Abstract
Purpose
To evaluate the effects of an oral health protocol on the incidence of postoperative pneumonia in patients submitted to coronary artery bypass grafting and to valve surgery.
Methods
All patients admitted to a public cardiac surgery hospital were examined by a dentist and had a thorough dentistry anamnesis and an intraoral exam focusing on teeth, gums, and tongue. Patients were taught how to brush their teeth and tongue and how to clean their jugal and palatal membranes. Chlorhexidine gluconate (CXG) 0.12 % oral rinse twice a day was used until surgery. Data on age, sex, comorbidities, oral evaluation, type of surgery, and development of pneumonia were obtained. Statistical analysis was done on these variables to evaluate the impact of the study protocol.
Results
A total of 226 patients were enrolled, 136 male (60.2 %). The median age was 59 years. There were 123 (54.4 %) patients with coronary artery disease and 103 (45.6 %) with valve disease. There were 18/226 (8 %) postoperative pneumonias (PP), nine in each group. Ten occurred in dentate patients and eight in edentulous ones. Oral health optimization was achieved in 208/226 (92 %) of patients in the preoperative period. The presence of tongue plaque (OR 17, P < 0.001) and of poor hygiene of the total superior dentures (OR 25, P < 0.001) in the preoperative period significantly increased the chance of PP. The use of CXG 0.12 % in the preoperative period (OR 0.06, P < 0.001) and on the day of surgery (OR 0.002, P < 0.001) was protective against PP. Mortality in patients without pneumonia was 9/208 (4.32 %) vs. 6/19 (33.3 %) in those with pneumonia. The presence of pneumonia increased the chances of death by 11 times (P < 0.001). The mean pneumonia rate in ICU in the 6 months before the study protocol was 32 per 1,000 ventilator-days, 24 during the 6-month intervention period, and 10 during the next 6 months following the study.
Conclusions
PP rates were reduced using a simple and efficient protocol of dental care that improved oral hygiene in the preoperative period of cardiac surgery patients.
Similar content being viewed by others
Introduction
Pneumonia is an infection of the lungs, and bacterial pneumonia is a common and significant cause of mortality and morbidity in human populations [1].
Ventilator-associated pneumonia (VAP) is defined as a nosocomial pneumonia that develops in patients on mechanical ventilation for 48 h or more, and patients with VAP have high hospital mortality [2]. VAP has high morbidity and mortality in the ICU; mortality ranges from 24 to 50 %. Two types of VAP are distinguished: early-onset VAP, diagnosed within the first 96 h of mechanical ventilation, and late-onset, occurring thereafter. The mechanical process of intubation compromises the natural barrier between the oropharynx and trachea and facilitates the entry of bacteria into the lungs around the endotracheal tube cuff [3]. It is difficult to completely prevent secretions of the oropharynx from invading the airway through the space around the cuff of the tracheal tube, and the pooling of secretions around the cuff may provide a reservoir for pathogenic bacteria [3].
VAP was confirmed as the main cause of postoperative infection in patients undergoing major heart surgery [4].
Nosocomial pathogens may be part of the host’s endogenous flora, or may be acquired from other patients, staff, devices, or the hospital environment [5]. The oral cavity may be an important reservoir of bacteria responsible for causing lung infection [1]. Oropharynx colonization is important for the development of respiratory infection, because oral microorganisms of critically ill adults differ from those of healthy adults [6].
The surface of the tongue facilitates the accumulation of nutrient-rich dietary debris. The biofilm on the tongue’s surface is packed less densely than in periodontal plaque, so this probably facilitates nutrient delivery into saliva. The killing of bacteria in the biofilm requires antibiotic/disinfectant concentrations 10–1,000 times those needed to kill free-living forms, and the most effective way to treat biofilm is by mechanical debridement or removal [7]. Edentulous elderly patients with the presence of tongue coating have demonstrated significantly higher salivary bacterial counts than those with no tongue coating [8].
People with teeth or dentures have nonshedding surfaces on which biofilms form, and these biofilms are susceptible to colonization by respiratory pathogens [9]. A systematic review of the literature studying the association between poor oral hygiene and the risk of nosocomial pneumonia and chronic lung disease found that improving oral hygiene can significantly reduce the incidence of pulmonary disease [10]. According to current evidence, it appears that toothbrushing has beneficial effects in reducing dental plaque colonization [11] and chlorhexidine may effectively reduce oropharyngeal colonization and VAP [12].
Chlorhexidine gluconate (CXG) mouthwash is an antiplaque agent that is effective at low concentrations with little, if any, absorption from the gastrointestinal tract and the oral mucous membrane [13]. At the present time there is no evidence to support the use of one oral rinse over another in mouth care, the exception being the use of CXG 0.12 % in cardiac surgery patients [11].
The mean rate of postoperative pneumonia (PP) in cardiac surgery patients in the Instituto Nacional de Cardiologia (INC) was 32 per 1,000 ventilator-days in the 6 months before the intervention, well above that reported in the literature (around 14 per 1,000) [14]. A protocol was implemented including oral hygiene instructions, toothbrushing, tongue and denture hygiene in association with the use of CXG 0.12 % oral rinse. The goal was to reduce PP rates, particularly in the coronary artery bypass grafting (CABG) group, because no routine dental care was offered to them at INC, a procedure that differs from that adopted for patients with valvular heart disease.
Methods
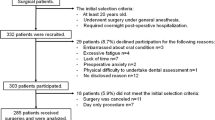
Patients were recruited during a 6-month period after their admission to INC, a federal public hospital located in Rio de Janeiro, Brazil. Patients were invited by the principal investigator to participate in the study by signing the informed consent form (ICF). Forty-two patients were excluded, and 226 were included. The study was approved by the institutional review board of this hospital under number 0307/26.01.2011.
Inclusion criteria were being 18 years of age or older; a candidate for heart valve surgery (valve repair or replacement); a candidate for CABG; and signing the ICF. The exclusion criterion was a history of pneumonia less than 2 weeks prior to admission.
Patients were examined in the dentistry unit by the same dentist (EHB). Examination consisted of a medical and dentistry anamnesis, and an intraoral exam of the oral and palatal mucosal tissue, tongue, and teeth. During examination, some indices were obtained:
-
(a)
Decayed, missing, and filled teeth index (DMFT), which determines the total number of permanent teeth that have past or present carious lesions [15].
-
(b)
Simplified oral hygiene index (OHI-S) by (Greene and Vermillion 1964). This quantifies the plaque and calculus index and allows classification of oral hygiene [16]. Oral hygiene was classified after the oral hygiene index and was calculated by the totality of debris index + calculus index by the following scores: 0–1, satisfactory; >1.1, unsatisfactory [17].
-
(c)
Community periodontal index of treatment needs (CPITN), which was used to determine the periodontal needs, and to quantify periodontal disease: (0) healthy periodontal tissues; (1) bleeding after gentle probing; (2) supragingival or subgingival calculus or defective margin of filling or crown; (3) 4 or 5 mm pocket; (4) 6 mm or deeper pathologic pocket [18]. Patients were considered as having periodontal disease if they received the score number 4.
-
(d)
The additive index, which quantifies the plaque of total maxillary dentures, with a score between 0 and 15 points was recorded in five defined areas on the denture base: 0, no visible plaque; 1, plaque visible only by scraping on the denture base; 2, moderate accumulation; 3, abundant plaque [19]. All dentures with a score greater than 10 were considered to be in a state of poor hygiene.
Totally edentulous patients were assessed in terms of the hygiene of the total maxillary dentures and of the tongue.
The presence of active infectious foci such as teeth or residual roots with active carious lesions, residual roots with endodontic material exposed in the intraoral environment, inflamed gums with suppuration, teeth mobility with subgingival calculus and oral candidiasis was evaluated in all patients.
Patients were instructed on how to brush their teeth by using the Bass technique [20], cleaning the palate, the tongue, and the denture by brushing. They were instructed to use CXG 0.12 % twice a day, after breakfast and before sleep, by rinsing the mouth with 15 ml for 2 min including gargling. They were also instructed to do the same process with CXG 0.12 % just before going to the operating room. In the immediate postoperative period (in ICU) nursing staff and/or the responsible dentist (EHB) performed the oral hygiene protocol twice a day using toothbrushing and CXG 0.12 % even in intubated patients. Patients were also instructed to continue the same preoperative protocol as soon as they returned to the ward. Patients continued to be assessed in the postoperative period to observe the effectiveness of oral care and were considered to have optimized oral hygiene if they presented with less intraoral plaque and/or if they were using CXG 0.12 % as recommended. Postoperative pneumonia was diagnosed by the Clinical Pulmonary Infection Score (CPIS) modified by Flanagan et al. [21]. Clinical suspicion of VAP was diagnosed from chest X-rays showing a new, persistent (>24 h), and/or progressive infiltrate, abscess, cavitation, or suspected empyema, and an increase in the volume and purulence of suctioned secretions, and one or more of the following: fever of at least 38 °C for more than 4 h; blood leukocytosis of least 11 × 109/l; and an increase in the fraction of inspired oxygen (FIO2) of 0.2 needed to maintain arterial oxygen saturation, sustained for more than 4 h. A CPIS of at least 6 was very suggestive of pneumonia [21]. The VAP bundle included elevation of the head of the bed (HOB) (30–45°); daily “sedation vacations” and assessment of the readiness to extubate; peptic ulcer disease prophylaxis (all patients were administered antacids, ranitidine or omeprazole, as a postoperative protocol for gastric bleeding prevention in cardiac surgery); and deep venous thrombosis/pulmonary thromboembolism (DVT/PE) prophylaxis for all ICU patients requiring mechanical ventilation. Pneumonia rates were expressed by the number of pneumonias per 1,000 days of mechanical ventilation, as per the Centers for Disease Control and Prevention National Healthcare Safety Network (CDC/NHSN) definition [22]. All procedures were registered and collected in a specific record sheet. A control group was considered unethical by the ethics committee.
Statistical analysis
Percentages were calculated for discrete variables, and median and interquartile ranges for continuous variables. The association between categorical variables was made by contingency tables analyzing Pearson chi-squared test or Fisher’s exact test. All continuous variables did not show Gaussian distribution in the Shapiro–Wilk test and therefore a non-parametric test was used. The Mann–Whitney non-parametric test was used to verify differences between continuous variables by surgery groups and pneumonia. P values were considered statistically significant if less than 0.05; any P value less than 0.001 was recorded as P < 0.001. Data were collected and analyzed in the Epi Info statistical program, version 3.3.2 and Statistical Package for Social Sciences version 16.0.
Results
A total of 226 patients were included, of which 136 were male (60.2 %). The median age was 59 years. There were 50.9 % white, 21.7 % black, and 27.4 % mulatto. The median body mass index was 26.8. There were 123 (54.4 %) patients with coronary artery disease and 103 (45.6 %) with valvular disease. The number of patients submitted to combined surgery (CABG and VS) was 22 (9.7 %), and they were reclassified into VS or CABG groups according to the main underlying condition. So 16 (7.1 %) were enrolled in the VS group and 6 (2.6 %) in the CABG group. Forty-two patients were excluded because their cardiologist recommended clinical treatment and discharged them.
Patients from the VS group had received 2 g of amoxicillin 1 h before the invasive dentistry treatment as endocarditis prophylaxis. Two patients from the VS group were treated for endocarditis with vancomycin, and four patients from the CABG group were treated with clindamycin for an odontogenic infection before surgery. All patients received 2 g of cefazolin 30 min before cardiac surgery as wound infection prophylaxis except those treated for endocarditis, who received extended prophylaxis with vancomycin and ciprofloxacin for 24 h.
The two surgical groups were compared before cardiac surgery. Comorbidities, sociodemographic characteristics, and oral hygiene status are shown in Table 1 and continuous variables are shown in Table 2.
The oral health classification in the VS group in the first dentistry evaluation was satisfactory in 49.5 %, unsatisfactory in 27.5, and 23.0 % of patients were totally edentulous.
The oral health classification in the CABG group in the first dentistry evaluation was satisfactory in 27.6 %, unsatisfactory in 35.8, and 36.6 % were totally edentulous.
The first dentistry evaluation showed that the two surgery groups were different, with the VS group having 2.3 times more chance of having satisfactory hygiene, P = 0.01.
Oral health optimization was achieved in 208/226 (92 %) of patients in the preoperative period, 93.5 % in the CABG group and 90.5 % in the VS group. A total of 60.2 % patients from the CABG group were classified as having satisfactory oral hygiene just before surgery compared to 27.6 % in the first evaluation, whereas 70.9 % of patients from the VS group had satisfactory oral hygiene just before surgery compared to 49.5 % in the first evaluation.
After oral health optimization, on evaluation just before surgery, the two surgery groups were no longer statistically different, P = 0.74.
The oral health classification just before surgery of all 18 patients who had PP was satisfactory in 1 (5.6 %), unsatisfactory in 9 (50.0 %), and 8 patients (44.4 %) were edentulous.
There were 18/226 (8 %) postoperative pneumonias, nine in each group. Ten occurred in dentate patients and 8 in edentulous ones. There were 7 (38.9 %) women and 11 (61.1 %) men. The median time of ICU stay was greater in patients who developed pneumonia (17.5 days) than those that did not (5.0 days), P < 0.001.
Comorbidities, sociodemographic characteristics, and oral hygiene status in patients with and without PP are shown in Table 3 and continuous variables are shown in Table 4. Although male sex, diabetes, and tobacco use were more prevalent in the CABG group, only hypertension was shown to increase the chance of pneumonia, and hypertension may be a confounding variable. Patients with unsatisfactory oral hygiene had 12 times the chance of developing PP compared with the ones with satisfactory oral hygiene (P = 0.004).
The presence of tongue plaque (OR 17, P < 0.001) and of poor hygiene of the total superior dentures (OR 25, P < 0.001) in the preoperative period significantly increased the chance of PP.
The use of CXG 0.12 % in the preoperative period (OR 0.06 P < 0.001) and on the day of surgery (OR 0.002 P < 0.001) was protective against PP.
In the preoperative period, 107 (87 %) patients in the CABG group and 94 (91.3 %) in the VS group used CXG 0.12 %. On the day of surgery, 109 (88.6 %) patients in the CABG group and 92 (89.3 %) in the VS group used CXG 0.12 %.
The presence of pneumonia increased the chances of death by 11 times, P < 0.001. Mortality in patients without pneumonia was 9/208 (4.32 %) vs. 6/19 (33.3 %) in those with pneumonia.
The mean VAP rate in the 6 months previous to the study protocol was 32 per 1,000 ventilator-days and it was 24 per 1,000 ventilator-days during the 6-month intervention period. During the next 6 months following the study, with continuity of implemented measures by ICU staff, the rate was 10 per 1,000 ventilator-days.
Microbiological features of the 18 patients who developed PP are shown in Table 5.
A subgroup analysis was done for the patients who were ventilated for more than 2 days, comparing the 15 patients who had pneumonia to the 17 that did not have pneumonia. Oral hygiene optimization occurred more often in the no-pneumonia group (OR 64, P < 0.001), as well as the use of chlorhexidine preoperatively (OR 104, P < 0.001) and on the day of surgery (OR 136, P < 0.001). Poor denture hygiene was more frequent in those with pneumonia (OR 31.5, by Fisher’s, P = 0.005). There were no differences between the two subgroups in age, gender, or mortality.
Discussion
In this study, the characteristics of oral hygiene and postoperative pneumonias were compared between two cardiac surgery groups, VS and CABG. Patients with valve disease, historically, in our institute, showed lower rates of PP probably owing to better oral hygiene. Patients in this group have increased risk of endocarditis [23] and are frequently referred by physicians for dental care. After the protocol was implemented for all patients, there was a reduction in the overall rate of PP, and no difference was seen between the VS and CABG groups, meaning that the protocol worked well for both groups.
A large amount of dental plaque brings a high risk for development of VAP [24] and therefore risk reduction for PP was the goal of this oral intervention study [25].
Biofilm adheres and colonizes mucosal surfaces, teeth, dorsum of the tongue, and foreign bodies including dentures and the endotracheal tube [12]. In edentulous people, dentures may easily serve as a reservoir for bacteria if they are not properly cleaned. The surgery groups were not different in the preoperative period for debris on the tongue, debris on the denture, calculus on the denture, and total superior denture with poor hygiene; however, the groups were different concerning periodontal disease. Scannapieco and Genco [10] showed the potential correlation of periodontal disease with VAP, but in our study the correlation of periodontal disease with PP was not significant, possibly because 14 of the 18 patients diagnosed in the preoperative period with periodontal disease had their oral hygiene improved by the protocol measures. The CABG group showed a higher percentage of active oral infection, compared with the VS group, but the number of patients who went to surgery with active oral infection was small, as they were treated before surgery.
In two studies, the authors excluded edentulous patients [26, 27]. In our study, this could not be done as there were a large number of edentulous people (30.5 %), and pneumonia was significantly linked with the presence of tongue plaque and poor hygiene of the total superior denture (variables not linked with teeth). Before this study, edentulous patients were not sent for dental evaluation in INC prior to cardiac surgery. This practice has changed, and all patients, dentate or not, are now examined in the preoperative period.
Although oral rinse with CXG is generally accepted as an effective measure to reduce the risk of VAP, including in cardiac surgery patients [28], it remains unclear which concentration to use, what the exposure time should be, and how frequently it should be performed [14]. A study in a surgical/trauma/burn ICU, using toothbrushing for 1–2 min twice a day with 15 ml of CXG 0.12 % solution achieved a 46 % reduction in VAP rates [29]. Using the same protocol in the preoperative period, we achieved a 25 % reduction in 6 months and 69 % in 12 months, showing that this protocol was effective in the setting of patients submitted to cardiac surgery in a developing country.
Recent surveillance data in which 173 ICUs from different continents were involved, the estimated pooled mean of VAP was 13.6 per 1,000 ventilator-days [14]. In our study, similarly to that by Garcia et al. [30], VAP rates decreased during and after the intervention period. We observed in the study that 92 % of patients improved oral hygiene, and systematic oral care can improve oral health in critically ill patients [31].
Oral care with the use of CXG is part of the European care bundle for prevention of VAP [32], and oral care was recognized by the CDC as a modifiable risk factor for preventing VAP [33]. We have included oral hygiene in the pneumonia bundle at our hospital following the results of this intervention.
It seems that oral disinfection with CXG [34] and mechanical oral hygiene with toothbrushing are required for optimal oral health [35]. A systematic review on toothbrushing in VAP found a significant reduction in rates in the trial at low risk of bias, and when all trials were considered, there was a trend toward lower VAP rates [35]. In accordance with a meta-analysis and the American Association of Critical Care Nursing, CXG and mechanical oral care need further studies so that their effects can be clearly explained and elucidated [36, 37]. Although the importance of toothbrushing in reducing VAP rates is recognized [35], the role of brushing oral surfaces needs further evaluation. We need more research on this aspect of oral care to evaluate its potential, because until now no effect on reducing VAP, mortality, or length of stay has been proved, especially in cardiac surgery patients. We believe CXG alone can make intraoral plaque less pathogenic, but removing the intraoral plaque can reduce bacterial lung translocation. It was not the purpose of this study to compare CXG alone and CXG associated with toothbrushing, because the goal was to offer optimal health care for all patients with a combined mechanical and chemical approach.
As shown in other studies, PP is related to longer ventilator times following surgery and higher mortality rates. Other variables, such as depth of sedation, may account for this, and although daily awakening from sedation is part of the VAP protocol implemented in our ICU, it was not systematically studied in this report [38]. Patients ventilated for more than 2 days in this study still experienced a protective effect with the use of chlorhexidine preoperatively and with oral health optimization, and pneumonia was associated with poor denture hygiene. Therefore, despite the possibility of cardiac, respiratory, and neurological failure in those with more than 2 days of ventilation, the protocol protected even these more vulnerable patients from pneumonia.
During the study period, endotracheal tubes with subglottic drainage were not used; therefore, this confounding variable was absent [14]. This form of prevention is valid and has been shown in another Brazilian hospital [34]; however, avoiding secretions that reach the area around the cuff is the critical issue, and we have focused on oral hygiene and CXG 0.12 % use. Since microaspiration of secretions is an etiological factor for VAP, oral suctioning and practices for management of the cuffs of endotracheal tubes (pressure over 20 cmH2O) are very important [39]. The costs of endotracheal tubes with a subglottic device may be too high for routine use in our scenario and need to be further evaluated [40].
Limitations
Firstly, although CXG 0.12 % showed very good results, the study was not controlled for that. Secondly, this is a single center study in the setting of a developing country and results may not be amenable to extrapolation.
Conclusions
PP rates were reduced during the study period and the incidence of PP in CABG and VS groups decreased, showing the importance of improving oral hygiene in the preoperative and postoperative period of patients submitted to cardiac surgery.
References
Paju S, Scannapieco FA (2007) Oral biofilms, periodontitis, and pulmonary infections. Oral Dis 13:508–512
Hutchins K, Karrus G, Erwin J et al (2009) Ventilator-associated pneumonia and oral care: a successful quality improvement project. Am J Infect Control 37(7):590–597
American Thoracic Society, Infectious Diseases Society of America (2005) Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 171:388–416. doi: 10.1164/rccm.200405-644ST
Hortal J, Muñoz p, Cuerpo G et al (2009) Ventilator-associated pneumonia in patients undergoing major heart surgery: an incidence study in Europe. Crit Care 13(3):R80
Craven DE (2000) Epidemiology of ventilator-associated pneumonia. Chest 117:1865–1875
Garcia R (2005) A review of the possible role of oral and dental colonization on the occurrence of health care-associated pneumonia: underappreciated risk and a call for interventions. Am J Infect Control 33:527–541
Drinka PJ, El-Solh AA (2010) The tongue, oral hygiene, and prevention of pneumonia in the institutionalized elderly. JAMDA 11(7):465–467
Abe S, Ishihara K, Adachi M et al (2008) Tongue-coating as risk indicator for aspiration pneumonia in edentate elderly. Arch Gerontol Geriatr 47:267–275
Scannapieco FA (2006) Pneumonia in nonambulatory patients. JADA 137:215–219
Scannapieco FA, Genco RJ (1999) Association of periodontal infections with atherosclerotic and pulmonary diseases. J Periodontal Res 34:340–345
Berry AM, Davidson PM, Nicholson L et al (2011) Consensus based clinical guideline for oral hygiene in the critically ill. Intensive Crit Care Nurs 27:180–185
Halm MA, Armola R (2009) Effect of oral care on bacterial colonization and ventilator-associated pneumonia. Am J Crit Care 18:275–278
Dodd MJ, Dibble SL, Miaskowski C et al (2000) Randomized clinical trial of the effectiveness of 3 commonly used mouthwashes to treat chemotherapy-induced mucositis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 90(1):39–47
Blot S, Rello J, Vogelaers D (2011) What is new in the prevention of ventilator-associated pneumonia? Curr Opin Pulm Med 17:155–159
DMFT index. http://classof2011indexwikisite.wikispaces.com/DMFT+Index. Accessed May 2013
Greene JC, Vermillion JR (1964) Simplified oral hygiene index. http://www.mah.se/CAPP/Methods-and-Indices/Oral-Hygiene-Indices/Simplified-Oral-Hygiene-Index-OHI-S/. Accessed May 2013
Dos Santos PAT, Fortes TMV, Cabral MCB et al (2008) Influence of sexual hormones on periodontal tissues in hormonal contraceptives users. Revista de Periodontia 18(03):55–63
CPITN index. http://classof2011indexwikisite.wikispaces.com/CPITN+Index. Accessed May 2013
Ambjornsen E, Vulderhaug J, Norheim PW et al (1982) Assessment of an additive index for plaque accumulation on complete maxillary dentures. Acta Odontol Scand 40(4):203–208
Bass method. http://www.oralcareshop.com/bass-method.htm. Accessed May 2013
Flanagan PG, Findlay GP, Magee JT et al (2000) The diagnosis of ventilator-associated pneumonia using non-bronchoscopic, non-directed lung lavages. Intensive Care Med 26:20–30
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of healthcare-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332
Wilson W, Taubert KA, Gewitz M et al (2007) Prevention of infective endocarditis. Guidelines from the American Heart Association. A guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation 116:1736–1754
Munro CL, Grap MJ, Elswick RK Jr et al (2006) Oral health status and development of ventilator-associated pneumonia: a descriptive study. Am J Crit Care 15:453–460
Jones DJ, Munro CL, Grap MJ (2011) Natural history of dental plaque accumulation in mechanically ventilated adults: a descriptive correlational study. Intensive Crit Care Nurs 27(6):299–304
Munro CL, Grap MJ, jones DJ et al (2009) Chlorhexidine, toothbrushing, and preventing ventilator-associated pneumonia in critically ill adults. Am J Crit Care 18(5):428–438
Grap MJ, Munro CL, Hamilton VA et al (2011) Early, single chlorhexidine application reduces ventilator-associated pneumonia in trauma patients. Heart Lung 40(5):e115–e122
Chlebicki MP, Safdar N (2007) Topical chlorhexidine for prevention of ventilator-associated pneumonia: a meta-analysis. Crit Care Med 35:595–602
Sona CS, Zack JE, Schallom ME et al (2009) The impact of a simple, low-cost oral care protocol on ventilator-associated pneumonia rates in a surgical intensive care unit. J Intensive Car Med 37(7):590–597
Garcia R, Jendresky L, Colbert L et al (2009) Reducing ventilator-associated pneumonia through advanced oral-dental care: a 48-month study. Am J Crit Care 18(6):523–534
Fourrier F, Duvivier B, Boutigny H et al (1998) Colonization of dental plaque: a source of nosocomial infections in intensive care unit patients. Crit Care Med 26(2):301–308
Rello J, Lode h, Cornaglia G et al (2010) A European care bundle for prevention of ventilator-associated pneumonia. Intensive Care Med 36:773–780
Tablan OC, Anderson IJ, Besser R et al (2004) Guidelines for preventing health-care-associated pneumonia, 2003: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR Recomm Rep 53:1–36
Caserta RA et al (2012) A program for sustained improvement in preventing ventilator associated pneumonia in an intensive care setting. BMC Infect Dis 12:234
Alhazzani W et al (2013) Toothbrushing for critically ill mechanically ventilated patients: a systematic review and meta-analysis of randomized trials evaluating ventilator-associated pneumonia. Crit Care Med 41:646–655
Martin B (2010) Oral care for patients at risk for ventilator-associated pneumonia. http://www.aacn.org/wd/practice/content/oral-care-practice-alert.pcms?menu=practice. Accessed May 2013
Balamurugan E, Kanimozhi A, Kumeri G (2012) Effectiveness of chlorhexidine oral decontamination in reducing the incidence of ventilator associated pneumonia: a meta-analysis. BJMP 5(1):a512
Shehabi Y et al (2013) Sedation depth and long-term mortality in mechanically ventilated critically ill adults: a prospective longitudinal multicentre cohort study. Intensive Care Med 39:910–918
Sole ML, Byers JF, Ludy JE et al (2002) Suctioning techniques and airway management practices: pilot study and instrument evaluation. Am J Crit Care 11:363–368
Muscerede J et al (2011) Subglottic secretion drainage for the prevention of ventilator-associated pneumonia: a systematic review and meta-analysis. Crit Care Med 39(8):1985–1991
Acknowledgments
We would like to thank all medical personnel in the ICU and all colleagues from the Dentistry Department; and Dr. Armando de Oliveira Schubach, Dr. Raquel de Vasconcellos C. de Oliveira and Dr Claudia Maria Valete Rosalino from IPEC, Fiocruz, for reviewing the paper critically; and José Emanuel Félix, from the Infection Control Unit (INC), for logistics support.
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bergan, E.H., Tura, B.R. & Lamas, C.C. Impact of improvement in preoperative oral health on nosocomial pneumonia in a group of cardiac surgery patients: a single arm prospective intervention study. Intensive Care Med 40, 23–31 (2014). https://doi.org/10.1007/s00134-013-3049-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-3049-y