Abstract
Purpose
The aims of this focused review of the literature on children surviving critical illness were to (1) determine whether health-related quality of life (HRQL) represents a clinically meaningful outcome measure for children surviving critical illness and (2) evaluate the HRQL measures implemented in pediatric critical care studies to date.
Methods
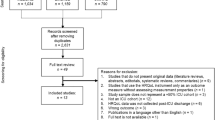
This was a focused review of the literature from 1980 to 2015 based on a search of EMBASE/PubMed, MEDLINE and PsycInfo assessing trends and determinants of HRQL outcomes in children surviving critical illness. We also evaluated the psychometric properties of the HRQL instruments used in the studies identified by examining each measure’s reported reliability, validity and sensitivity to clinical change.
Results
The literature search identified 253 pediatric articles for potential inclusion in the review, among which data from 78 studies were ultimately selected for inclusion. Of the 22 measures utilized in the studies reviewed, only four demonstrated excellent psychometric properties for use in pediatric critical care trials. Trends in HRQL identified in the studies reviewed suggest significant ongoing morbidity for children surviving critical illness. Key determinants of poor HRQL outcomes include reason for PICU admission (sepsis, meningoencephalitis, trauma), antecedents (chronic comorbid conditions), treatments received (prolonged cardiopulmonary resuscitation, long-stay patients, invasive technology), psychological outcomes (post-traumatic stress disorder, parent anxiety/depression) and social and environmental characteristics (low socioeconomic status, parental education and functioning).
Conclusions
Validated pediatric HRQL instruments are now available. Significant impact on HRQL has been demonstrated in acute and acute on chronic critical illness. Future pediatric critical care interventional trials should include both mortality as well as long-term HRQL measurements to truly ascertain the full impact of critical illness in children.



Similar content being viewed by others
References
Conlon NP, Breatnach C, O’Hare BP, Mannion DW, Lyons BJ (2009) Health-related quality of life after prolonged pediatric intensive care unit stay. Pediatr Crit Care Med 10:41–44
Typpo KV, Petersen NJ, Hallman M, Markovitz BP, Mariscalco MM (2009) Day 1 multiple organ dysfunction syndrome is associated with poor functional outcome and mortality in the pediatric intensive care unit. Pediatr Crit Care Med 10:562–570
Visser IH, Hazelzet JA, Albers MJ, Verlaat CW et al (2013) Mortality prediction models for pediatric intensive care: comparison of overall and subgroup specific performance. Intensive Care Med 39:942–950
Namachivayam P, Shann F, Shekerdemian L, Taylor A et al (2010) Three decades of pediatric intensive care: who was admitted, what happened in intensive care, and what happened afterward. Pediatr Crit Care Med 11(5):549–555
Epstein D, Wong CF, Khemani RG, Moromisato DY et al (2011) Race/ethnicity is not associated with mortality in the PICU. Pediatrics 127:e588–e597
Pollack MM, Holubkov R, Funai T, Clark A et al (2014) Pediatric intensive care outcomes: development of new morbidities during pediatric critical care. Pediatr Crit Care Med 15:821–827
Janssens L, Gorter JW, Ketelaar M, Kramer WLM, Holtslag HR (2008) Health-related quality-of-life measures for long-term follow-up in children after major trauma. Qual Life Res 17:701–713
Janssens L, Gorter JW, Ketelaar M, Kramer WLM, Holtslag HR (2009) Long-term health condition in major pediatric trauma: a pilot study. J Ped Surg 44:1591–1600
Solans M, Pane S, Estrada MD, Serra-Sutton V et al (2007) Health-related quality of life measurement in children and adolescents: a systematic review of generic and disease specific instruments. Value Health 11(4):742–764
Martin-Herz SP, Zatzick DF, McMahon RJ (2012) Health-related quality of life in children and adolescents following traumatic injury: a review. Clin Child Fam Psychol Rev 15(3):192–214
World Health Organization (1958) The first ten years of the World Health Organization. World Health Organization, Geneva
Knoester H, Grootenhuis MA, Bos AP (2007) Outcome of pediatric intensive care survivors. Eur J Pediatr 166:1119–1128
Knoester H, Bronner MB, Bos AP, Grootenhuis MA (2008) Quality of life in children three and nine months after discharge from a paediatric intensive care unit: a prospective cohort study. Health Qual Life Outcomes 6:1–9
Eiser C, Morse R (2001) Quality-of-life measures in chronic diseases of childhood. Health Technol Assess 5:1–157
[No authors listed] (1995) The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med 41:1403–1409
Simon AE, Chan KS, Forrest CB (2008) Assessment of children’s health-related quality of life in the United States with a multidimensional index. Pediatrics 121:e118–e126
Angus DC, Carlet J (2003) Surviving intensive care: a report from the 2002 Brussels roundtable. Intensive Care Med 29(3):368–377
Wilson IB, Cleary PD (1995) Linking clinical variables with health-related quality of life. JAMA 273:59–65
Morrison AL, Gillis J, O’Connell AJ, Schell DN, Dossetor DR, Mellis C (2002) Quality of life of survivors of pediatric intensive care. Pediatr Crit Care Med 3(1):1–5
Colville G, Kerry S, Pierce C (2008) Children’s factual and delusional memories of intensive care. Am J Respir Crit Care Med 177:976–982
Colville GA, Pierce CM (2013) Children’s self-reported quality of life after intensive care treatment. Pediatr Crit Care Med 14:e85–e92
Samransamruajit R, Boonsag K, Chanprasert K, Deelodejanawong J et al (2011) Clinical functional outcomes and quality of life in children surviving from ARDS. Pediatr Crit Care 12[3 Suppl]:163
Brook A, Schulz S, Yung M (2011) Paediatric intensive care follow-up study (pilot). Pediatr Crit Care Med 12[3 Suppl]:1099
Pollack MM, Wilkinson JD, Glass NL (1987) Long-stay pediatric intensive care unit patients: outcome and resource utilization. Pediatrics 80:855–860
Butt WW (2009) Outcome assessment—what outcome do we want? Pediatr Crit Care Med 10(1):133–134
Marcin JP, Slonim AD, Pollack MM, Ruttimann UE (2001) Long-stay patients in the pediatric intensive care unit. Crit Care Med 29:652–657
Namachivayam O, Taylor A, Montague T, Moran K et al (2012) Long-stay children in intensive care: long-term functional outcome and quality of life from a 20-yr institutional study. Pediatr Crit Care Med 13:520–528
Buysse CM, Raat H, Hazelzet JA, Hop WC, Maliepaard M, Joosten KF (2008) Surviving meningococcal septic shock: health consequences and quality of life in children and their parents up to 2 years after pediatric intensive care unit discharge. Crit Care Med 36(2):596–602
Buysse C, Vermunt L, Raat H, Hazelzet JA (2010) Surviving meningococcal septic shock in childhood: long-term overall outcome and the effect on health-related quality of life. Crit Care 14(3):R124
Edmond K, Dieye Y, Griffiths UK, Fleming J, Ba O, Diallo N, Mulholland K (2010) Prospective cohort study of disabling sequelae and quality of life in children with bacterial meningitis in urban Senegal. Pediatr Infect Dis J 29(11):1023–1029
Als LC, Nadel S, Cooper M, Pierce CM, Sahakian BJ et al (2013) Neuropsychologic function three to six months following admission to the PICU with meningoencephalitis, sepsis, and other disorders: a prospective stucy of school-aged children. Crit Care Med 41:1094–1103
Farris RW, Weiss NS, Zimmerman JJ (2013) Functional outcomes in pediatric severe sepsis: further analysis of the researching severe sepsis and organ dysfunction in children: a global perspective trial. Pediatr Crit Care Med 14:835–842
Matos RI, Watson RS, Nadkarni VM, Huang HH et al(2013) Duration of cardiopulmonary resuscitation and illness category impact survival and neurologic outcomes for in-hospital pediatric cardiac arrests. Circulation 127:442–451
Ebrahim S, Singh S, Hutchinson JS, Kulkarni AV et al (2013) Adaptive behavior, functional outcomes, and quality of life outcomes of children requiring urgent ICU admission. Pediatr Crit Care Med 14:10–18
Polic B, Mestrovic J, Markic J, Mestrovic M et al (2013) Long-term quality of life of patients treated in paediatric intensive care unit. Eur J Pediatr 172:85–90
Cunha F, Mota T, Texeira-Pinto A, Carvalho L et al (2013) Factors associated with health-related quality of life changes in survivors to pediatric intensive care. Pediatr Crit Care Med 14:e8–e15
Bloom B, Dey AN, Freeman G (2006) Summary health statistics for US children: national health interview survey, 2005. Vital Health Stat 10:1–84
Centers for Disease Control and Prevention (2007) WISQARS (Web-based Injury Statistics Query and Reporting System). Centers for Disease Control and Prevention, Atlanta
Holbrook TL, Hoyt DB, Coimbra R, Potenza B et al (2007) Trauma in adolescents causes long-term market deficits in quality of life: adolescent children do not recover preinjury quality of life or function up to two years postinjury compared to national norms. J Trauma Inj Infect Crit Care 62:577–583
Sorensen TI, Nielsen GG, Andersen PK, Teasdale TW (1988) Genetic and environmental influences on premature death in adult adoptees. N Engl J Med 318(12):727–732
Varni JW, Sherman SA, Burwinkle TM, Dickinson PE, Dixon P (2004) The PedsQL family impact module: preliminary reliability and validity. Health Qual Life Outcomes 2:55
Feudtner C, Christakis DA, Connell FA (2000) Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington State, 1980–1997. Pediatrics 106(1 Pt 2):205–209
Mestrovic J, Kardum G, Sustic A, Polic B et al (2007) Neurodevelopmental disabilities and quality of life after intensive care treatment. J Paediatr Child Health 43:673–676
Jones S, Rantell K, Stevens K, Colwell B et al (2006) Outcome at 6 months after admission for pediatric intensive care: a report of a national study of pediatric intensive care units in the United Kingdom. Pediatrics 118:2101
Simon AE, Chan KS, Forrest CB (2008) Assessment of children’s health-related quality of life in the United States with a multidimensional index. Pediatrics 121(1):e118–e126
Dosa NP, Boeing NM, Ms N, Kanter RK (2001) Excess risk of severe acute illness in children with chronic health conditions. Pediatrics 107(3):499–504
Odetola FO, Gebremariam A, Davis MM (2010) Comorbid illnesses among critically ill hospitalized children: impact on hospital resource use and mortality, 1997–2006. Pediatr Crit Care Med 11(4):457–463
Burns KH, Casey PH, Lyle RE, Bird TM, Fussell JJ, Robbins JM (2010) Increasing prevalence of medically complex children in US hospitals. Pediatrics 126(4):638–646
Boyle CA, Boulet S, Schieve LA, Cohen RA, Blumberg SJ, Yeargin-Allsopp M, Visser S, Kogan MD (2011) Trends in the prevalence of developmental disabilities in US children, 1997–2008. Pediatrics 127(6):1034–1042
Edwards JD, Houtrow AJ, Vasilevskis EE, Rehm RS, Markovitz BP, Graham RJ, Dudley RA (2012) Chronic conditions among children admitted to U.S. pediatric intensive care units: their prevalence and impact on risk for mortality and prolonged length of stay*. Crit Care Med 40(7):2196–2203
Cunha F, Almeida-Santos L, Teixeira-Pinto A, Neves F et al (2012) Health-related quality of life of pediatric intensive care survivors. J Pediatr 88(1):25–32
Typpo KV, Petersen NJ, Petersen LA, Mariscalco MM (2010) Children with chronic illness return to their baseline functional status after organ dysfunction on the first day of admission in the pediatric intensve care unit. J Pediatr 157:108–113
Sturms LM, van der Sluis CK, Groothoff JW, Eisma WH, den Duis HJ (2002) The health-related quality of life of pediatric traffic victims. J Trauma Inj Infect Crit Care 52:88–94
Smith GD, Hart C, Blane D, Gillis C, Hawthorne V (1997) Lifetime socioeconomic position and mortality: prospective observational study. BMJ 314(7080):547–552
Adler NE, Boyce WT, Chesney MA, Folkman S, Syme SL (1993) Socioeconomic inequalities in health. No easy solution. JAMA 269(24):3140–3145
Ho KM, Dobb GJ, Knuiman M, Finn J, Webb SA (2008) The effect of socioeconomic status on outcomes for seriously ill patients: a linked data cohort study. Med J Aust 189(1):26–30
Sarsour K, Sheridan M, Jutte D, Nuru-Jeter A et al (2011) Family socioeconomic status and child executive functions: the roles of language, home environment, and single parenthood. J Int Neuropsychol Soc 17:120–132
Barlow JH, Ellard DR (2006) The psychosocial well-being of children with chronic disease, their parents and siblings: an overview of the research evidence base. Child Care Health Dev 32(1):19–31
Drotar D (1997) Relating parent and family functioning to the psychological adjustment of children with chronic health conditions: what have we learned? What do we need to know? J Pediatr Psychol 22(2):149–165
Klassen A, Raina P, Reineking S, Dix D, Pritchard S, O’Donnell M (2007) Developing a literature base to understand the caregiving experience of parents of children with cancer: a systematic review of factors related to parental health and well-being. Support Care Cancer 15(7):807–818
Daniels D, Moos RH, Billings AG, Miller JJ 3rd (1987) Psychosocial risk and resistance factors among children with chronic illness, healthy siblings, and healthy controls. J Abnorm Child Psychol 15(2):295–308
Jessop DJ, Riessman CK, Stein RE (1988) Chronic childhood illness and maternal mental health. J Dev Behav Pediatr 9(3):147–156
Pochard F, Azoulay E, Chevret S, Lemaire F, Hubert P, Canoui P et al (2001) Symptoms of anxiety and depression in family members of intensive care unit patients: ethical hypothesis regarding decision-making capacity. Crit Care Med 29(10):1893–1897
Rees G, Gledhill J, Garralda ME, Nadel S (2004) Psychiatric outcome following paediatric intensive care unit (PICU) admission: a cohort study. Intensive Care Med 30:1607–1614
Rennick JE, Johnson CC, Dougherty G, Platt R, Ritchie JA (2002) Children’s psychological responses after critical illness and exposure to invasive technology. J Dev Behav Pediatr 23:133–144
Holbrook TL, Hoyt DB, Coimbra R, Potenza B, Size M, Anderson JP (2005) Long-term posttraumatic stress disorder persists after major trauma in adolescents: new data on risk factors and functional outcome. J Trauma Inj Infect Crit Care 58:764–769
Vollrath M, Landolt MA (2005) Personality predicts quality of life in pediatric patients with unintentional injuries: a 1-year follow-up study. J Pediatr Psychol 30:481–491
Landolt MA, Vollrath ME, Gnehm HE, Sennhauser FH (2009) Post-traumatic stress impacts on quality f life in children after road traffic accidents: prospective study. Aust N Z J Psychol 43:746–753
Zatzick DF, Jurkovich GJ, Fan MY, Grossman D et al (2008) Association between posttraumatic stress and depressive symptoms and functional outcomes in adolescents followed up longitudinally after injury hospitalization. Arch Pediatr Adolesc Med 162:642–648
Colville G, Pierce C (2012) Patterns of post-traumatic stress symptoms in families after paediatric intensive care. Intensive Care Med 38:1523–1531
Dow B, Kenardy J, Long D, Le Brocque R (2011) Beyond survival recall and aspects of care and environement in children’s psychological distress following picu admission. Pediatr Crit Care Med 12(3 suppl):680
Guerra GG, Robertson CMT, Alton GY, Joffe AR, Moez EK, Dinu IA, Ross DB, Rebeyka IM, Lequier L, Western Canadian Complex Pediatric Therapies Follow-Up Group (2014) Health-related quality of life in pediatric cardiac extracorporeal life support survivors. Pediatr Crit Care Med 15:720–727
Fiser DH, Long N, Roberson PK, Hefley G, Zolten K, Brodie-Fowler M (2000) Relationship of pediatric overall performance category and pediatric cerebral performance category scores at pediatric intensive care unit discharge with outcome measures collected at hospital discharge and 1- and 6-month follow-up assessments. Crit Care Med 28(7):2616–2620
World Health Organization (1948) Constitution of the World Health Organization basic document. World Health Organization, Geneva
Varni JW, Seid M, Kurtin PS (2001) PedsQL 4.0 reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 39(8):800–812
Varni JW, Burwinkle TM, Seid M, Skarr D (2003) The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr 3(6):329–341
Elliot D, Davidson JE, Harvey MA, Bernis-Dougherty A, Hopkins RO, Iwashyna TJ, Wagner J, Weinert C, Wunsch J et al (2014) Exploring the scope of post-intensive care syndrome therapy and care:engagement of non-critical care providers and survivors in a second stakeholders meeting. Crit Care Med 42(12):2518–2526
Jardine J, Glinianaia SV, McConachie H, Embleton ND, Rankin J (2014) Self-reported quality of life of young children with conditions from early infancy: a systematic review. Pediatrics 134:e1129–e1148
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aspesberro, F., Mangione-Smith, R. & Zimmerman, J.J. Health-related quality of life following pediatric critical illness. Intensive Care Med 41, 1235–1246 (2015). https://doi.org/10.1007/s00134-015-3780-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-3780-7