp 250–253
Grümann A, Baretto L, Dugard A, Morera P, Cornu E, Amiel JB et al (2012) Localized cardiac tamponade after open-heart surgery. Ann Thorac Cardiovasc Surg 18:524–529
Vignon P, Slama M (2011) Diagnosing the mechanisms of circulatory failure. In: De Baker D, Cholley B, Slama M, Vieillard-Baron A, Vignon P (eds) Hemodynamic monitoring using echocardiography in the critically ill. Springer, Berlin, pp 99–107
Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM et al (2000) Clinical utility of doppler echocardiography and tissue doppler imaging in the estimation of left ventricular filling pressures. Circulation 102:1788–1794
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA et al (2009) Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr 10:165–193
Vignon P, Ait Hassain A, François B, Preux PM, Pichon N, Clavel M et al (2008) Non invasive assessment of pulmonary artery occlusion pressure in ventilated patients: a transesophageal study. Crit Care 12:R18
The ARDS Definition Task Force (2012) Acute respiratory distress syndrom: the Berlin definition. JAMA 307:2526–2533
Lhéritier G, Legras A, Caille A, Lherm T, Mathonnet A, Frat JP et al (2013) Prevalence and prognostic value of acute cor pulmonale and patent foramen ovale in ventilated patients with early acute respiratory distress syndrome. A multicenter study. Intensive Care Med 39:1734–1742
Sohn J, Hollenberg SM (2011) Cardiogenic Shock Associated with Acute Left-Heart Failure. In: De Baker D, Cholley B, Slama M, Vieillard-Baron A, Vignon P (eds) Hemodynamic monitoring using echocardiography in the critically ill. Springer, Berlin, pp 117–131
Huttemann E, Schelenz C, Kara F, Chatzinikolaou K, Reinhart K (2004) The use of transesophageal echocardiography in the general ICU – a minireview. Acta Anaesthesiol Scand 48:827–836
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellika PA et al (2015) Recommendations for chamber quantification. J Am Soc Echocardiogr 28:1–39
Ryan T, Petrovic O, Dillon JC, Feigenbaum H, Conley MJ, Armstrong WF (1985) An echocardiographic index for separation of right ventricular volume and pressure overload. J Am Coll Cardiol 5:918–927
Kuecherer HF, Muhiudeen IA, Kusumoto FM, Lee E, Moulinier LE, Cahalan MK et al (1990) Estimation of mean left atrial pressure from transesophageal pulsed Doppler echocardiography of pulmonary venous flow. Circulation 82:1127–1139
Zoghbi WA, Quinones MA (1986) Determination of cardiac output by Doppler echocardiography: a critical appraisal. Herz 11:258–268
Vignon P, Allot V, Lesage J, Martaillé JF, Aldigier JC, François B et al (2007) Diagnosis of left ventricular diastolic dysfunction in the setting of acute changes in loading conditions. Crit Care 11:R43
Bloch DA, Kraemer HC (1989) 2 x 2 kappa coefficients: measures of agreement or association. Biometrics 45:269–287
Fermanian J (1984) Measurement of agreement between 2 judges. Qualitative cases. Rev Epidemiol Sante Publ 32:140–147
Blant JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Urbanowicz JH, Kernoff RS, Oppenheim G, Parnagian E, Billingham ME, Popp RL (1990) Transesophageal echocardiography and its potential for esophageal damage. Anesthesiology 72:40–43
Ferns S, Komarlu R, Van Bergen A, Multani K, Wei Cui V, Robertson DA (2012) Transesophageal echocardiography in critically ill acute postoperative infants: comparison of AcuNav intracardiac echocardiographic and microTEE miniaturized transducers. J Am Soc Echocardiogr 25:874–881
Scohy TV, Gommers D, Jan Derk, ten Harkel A, Deryck Y, McGhie J, Bogers AdJJC (2007) Intraoperative evaluation of micromultiplane transesophageal echocardiographic probe in surgery for congenital heart disease. Eur J Cardiol 8:241–246
Pushparajah K, Miller OI, Rawlins D, Barlow A, Nugent K, Simpson JM (2012) Clinical application of a micro multiplane transesophageal probe in congenital cardiac disease. Cardiol Young 22:170–177
Zyblewski SC, Shirali GS, Forbus GA, Hsia TY, Bradley SM, Atz AM et al (2010) Initial experience with a miniaturized multiplane transesophageal probe in small infants undergoing cardiac operations. Ann Thorac Surg 89:1990–1994
Vieillard-Baron A, Charron C, Chergui K, Peyrouset O, Jardin F (2006) Bedside echocardiographic evaluation of hemodynamics in sepsis: is a qualitative evaluation sufficient? Intensive Care Med 32:1547–1552
Acknowledgments
PV takes responsibility for the content of the manuscript, including the data and analysis. EB and PV: designed the study; acquired and interpreted the data; drafted and revised the manuscript. CE, MC, NP, BF: acquired the data; revised the manuscript. FD and RL: interpreted the data; revised the manuscript. All authors approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The miniaturized multiplane probe was lent by Philips Healthcare, which was not involved in data acquisition and analysis and did not take part in the manuscript drafting.
Additional information
Take-home message: Hemodynamic assessment of ventilated ICU patients with cardiopulmonary compromise using a miniaturized multiplane TEE probe appears feasible, well tolerated, and relevant in terms of diagnostic information and potential therapeutic impact.
Electronic supplementary material
Below is the link to the electronic supplementary material.
134_2015_3998_MOESM1_ESM.pdf
Supplementary material 1: Blant-Altman plots depicting estimated bias and 95 % limits of agreement of comparisons of hemodynamic parameters measured with the miniaturized TEE probe and the standard TEE probe used as reference. (PDF 200 kb)
Rights and permissions
About this article
Cite this article
Begot, E., Dalmay, F., Etchecopar, C. et al. Hemodynamic assessment of ventilated ICU patients with cardiorespiratory failure using a miniaturized multiplane transesophageal echocardiography probe. Intensive Care Med 41, 1886–1894 (2015). https://doi.org/10.1007/s00134-015-3998-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-3998-4