Abstract
Purpose
Splanchnic artery occlusion (SAO) shock is a severe form of circulatory shock produced by ischemia and reperfusion of the splanchnic organs. The occlusion and reperfusion of the splanchnic arteries causes activation and adhesion of polymorphonuclear neutrophils (PMNs), release of proinflammatory substances and the formation of both species of oxygen and nitrogen derivatives free radicals. Olprinone is a specific phosphodiesterase-III inhibitor that has many properties; one of which is anti-inflammatory actions at therapeutic concentrations clinically used for heart failure. In this study, we wanted to evaluate the pharmacological action of olprinone (a PDEIII inhibitor) on SAO shock in mice.
Methods
SAO shock was induced by clamping both the superior mesenteric artery and the celiac trunk, resulting in a total occlusion of these arteries for 30 min. After this period of occlusion, the clamps were removed. Olprinone was given at a dose of 0.2 mg/kg i.p. 15 min before reperfusion.
Results
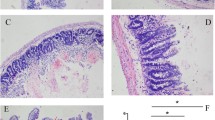
Our results indicated that olprinone up-regulated cAMP in injured ileum tissue, and decreased the ileum tissue damage after 1 h of reperfusion in SAO shock mice. Moreover, olprinone decreased NF-κB expression; the nitration of tyrosine residues; the phosphorylation of p38 MAPK and JNK; cytokine production (TNF-α and IL-1β); ICAM-1 and P-selectin expression and apoptosis in the injured ileum.
Conclusions
These results could imply a future use of olprinone in the therapy of ischemia and reperfusion shock.






Similar content being viewed by others
References
Mizushige K, Ueda T, Yukiiri K, Suzuki H (2002) Olprinone: a phosphodiesterase III inhibitor with positive inotropic and vasodilator effects. Cardiovasc Drug Rev 20:163–174
Sanada S, Kitakaze M, Papst PJ, Asanuma H, Node K, Takashima S, Asakura M, Ogita H, Liao Y, Sakata Y, Ogai A, Fukushima T, Yamada J, Shinozaki Y, Kuzuya T, Mori H, Terada N, Hori M (2001) Cardioprotective effect afforded by transient exposure to phosphodiesterase III inhibitors: the role of protein kinase A and p38 mitogen-activated protein kinase. Circulation 104:705–710
Ueda T, Mizushige K, Yukiiri K, Nishiyama Y, Kohno M (2004) The cerebrovascular dilatation effects of olprinone, a phosphodiesterase III inhibitor, in comparison with acetazolamide––a pilot study. Clin Neurol Neurosurg 106:284–288
Tajimi M, Ozaki H, Sato K, Karaki H (1991) Effect of a novel inhibitor of cyclic AMP phosphodiesterase, E-1020, on cytosolic Ca++ level and contraction in vascular smooth muscle. Naunyn Schmiedebergs Arch of Pharmacol 344:602–610
Okuda K, Kudo H, Ohishi K, Kitano T, Imasaka H, Noguchi T (1997) Effects of olprinone on IL-6 and IL-10 production during and after cardiac surgery. Masui 46:1580–1584
Altura BM, Gebrewold A, Burton RW (1985) Reactive hyperemic responses of single arterioles are attenuated markedly after intestinal ischemia, endotoxemia and traumatic shock: possible role of endothelial cells. Microcirc Endothelium Lymphatics 2:3–14
Carey C, Siegfried MR, Ma XL, Weyrich AS, Lefer AM (1992) Antishock and endothelial protective actions of a NO donor in mesenteric ischemia and reperfusion. Circ Shock 38:209–216
Zingarelli B, Squadrito F, Ioculano M, Altavilla D, Bussolino F, Campo GM, Caputi AP (1992) Platelet activating factor interaction with tumor necrosis factor and myocardial depressant factor in splanchnic artery occlusion shock. Eur J Pharmacol 222:13–19
Lefer AM, Lefer DJ (1993) Pharmacology of the endothelium in ischemia-reperfusion and circulatory shock. Annu Rev Pharmacol Toxicol 33:71–90
McCord JM (1985) Oxygen-derived free radicals in postischemic tissue injury. N Engl J Med 312:159–163
Parks DA, Granger DN (1986) Contributions of ischemia and reperfusion to mucosal lesion formation. Am J Physiol 250:G749–G753
Masini E, Cuzzocrea S, Mazzon E, Muia C, Vannacci A, Fabrizi F, Bani D (2006) Protective effects of relaxin in ischemia/reperfusion-induced intestinal injury due to splanchnic artery occlusion. Br J Pharmacol 148:1124–1132
Husted TL, Lentsch AB (2006) The role of cytokines in pharmacological modulation of hepatic ischemia/reperfusion injury. Curr Pharm Des 12:2867–2873
Frangogiannis NG (2007) Chemokines in ischemia and reperfusion. Thromb Haemost 97:738–747
Martinez-Mier G, Toledo-Pereyra LH, Ward PA (2000) Adhesion molecules in liver ischemia and reperfusion. J Surg Res 94:185–194
Serracino-Inglott F, Habib NA, Mathie RT (2001) Hepatic ischemia-reperfusion injury. Am J Surg 181:160–166
Ayub K, Serracino-Inglott F, Williamson RC, Mathie RT (2001) Expression of inducible nitric oxide synthase contributes to the development of pancreatitis following pancreatic ischaemia and reperfusion. Br J surg 88:1189–1193
Mizutani A, Murakami K, Okajima K, Kira S, Mizutani S, Kudo K, Takatani J, Goto K, Hattori S, Noguchi T (2005) Olprinone reduces ischemia/reperfusion-induced acute renal injury in rats through enhancement of cAMP. Shock 24:281–287
Miyakawa H, Kira S, Okuda K, Takeshima N, Mori M, Noguchi T (2008) Olprinone decreases elevated concentrations of cytokine-induced neutrophil chemoattractant-1 in septic rats. J Anesth 22:27–31
Roviezzo F, Cuzzocrea S, Di Lorenzo A, Brancaleone V, Mazzon E, Di Paola R, Bucci M, Cirino G (2007) Protective role of PI3-kinase-Akt-eNOS signalling pathway in intestinal injury associated with splanchnic artery occlusion shock. Br J Pharmacol 151:377–383
Yamaguchi K, Kawahara T, Kumakura S, Hua J, Kugimiya T, Nagaoka I, Inada E (2009) Effect of olprinone a phosphodiesterase III inhibitor, on hepatic ischemiareperfusion injury in rats. Shock, Augusta
Genovese T, Esposito E, Mazzon E, Crisafulli C, Paterniti I, Di Paola R, Galuppo M, Bramanti P, Cuzzocrea S (2009) PPAR-? modulate the anti-inflammatory effect of glucocorticoids in the secondary damage in experimental spinal cord trauma. Pharmacol Res 59:338–350
Cuzzocrea S, Zingarelli B, Caputi AP (1998) Role of peroxynitrite and poly (ADP-ribosyl) synthetase activation in cardiovascular derangement induced by zymosan in the rat. Life Sci 63:923–933
Cuzzocrea S, Zingarelli B, Caputi AP (1998) Role of constitutive nitric oxide synthase and peroxynitrite production in a rat model of splanchnic artery occlusion shock. Life Sci 63:789–799
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358
Cuzzocrea S, Mazzon E, De Sarro A, Caputi AP (2000) Role of free radicals and poly (ADP-ribose) synthetase in intestinal tight junction permeability. Mol Med 6:766–778
Anas C, Ozaki T, Maruyama S, Yamamoto T, Zu Gotoh M, Ono Y, Matsuo S (2007) Effects of olprinone, a phosphodiesterase III inhibitor, on ischemic acute renal failure. Int J Urol 14:219–225
Matsumoto T, Kobayashi T, Kamata K (2003) Alterations in EDHF-type relaxation and phosphodiesterase activity in mesenteric arteries from diabetic rats. Am J Physiol Heart Circ Physiol 285:H283–H291
Zager RA, Johnson AC, Hanson SY, Lund S (2005) Ischemic proximal tubular injury primes mice to endotoxin-induced TNF-alpha generation and systemic release. Am J Physiol 289:F289–F297
Koga S, Morris S, Ogawa S, Liao H, Bilezikian JP, Chen G, Thompson WJ, Ashikaga T, Brett J, Stern DM et al (1995) TNF modulates endothelial properties by decreasing cAMP. Am J Physiol 268:C1104–C1113
Rahman A, Anwar KN, Minhajuddin M, Bijli KM, Javaid K, True AL, Malik AB (2004) cAMP targeting of p38 MAP kinase inhibits thrombin-induced NF-kappaB activation and ICAM-1 expression in endothelial cells. Am J Physiol Lung Cell Mol Physiol 287:L1017–L1024
Aizawa T, Wei H, Miano JM, Abe J, Berk BC, Yan C (2003) Role of phosphodiesterase 3 in NO/cGMP-mediated antiinflammatory effects in vascular smooth muscle cells. Circ Res 93:406–413
Salvemini D, Muscoli C, Riley DP, Cuzzocrea S (2002) Superoxide dismutase mimetics. Pulm Pharmacol Ther 15:439–447
Hassa PO, Hottiger MO (2002) The functional role of poly (ADP-ribose)polymerase 1 as novel coactivator of NF-kappaB in inflammatory disorders. Cell Mol Life Sci 59:1534–1553
Giovannelli L, Cozzi A, Guarnieri I, Dolara P, Moroni F (2002) Comet assay as a novel approach for studying DNA damage in focal cerebral ischemia: differential effects of NMDA receptor antagonists and poly (ADP-ribose) polymerase inhibitors. J Cereb Blood Flow Metab 22:697–704
Itoh G, Tamura J, Suzuki M, Suzuki Y, Ikeda H, Koike M, Nomura M, Jie T, Ito K (1995) DNA fragmentation of human infarcted myocardial cells demonstrated by the nick end labeling method and DNA agarose gel electrophoresis. Am J Pathol 146:1325–1331
Noda T, Iwakiri R, Fujimoto K, Matsuo S, Aw TY (1998) Programmed cell death induced by ischemia-reperfusion in rat intestinal mucosa. Am J Physiol 274:G270–G276
Fukuda K, Kojiro M, Chiu JF (1993) Induction of apoptosis by transforming growth factor-beta 1 in the rat hepatoma cell line McA-RH7777: a possible association with tissue transglutaminase expression. Hepatology 18:945–953
Masini E, Cuzzocrea S, Bani D, Mazzon E, Muja C, Mastroianni R, Fabrizi F, Pietrangeli P, Marcocci L, Mondovi B, Mannaioni PF, Federico R (2007) Beneficial effects of a plant histaminase in a rat model of splanchnic artery occlusion and reperfusion. Shock 27:409–415
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Crisafulli, C., Mazzon, E., Galuppo, M. et al. Olprinone attenuates the development of ischemia/reperfusion injury of the gut. Intensive Care Med 36, 1235–1247 (2010). https://doi.org/10.1007/s00134-010-1798-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-1798-4