Abstract
Objective: To examine practices of French intensivists regarding the management of mechanically ventilated patients with Candida-positive airway specimens but no major risk factors for immunodepression. Design : Closed-item questionnaire with a clinical vignette. Setting: 564 French intensive care units (ICUs). Participants: 198 intensivists who have a special interest in infectious diseases and who answered the questionnaire (response rate, 35.1%). Intervention: None. Measurements and results: The respondents recommended bronchoalveolar lavage (62.6% of respondents), protected distal sampling and protected specimen brush (59.1%), transbronchial biopsy (38.9%), and tracheal aspiration (12.1%) for the diagnosis of candidal pneumonia. A positive airway specimen was felt by most respondents (83.3%) to indicate colonisation; 66.7% of respondents recommended tests for systemic candidiasis in this situation, and 56.5% serial sampling to compute the colonisation index. Azole derivatives were the preferred antifungal medications. The clinical vignette described a patient with chronic obstructive lung disease who required mechanical ventilation for an acute exacerbation and who had a tracheal aspirate positive for Candida. Responses varied widely, with 37.8% of respondents diagnosing clinically insignificant colonisation but 24.2% recommending antifungal treatment and 61.6% serial testing to assess the Candida colonisation index. Intensivists with greater experience with severely immunocompromised patients were more aggressive in their diagnostic management. Conclusions: Wide variations occur among practices of French intensivists regarding Candida-positive airway specimens in patients without major risk factors for immunodepression. Additional studies are needed to improve our understanding of the links between Candida colonisation and infection and to determine the indications for pre-emptive antifungal treatment in non-neutropenic critically ill patients.
Similar content being viewed by others
Introduction
Candida is a normal inhabitant of the oral cavity and gastrointestinal tract that proliferates in patients with immunodepression. Thus, Candida colonisation and infection occur in close association with chemotherapy and radiation therapy for cancer and haematological malignancies, HIV infection, malnutrition, steroid therapy, and broad-spectrum antibiotics [1]. Differentiating colonisation from infection is a challenging and important problem: whereas systemic antifungal treatment is in order in patients with infection, colonisation is not always clinically significant. According to recently developed criteria, a diagnosis of Candida infection requires a positive blood culture, a positive culture from a normally sterile site (other than the urine and sinuses), or a histologically positive biopsy specimen [2].
Although the distinction between colonisation and infection is important, studies in ICU and surgical patients have confirmed that a continuum exists from colonisation to infection with Candida. Colonisation is an independent risk factor for systemic candidiasis [3, 4, 5]. Pittet et al. have shown, in surgical patients, that routine serial testing for colonisation at multiple sites (trachea, urine, skin, stool, surgical wounds, and drainage fluids) can be used to define a colonisation index (number of positive sites/number of tested sites) [6]. A colonisation index greater than 0.5 is associated with an increased risk of deep-seated candidal infection. It has been suggested that pre-emptive antifungal treatment may be in order in patients with a colonisation index greater than 0.5 [7].
Invasive pulmonary candidiasis occurs as a metastatic complication of candidemia, often at the terminal stage of a malignant disease with profound immunodepression [8]. In the intensive care unit (ICU) many patients without invasive candidiasis have respiratory specimens containing Candida counts above the “thresholds” validated for distinguishing bacterial colonisation from nosocomial pneumonia [9]. In ICU patients, airway colonisation by Candida probably reflects immune paralysis, with alterations in both neutrophil and alveolar macrophage function [10, 11]. It may therefore indicate a high risk of invasive candidiasis. The EPIC study, a 1995 prevalence survey of nosocomial infection in European ICUs, found that 17% of ICU-acquired infections were related to yeasts, primarily Candida [9]. The National Nosocomial Infections Surveillance system in the United States showed that Candida species were responsible for 10.1% of all ICU-acquired infections between 1980 and 1990 [12]. Furthermore, the incidence of Candida infection in hospital patients climbed steadily over the study period, increasing 5-fold for candidemia, 2-fold for urinary tract infections, and 1.6-fold for pneumonia [12]. Other studies have reported nosocomial Candida pneumonia in patient subgroups sharing factors such as ICU admission or postoperative status [6, 13, 14]. Candida pneumonia has also been described in patients with diabetes mellitus or alcohol abuse. Pharyngeal colonisation by yeasts is common in these patients [15, 16].
At the lung, the colonisation/infection dichotomy is supported by evidence from both clinical and autopsy studies. Candidal “pneumonia” seems to exist as two very different conditions. One is secondary to haematogenous dissemination with selective tropism for the blood vessels. This is probably true candidal pneumonia, with invasion of the lung parenchyma [8, 17, 18]. In the other variant, Candida colonizing the oropharynx and gastrointestinal tract spreads along the respiratory tract, ultimately filling the alveoli, so that endobronchial specimens are positive, but no clinical or pathological evidence of pneumonia is detectable [19]. Clinical studies consistently support this distinction. Two studies investigated the clinical relevance of “positive” tracheal or protected distal specimens, bronchoalveolar lavage fluid, or bronchial or transbronchial biopsies in ICU patients who received mechanical ventilation for longer than 2 days [20, 21] and had showed no evidence of systemic candidiasis. In most patients, lung biopsies or lung autopsy specimens found tracheobronchial colonisation without evidence of invasive candidiasis despite positive respiratory specimens. In one study, alveolitis was found in several patients, but there was no evidence of a causal relation with Candida since other organisms were usually present also [20]. These data emphasize the poor correlation between respiratory samples yielding Candida (colonisation) and invasive pulmonary candidiasis. Thus, the usual diagnostic criteria for nosocomial pneumonia do not seem valid for pulmonary candidiasis. To date, however, no other criteria have been established for diagnosing invasive pulmonary candidiasis. Thus recovery of Candida from the respiratory tract of a critically ill, mechanically ventilated patient without risk factors for immunodepression is both common and difficult to interpret. We conducted a survey to describe the practices of French intensivists in this situation.
Methods
A questionnaire and a clinical vignette were sent in March 2001 to the attending intensivists specialised in infectious diseases in 564 ICUs throughout France (one per ICU). The questionnaire was sent to all the ICUs located in metropolitan France fulfilling the following criteria: medical or surgical ICU in private or public hospitals, managing only adult patients, ICUs of more than six beds and more than two attending physicians. When in a given ICU no intensivist specialised in infectious diseases, the questionnaire was sent to the head of department. After six weeks, non-responders were randomised and the authors (E.A., Y.C. and J.R.Z.) tried to reach 25% of the non responders by telephone.
We developed the questionnaire based on a literature review and on the problems we had been encountering with Candida colonisation/infection in our everyday practices. We elected to develop a simple, short, closed-ended questionnaire using items appropriate for gathering data on current practices regarding Candida pneumonia in critically ill patients. The clinical vignette described a situation likely to be encountered frequently in the study ICUs. Preliminary questionnaires and scenarios were developed during discussions held by the investigators at the annual conference of the Outcomerea study group. Items were selected by a group of three investigators (E.A., J.F.T., and Y.C.) and redundant items were removed. Then, further discussions were held to develop the response options. The items collected three groups of data:
-
1.
Characteristics of the respondents and ICUs (type of hospital and case mix, including whether at least 5% of admitted patients had immune deficiencies related to neutropenia, HIV infection, or transplantation); and respondents’ standard protocols for diagnosing nosocomial pneumonia (invasive or non-invasive specimens, specimen collection before or after antibiotic treatment initiation)
-
2.
Number of cases considered by the respondent to be Candida pneumonia diagnosed per year in the ICU, as the absolute number and as the percentage of all cases of nosocomial pneumonia
-
3.
Means used by the respondents for confirming the diagnosis in non-neutropenic mechanically ventilated patients with suspected Candida pneumonia, and preferred treatment, should the diagnosis be confirmed
The clinical vignette was written to reflect the focus of our study, namely, practices of intensivists in critically ill, mechanically ventilated patients without profound immunodepression but with a positive respiratory tract specimen for Candida. The fictional patient was a 55-year-old man using long-term oxygen therapy at home for severe, chronic obstructive pulmonary disease. For the last 5 days, he had been taking prednisone (1 mg/kg) and amoxicillin+clavulanate (3 g/day) because of purulent sputum without increased dyspnea. He was referred to the ICU because of worsening respiratory failure rapidly requiring mechanical ventilation. The chest radiograph was unchanged, body temperature was 38.3°C, and the peripheral leukocyte count was 12,000/mm3. Mechanical ventilation and prednisone were continued. Unprotected tracheal aspiration was performed for microbiological studies, and the antibiotic was changed to cefotaxime (50 mg/kg/day). Two days later, a streptococcus and a Candida were isolated from the tracheal aspirate. On day 4, a consolidation in the right lower lobe and persistent fever and leukocytosis prompted a second tracheal aspiration, which recovered E. coli and Candida albicans. The respondents were asked what diagnostic and therapeutic measures they would take after receiving the results of the first and second tracheal aspirates positive for Candida.
Results are reported as medians (ranges). Groups were compared using the chi-square test for categorical variables (or Fisher’s exact test where appropriate) and the nonparametric Wilcoxon test for continuous variables (or the Kruskal-Wallis test where appropriate). P values ≤0.05 were considered statistically significant. Statistical tests were performed using the StatView 5.0 software package (SAS Institute, Cary, NC, USA).
Results
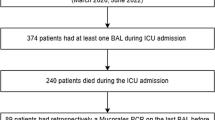
As reported in Fig. 1, among the 564 intensivists specialised in infectious diseases who received the questionnaire, 116 (20.6%) mailed back a completed questionnaire. Among the non-respondents, 25% (112/448) were selected at random for a telephone interview. This produced 82 additional completed questionnaires. The total response rate was 35.1% (198/564). Twenty respondents were called to obtain missing data. The 198 respondents did not differ from the 366 non-respondents in terms of location in France, type of ICU (respiratory, medical, surgical or mixed), number of ICU beds, or number of ICU physicians. Moreover, the group of respondents who mailed back a completed questionnaire and the group interviewed by telephone did not differ regarding any of the collected data, including the replies to the questionnaire and vignette.
General administrative data regarding the case mix
Among the respondents, 123 (62.4%) worked in medical-surgical ICUs, 35 (17.8%) in surgical ICUs, 24 (12.2%) in medical ICUs, and 15 (7.6%) in respiratory ICUs. More than half the ICUs were in teaching hospitals (115, 58%). In half the ICUs, more than 5% of admitted patients had immune deficiency related to neutropenia, HIV infection, or solid organ or bone marrow transplantation.
Specific questions about the usual approach to diagnosing VAP
Most respondents (152, 76.7%) routinely obtained invasive or non-invasive bronchial specimens before initiating antibiotics for pneumonia in mechanically ventilated patients, and 34 other respondents (17.2%) obtained pulmonary specimens within 24 hours after antibiotic initiation. The 12 remaining respondents did not seek to obtain microbiological documentation of ventilator-associated pneumonia (VAP). The 152 respondents who obtained microbiological specimens used one or two of the following techniques: bronchoalveolar lavage (BAL), 105 (53%) respondents; protected distal sampling, 88 (44.4%); distal bronchial brushing, 57 (28.7%); unprotected tracheal aspiration under fiberoptic bronchoscopy guidance, 33 (16.6%), or blind, unprotected tracheal aspiration, 16 (8%).
Epidemiological data about the incidence of cases diagnosed as Candida pneumonia
Respondents estimated that they diagnosed Candida pneumonia in two patients every year (0–10) and that Candida contributed 2% of all cases of nosocomial pneumonia in their ICU (0–14). BAL was considered a useful diagnostic procedure for Candida pneumonia by 124 (62.6%) respondents, protected distal sampling and distal bronchial brushing by 117 (59.1%), transbronchial biopsies by 77 (38.9%), and tracheal aspiration by 24 (12.1%). Most (165, 83.3%) respondents considered that a positive specimen for Candida indicated colonisation. Nevertheless, in this situation, 132 (132/198, 66.6%) respondents reported that they performed tests to eliminate systemic candidiasis, and 112 (112/198, 56.6%) said that they obtained specimens from multiple body sites to compute the colonisation index. Azole derivatives were the preferred agents for treatment.
Respondents’ approach to solving a case in a clinical vignette
To the clinical vignette question regarding management of a case after the result of the first tracheal aspirate, 75 (37.8%) respondents answered that they would consider the presence of Candida clinically insignificant. Among the remaining 123 respondents, 48 (48/123, 39.0%) would initiate systemic antifungal treatment and 61 (61/123, 49.6%) would give oral amphotericin B for gastrointestinal tract decontamination. Among the 198 respondents, 122 (122/198, 61.6%) would obtain serial specimens from multiple body sites to monitor the Candida colonisation index.
To the question as to how they would respond to the result of the second tracheal aspirate, which is positive for Candida and E. coli on day 4, 57 (28.7%) respondents answered that the Candida was not clinically significant; all but four of these 57 respondents were among the 75 who said the presence of Candida in the first specimen was clinically insignificant. Among the 141 other respondents, 55 (55/141, 39.0%) would give systemic antifungal treatment (the 48 respondents who recommended this treatment after the first specimen and seven additional respondents) and 34 (34/141, 24.1%) would give oral amphotericin B for gastrointestinal tract decontamination. Half the respondents (99, 50%) would obtain serial specimens from multiple body sites to monitor the Candida colonisation index. Less than half the respondents (94, 47.5%) stated that fiberoptic bronchoscopy was in order; among them, 91 (91/198, 45.9%) would perform BAL, and 90 (90/198, 45.4%) would perform protected distal sampling/bronchial brushing; 89 would do both. Among the respondents who would perform BAL and/or protected distal sampling, 86 (86/91, 94.5%) of the former and 72 (72/90, 80.0%) of the latter would order specific mycological studies on the specimens. Finally, among the respondents who recommended fiberoptic bronchoscopy, assuming the respiratory samples yielded Candida (in any concentration), 75 (75/198, 37%) would give antifungal therapy if the colonisation index was 3/5 (3 of 5 sites positive), as compared to 107 (107/198, 54%) if the colonisation index was 4/5 (4 of 5 sites positive).
Practices differed significantly between respondents, depending on whether or not they had extensive experience with profoundly immunodeficient patients. In the responses to both the questionnaire and the vignette, respondents working in ICUs in which more than 5% of patients had profound immunodeficiency related to neutropenia, HIV infection, or a transplant were more likely to consider that a positive airway specimen for Candida was clinically insignificant (43.4% vs 32.3%, p=0.02) and were less likely to initiate systemic antifungal therapy at admission (16.1% vs 32.3%, p=0.01). These respondents were more likely to recommend transbronchial biopsies for diagnosing Candida pneumonia (48.4% vs 29.2%, p=0.04), to perform BAL for investigating a tracheal aspirate positive for Candida (49.5% vs 42.4%, p=0.05), and to request specific mycological studies on the BAL fluid (49.5% vs 37.3%, p=0.03). Moreover, when systemic antifungal therapy was considered, they were more likely to give systemic antifungal treatment to patients with a colonisation index of 4/5 (63.6% vs 44.4%, p=0.003) and to use fluconazole in a dosage of 400 rather than 800 mg per day (57% vs 27%, p=0.02). There were no significant differences between intensivists from medical, surgical or multipurpose ICUs.
Discussion
Guidelines exist for the management of patients with profound immunodepression and specimens positive for Candida. [22] We elected to examine another situation, for which no guidelines are available, namely, presence of Candida in an airway specimen from a critically ill, mechanically ventilated patient without profound immunodepression. Even in this situation, airway specimens yielding Candida (in counts above or below the thresholds used to diagnose bacterial pneumonia) are clinically relevant: they indicate “relative” immunodepression, particularly in ICU patients or after surgery (post-injury immunodepression) [10, 23]. Consequently, the appropriateness of pre-emptive antifungal treatment should be evaluated. Because a respiratory specimen yielding Candida merely indicates bronchial colonisation, a search for colonisation at other sites is in order to allow evaluation of the colonisation index. In surgical patients, this is known to correlate well with secondary emergence of systemic candidiasis [6, 7, 24, 25].
The results of our questionnaire and clinical-vignette survey provide information on practices of French intensivists regarding the management of non-neutropenic, critically ill patients with respiratory specimens positive for Candida. The considerable variability in the answers across respondents reflects a need for developing a consensus about Candida airway colonisation, its significance relative to colonisation at other body sites, and its association with the frequency and pathogenesis of invasive pulmonary candidiasis. Studies are needed to obtain the knowledge on which to build such a consensus. We found substantial differences in practices between respondents who had extensive experience with immunocompromised patients and those who did not have this level of experience. Respondents in ICUs in which more than 5% of patients were profoundly immunocompromised proved more aggressive in diagnostic and therapeutic approach, suggesting that they may have applied guidelines for severely immunodeficient patients to the vignette. Again, studies are in order to determine whether this approach is warranted.
Evidence from several studies indicates that candidemia carries a poor prognosis and, consequently, requires early diagnosis and/or prophylactic measures [4, 26, 27]. The beneficial effect of preventive antifungal treatment to prevent candidemia has been documented in haematology patients [28, 29] and suggested by several ICU studies [24, 25, 30, 31]. However, to date, no studies have been conducted to determine whether prophylactic or pre-emptive treatment is beneficial in non-neutropenic, mechanically ventilated, critically ill patients with respiratory specimens positive for Candida. Prevention is essential, given the high mortality associated with invasive candidal pneumonia. Thus, in a study conducted at the National Taiwan University Hospital [32], 140 cases of invasive fungal pneumonia were identified over the 10-year study period, including 20 due to Candida. Histological confirmation of the diagnosis was obtained in all patients (by examination of lung biopsies obtained by thoracotomy or thoracoscopy, of percutaneous pleural or lung biopsies obtained under ultrasound guidance, or of transbronchial biopsies). Candida was associated with a 70% mortality rate, the highest rate among causes of fungal pneumonia [32].
Our study has the methodological limitations inherent in a closed-ended questionnaire survey. However, the response options were developed by discussion among three of the study investigators, based on their clinical practice. Another limitation is that we investigated a fictional case rather than actual practice. Indeed, the patient reported in our case could be viewed as not representative of the majority of patients presenting Candida in their respiratory samples, since he had a severe underlying disease, received steroids and presented positive tracheal aspirate on admission rather than days after the onset of mechanical ventilation. Furthermore, the haziness that surrounds the term “Candida pneumonia” must be given consideration when interpreting our results. Our questionnaire did not provide a definition of candidal pneumonia. The median number of cases of “Candida pneumonia”, as estimated by our respondents, was two per ICU. The number of patients with true pneumonia, defined as invasive candidal infection of the lung parenchyma, was probably far smaller. Moreover, French intensivists, perhaps because they reach a high level of training, may be viewed as particularly aggressive in their management of patients suspected to have VAP. Finally, the response rate in our study was 35.1%. Although this rate was disappointingly low, our comparison of respondents and non-respondents found no differences, indicating that our study sample was probably representative of the source population.
Further studies of Candida airway colonisation and invasive pneumonia will have to determine the following: the Candida species responsible for colonisation and infection; the morbidity and mortality related to Candida colonisation; the risk factors for airway colonisation; and the factors indicating a high likelihood of beneficial effects from pre-emptive systemic antifungal therapy. Also of use would be therapeutic trials to assess the potential benefits of pre-emptive antifungal therapy in non-neutropenic, mechanically ventilated, critically ill patients. In these trials, an important methodological precaution would be stratification on the colonisation index and on ICU case-mix variability, particularly regarding the proportion of immunocompromised patients.
References
Bodey GP (1984) Candidiasis in cancer patients. Am J Med 77:13–19
Ascioglu S, Rex JH, de Pauw B, Bennett JE, Bille J, Crokaert F, Denning DW, Donnelly JP, Edwards JE, Erjavec Z, Fiere D, Lortholary O, Maertens J, Meis JF, Patterson TF, Ritter J, Selleslag D, Shah PM, Stevens DA, Walsh TJ (2002) Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: an international consensus. Clin Infect Dis 34:7–14
Wey SB, Mori M, Pfaller MA, Woolson RF, Wenzel RP (1989) Risk factors for hospital-acquired candidemia. A matched case-control study. Arch Intern Med 149:2349–2353
Petri MG, Konig J, Moecke HP, Gramm HJ, Barkow H, Kujath P, Dennhart R, Schafer H, Meyer N, Kalmar P, Thulig P, Muller J, Lode H (1997) Epidemiology of invasive mycosis in ICU patients: a prospective multicenter study in 435 non-neutropenic patients. Paul-Ehrlich Society for Chemotherapy, Divisions of Mycology and Pneumonia Research. Intensive Care Med 23:317–325
Eubanks PJ, de Virgilio C, Klein S, Bongard F (1993) Candida sepsis in surgical patients. Am J Surg 166:617–619; discussion 619–20
Pittet D, Monod M, Suter PM, Frenk E, Auckenthaler R (1994) Candida colonization and subsequent infections in critically ill surgical patients. Ann Surg 220:751–758
Eggimann P, Pittet D (2001) Candidiasis among non-neutropenic patients: from colonization to infection. Ann Fr Anesth Reanim 20:382–388
Masur H, Rosen PP, Armstrong D (1977) Pulmonary disease caused by Candida species. Am J Med 63:914–925
Vincent JL, Bihari DJ, Suter PM, Bruining HA, White J, Nicolas-Chanoin MH, Wolff M, Spencer RC, Hemmer M (1995) The prevalence of nosocomial infection in intensive care units in Europe. Results of the European Prevalence of Infection in Intensive Care (EPIC) Study. EPIC International Advisory Committee. JAMA 274:639–644
Stephan F, Yang K, Tankovic J, Soussy CJ, Dhonneur G, Duvaldestin P, Brochard L, Brun-Buisson C, Harf A, Delclaux C (2002) Impairment of polymorphonuclear neutrophil functions precedes nosocomial infections in critically ill patients. Crit Care Med 30:315–322
Kox WJ, Volk T, Kox SN, Volk HD (2000) Immunomodulatory therapies in sepsis. Intensive Care Med 26:S124–128
Jarvis WR (1995) Epidemiology of nosocomial fungal infections, with emphasis on Candida species. Clin Infect Dis 20:1526–1530
Eggimann P, Francioli P, Bille J, Schneider R, Wu MM, Chapuis G, Chiolero R, Pannatier A, Schilling J, Geroulanos S, Glauser MP, Calandra T (1999) Fluconazole prophylaxis prevents intra-abdominal candidiasis in high-risk surgical patients. Crit Care Med 27:1066–1072
Vincent JL, Anaissie E, Bruining H, Demajo W, el-Ebiary M, Haber J, Hiramatsu Y, Nitenberg G, Nystrom PO, Pittet D, Rogers T, Sandven P, Sganga G, Schaller MD, Solomkin J (1998) Epidemiology, diagnosis and treatment of systemic Candida infection in surgical patients under intensive care. Intensive Care Med 24:206–216
Fernandez-Sola J, Junque A, Estruch R, Monforte R, Torres A, Urbano-Marquez A (1995) High alcohol intake as a risk and prognostic factor for community-acquired pneumonia. Arch Intern Med 155:1649–1654
Wheat LJ (1980) Infection and diabetes mellitus. Diabetes Care 3:187–197
Haron E, Vartivarian S, Anaissie E, Dekmezian R, Bodey GP (1993) Primary Candida pneumonia. Experience at a large cancer center and review of the literature. Medicine (Baltimore) 72:137–142
Rose HD, Sheth NK (1978) Pulmonary candidiasis. A clinical and pathological correlation. Arch Intern Med 138:964–965
Azoulay E, Limal N, Mayaud C, Schlemmer B (2001) Bronchial specimens positive to Candida: infection or colonization. Réanimation Urgences 10:323–328
el-Ebiary M, Torres A, Fabregas N, de la Bellacasa JP, Gonzalez J, Ramirez J, del Bano D, Hernandez C, Jimenez de Anta MT (1997) Significance of the isolation of Candida species from respiratory samples in critically ill, non-neutropenic patients. An immediate postmortem histologic study. Am J Respir Crit Care Med 156:583–590
Rello J, Esandi ME, Diaz E, Mariscal D, Gallego M, Valles J (1998) The role of Candida sp isolated from bronchoscopic samples in non-neutropenic patients. Chest 114:146–149
Rex JH, Walsh TJ, Sobel JD, Filler SG, Pappas PG, Dismukes WE, Edwards JE (2000) Practice guidelines for the treatment of candidiasis. Infectious Diseases Society of America. Clin Infect Dis 30:662–678
Ahmed NA, McGill S, Yee J, Hu F, Michel RP, Christou NV (1999) Mechanisms for the diminished neutrophil exudation to secondary inflammatory sites in infected patients with a systemic inflammatory response (sepsis). Crit Care Med 27:2459–2468
Calandra T, Marchetti O (2002) Antifungal prophylaxis for intensive care unit patients: let’s fine tune it. Intensive Care Med 28(12):1698–1700
Garbino J, Lew D, Romand JA, Hugonnet S, Auckenthaler R, Pittet D (2002) Prevention of severe Candida infections in non-neutropenic, high-risk, critically ill patients. A randomized, double-blind, placebo-controlled trial in SDD-treated patients. Intensive Care Med 28(12):1708-1717
Trick WE, Fridkin SK, Edwards JR, Hajjeh RA, Gaynes RP (2002) Secular trend of hospital-acquired candidemia among intensive care unit patients in the United States during 1989–1999. Clin Infect Dis 35:627–630
Rangel-Frausto MS, Wiblin T, Blumberg HM, Saiman L, Patterson J, Rinaldi M, Pfaller M, Edwards JE, Jarvis W, Dawson J, Wenzel RP (1999) National epidemiology of mycoses survey (NEMIS): variations in rates of bloodstream infections due to Candida species in seven surgical intensive care units and six neonatal intensive care units. Clin Infect Dis 29:253–258
Goodman JL, Winston DJ, Greenfield RA, Chandrasekar PH, Fox B, Kaizer H, Shadduck RK, Shea TC, Stiff P, Friedman DJ et al (1992) A controlled trial of fluconazole to prevent fungal infections in patients undergoing bone marrow transplantation. N Engl J Med 326:845–851
Winston DJ, Chandrasekar PH, Lazarus HM, Goodman JL, Silber JL, Horowitz H, Shadduck RK, Rosenfeld CS, Ho WG, Islam MZ et al (1993) Fluconazole prophylaxis of fungal infections in patients with acute leukemia. Results of a randomized placebo-controlled, double-blind, multicenter trial. Ann Intern Med 118:495–503
Pelz RK, Hendrix CW, Swoboda SM, Diener-West M, Merz WG, Hammond J, Lipsett PA (2001) Double-blind placebo-controlled trial of fluconazole to prevent candidal infections in critically ill surgical patients. Ann Surg 233:542–548
Rex JH, Sobel JD (2001) Prophylactic antifungal therapy in the intensive care unit. Clin Infect Dis 32:1191–1200
Chen KY, Ko SC, Hsueh PR, Luh KT, Yang PC (2001) Pulmonary fungal infection: emphasis on microbiological spectra, patient outcome, and prognostic factors. Chest 120:177–184
Acknowledgements
This study was supported by an educational grant from Pfizer, France, and performed on behalf of the Outcomerea study group
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented in January 2002 at the congress of the French Society of Critical Care Medicine
Rights and permissions
About this article
Cite this article
Azoulay, E., Cohen, Y., Zahar, JR. et al. Practices in non-neutropenic ICU patients with Candida-positive airway specimens. Intensive Care Med 30, 1384–1389 (2004). https://doi.org/10.1007/s00134-004-2316-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2316-3