Abstract
Objective
To evaluate the extent to which respiratory changes in inferior vena cava (IVC) diameter can be used to predict fluid responsiveness.
Design
Prospective clinical study.
Setting
Hospital intensive care unit.
Patients
Twenty-three patients with acute circulatory failure related to sepsis and mechanically ventilated because of an acute lung injury.
Measurements
Inferior vena cava diameter (D) at end-expiration (Dmin) and at end-inspiration (Dmax) was measured by echocardiography using a subcostal approach. The distensibility index of the IVC (dIVC) was calculated as the ratio of Dmax − Dmin / Dmin, and expressed as a percentage. The Doppler technique was applied in the pulmonary artery trunk to determine cardiac index (CI). Measurements were performed at baseline and after a 7 ml/kg volume expansion using a plasma expander. Patients were separated into responders (increase in CI ≥15%) and non-responders (increase in CI <15%).
Results
Using a threshold dIVC of 18%, responders and non-responders were discriminated with 90% sensitivity and 90% specificity. A strong relation (r=0.9) was observed between dIVC at baseline and the CI increase following blood volume expansion. Baseline central venous pressure did not accurately predict fluid responsiveness.
Conclusion
Our study suggests that respiratory change in IVC diameter is an accurate predictor of fluid responsiveness in septic patients.
Similar content being viewed by others
Introduction
Circulatory failure in patients presenting septic shock is often the result of hypovolemia, which must be corrected. Volume expansion improves prognosis in this indication [1], whereas inappropriate use of vasoconstrictors leads to harmful tissue hypoperfusion [2]. However, volume expansion may prove ineffective or even deleterious through worsening of a pre-existing heart failure [3, 4] or by degrading gas exchanges in a patient ventilated for ARDS. It is therefore essential to have reliable tools to predict the efficacy of volume expansion.
Tools proposed hitherto have proven insufficiently reliable, whether invasive like the measurement of central venous pressure and pulmonary capillary wedge pressure, or non-invasive like the echocardiographic measurement of cavity size in diastole [5]. Only variation in pulse pressure currently seems to be a good predictor of the response to volume expansion [6].
Echocardiography is a non-invasive procedure which enables full assessment of cardiac function. The inferior vena cava (IVC) may be visualized by a subcostal approach,. The IVC is a compliant blood vessel, easily distended, especially in cases of hypovolemia [7]. The aim of our study was to test the hypothesis that respiratory changes in IVC diameter in mechanically ventilated patients could predict the efficacy of volume expansion.
Patients and methods
Patients
This prospective study was conducted over a 7-month period (January–July 2003) in the medical-surgical intensive care unit of the Poissy-Saint-Germain-en-Laye hospital center. Ventilated patients (>18 years of age) were included when they presented circulatory failure related to severe sepsis. Circulatory failure was defined by a systolic arterial pressure below 90 mmHg and/or perfusion of vasopressor amines. Sepsis was defined according to American Consensus Conference criteria [8].
Mechanical ventilation was performed in volume mode using a Horus ventilator (Taema) or a Servo Ventilator 300 (Siemens). The study needed perfect adaptation of the patient to the ventilator before starting the respiration cycle. Ventilatory parameters were as follows: tidal volume 8.5±1.5 ml/kg, breathing rate 15±2 breaths/min, PEEP 4±2 cmH2O. The plateau pressure was kept below 30 cmH2O.
This study was approved by the Saint-Germain-en-Laye Hospital Consultative Ethics Committee, without the need for a consent form.
Methods
Pressure measurements
Heart rate (HR) and systemic arterial pressure were monitored continuously using a radial or femoral artery catheter. Central venous pressure (CVP) was measured with an internal jugular or subclavian catheter, inserted beforehand in view of the patient’s condition. CVP was measured at end-expiration. All patients were monitored with a nail-bed oximeter.
In the last six patients included in the study, we also evaluated respiratory changes in abdominal pressure by measuring intravesical pressure, as previously reported [9]. Pressure values were thus measured at end-expiration and end-inspiration.
Transthoracic echocardiographic measurements
Doppler echocardiography was performed using a Philips ATL HDI 3500 CV system equipped with a phased array transthoracic probe (1.67–3.2 MHz). Synchronization of the measurements with the different times of the ventilatory cycle was verified by insertion of a pressure signal. Measurements were recorded on videotape for later review by a second operator not aware of fluid responsiveness.
The IVC was examined subcostally in longitudinal section. Its diameter was measured in M-mode coupled to two-dimensional mode, just upstream of the origin of the suprahepatic vein. Measurements were validated when the M-mode tracing was exactly perpendicular to the IVC. The distensibility index of the IVC (dIVC), which reflects the increase in its diameter on inspiration, was calculated as (maximum diameter on inspiration − minimum diameter on expiration) / minimum diameter on expiration. Intra- and inter-observer variabilities in the measurement of IVC diameter were 6.3±8 and 8.7±9%, respectively.
The cardiac index (CI) was calculated from the right ventricular outflow tract, as previously proposed [10]. From an echocardiographic subcostal view, the velocity-time integral (VTI) was measured in pulsed Doppler mode at the pulmonary annulus and averaged over the whole respiratory cycle. The velocity-time integrals were validated when we visualized the opening and the closing click of the pulmonary valve. The diameter of the pulmonary annulus (D) was also measured. The CI was calculated using the following formula:
Study protocol
All clinical and echocardiographic measurements were performed before (T0) and again immediately after (T1) a 30-min volume expansion (7 ml/kg) using 4% modified fluid gelatin.
Statistical analysis
For all patients, the non-parametric Wilcoxon test was used to compare paired values at T0 and T1. The non-parametric Mann-Whitney test was used to compare unpaired values. The patients were separated into two groups depending on the change in CI after volume expansion: responders, whose cardiac index increased 15% or more, and non-responders, whose increase was less than 15%. A receiver operating characteristic (ROC) curve was plotted to determine the threshold value of dIVC which provided the prediction of the response to volume expansion with the best sensitivity and specificity, using MedCalc statistical software.
Results
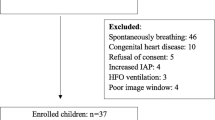
Three of the 23 patients initially included in the study were excluded because their poor response to echocardiography rendered data analysis difficult. Two of them had undergone laparotomy and the third was morbidly obese. Echocardiography coupled to volume expansion was straightforward in the other 20 patients (15 men and 5 women). The mean age of the patients was 63±15 years and the SAPS II score was 60±21. Their diagnoses are listed in Table 1. Six patients had ARDS, according to the criteria of the North American-European Consensus. One patient developed acute cor pulmonale at echocardiography. Five patients were given epinephrine (mean dose 0.31±0.2 µg/kg per min), seven norepinephrine (mean dose 0.5±0.5 µg/kg per min), four dobutamine (mean dose 11±2.5 µg/kg per min) and two dopamine (mean dose 10±3.8 µg/kg per min).
Table 2 shows the hemodynamic data in the overall population before and after volume expansion. Volume expansion significantly increased the mean CI from 2.7±1.2 to 3±1.2 l/min per m2 (p<0.05). However, ten patients were responders and ten non-responders. As shown in Table 3, only dIVC differed significantly between the two groups (40±24% for responders versus 8±8% for non-responders; p<0.05). An example of the calculation of dIVC for each group is given in Fig. 1. Table 4 lists the parameter changes after volume expansion in the two groups.
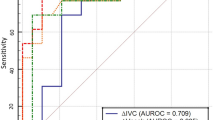
A dIVC value above 18% allowed prediction of the efficacy of volume expansion with 90% sensitivity and 90% specificity (Fig. 2). Figure 3 shows the change in CI of each patient as a function of this threshold value. There was a good correlation (r=0.9) between the IVC distensibility index at T0 and CI increase after volume expansion (Fig. 4). No significant difference was observed in doses of vasopressors between patients with dIVC greater or less than 18% (p=0.44). CVP was correlated neither with CI change (r=0.17, p=0.45) nor with dIVC (r=0.4, p=0.07) and did not allow prediction of the response to volume expansion (Fig. 2).
Receiver operating characteristic curve analysis of inferior vena cava distensibility index (dIVC) and central venous pressure (CVP) in prediction of fluid responsiveness. The areas under the curve (± SEM) were 0.91±0.07 and 0.57±0.13, respectively, p=0.008. Threshold values of dIVC and CVP are given with their respective sensibility, specificity, positive and negative likelihood ratios (+LR, -LR). Sensitivity and specificity of CVP are presented as the predictive value of a CVP lower than the threshold, whereas sensitivity and specificity of dIVC are presented as the predictive value of a dIVC higher than the threshold value
No difference between responders and non-responders was found regarding end-expiration and end-inspiration airway pressures, respiratory system compliance or change in pleural pressure related to tidal ventilation (Table 5). The mean change in abdominal pressure between the two phases of the ventilatory cycle, evaluated in six patients (three responders and three non-responders), was 1.35±0.1 cmH2O when the mean abdominal pressure was 14.6±2.3 cmH2O at end-expiration.
Discussion
Echocardiography has a history of reliable assessment of cardiac function in intensive care patients, notably in septic shock where the causes of circulatory failure are multiple and often overlap: hypovolemia, heart failure, vasoplegia. Echocardiography can be completed by the study of respiratory variations in the IVC. In our population of mechanically ventilated patients with septic shock we have shown that the IVC distensibility index was a good predictor of response to volume expansion. The poor predictive value of the CVP confirms previous findings [11, 12].
The IVC is a compliant blood vessel subject to abdominal pressure and acts as a reservoir [13]. Its caliber is altered by respiration [13], blood volume [14] and right heart function [15]. Takata et al. have reported abdominal vascular zone conditions that could explain the respiratory changes in IVC diameter [16]. In this study, the authors suggested that IVC diameter depended on the relation between the level of extra-mural IVC pressure, i.e. the abdominal pressure, and the level of the backward pressure, i.e. the right atrial pressure [16]. Moreover, this has been demonstrated by echocardiography in spontaneously breathing patients with severe acute asthma, in whom Jardin et al. observed inspiratory collapse of the IVC [17], mainly explained by a marked decrease in pleural pressure and then in right atrial pressure, associated with an increase in intra-abdominal pressure [17]. In addition, Kircher et al. showed that the observed inspiratory decrease in IVC diameter, expressed by the caval index (expiratory diameter − inspiratory diameter / expiratory diameter), was well correlated with right atrial pressure in spontaneous ventilation [18].
But this index is no longer valid in patients undergoing positive pressure ventilation [19, 20] since, in contrast to spontaneous ventilation, IVC diameter is maximal at inspiration and minimal on expiration [21]. On inspiration, the increase in pleural pressure leads to a rise in intravascular pressure of the right atrium and of the IVC. At the same time, the rise in abdominal pressure is less, since only 20% of the airway pressure is transmitted to the abdomen [22, 23]. This results in a rise in transmural pressure of the IVC. Applying a formula published by Jardin et al. [24], we calculated that the mean change in pleural pressure on inspiration was 5.3±1.4 cmH2O, whereas the change in intra-abdominal pressure was only 1.35±0.1 cmH2O in the six patients studied. Thus, the IVC dilates as transmural pressure rises, and dilation will be even greater if the IVC is easily distended because of a high compliance, as in hypovolemia [7].
As we have seen, changes in IVC diameter depend on the ventilation parameters. For a given plasma volume in a given patient, the increase in tidal volume and the application of PEEP can alter IVC diameter. This is, moreover, the principal usefulness of the recently studied dynamic indexes in predicting the response to volume expansion [6, 25, 26]: they take into account the “therapeutic” ventilation of patients and allow plasma volume to be adapted to the level of pressure. However, we did not observe significant differences between responders and non-responders in PEEP, plateau pressure or respiratory system compliance.
The study of respiratory variations in IVC diameter is limited in various ways in evaluating the efficacy of volume expansion. Certain patients (three (13%) in our study) respond poorly to echocardiography. Such patients are often obese or have undergone laparotomy and subcostal echocardiography is impossible. We also noted that changes in IVC diameter depended, among other parameters, on intra-abdominal pressure. In this way, we can hypothesize that the accurate value of changes in IVC diameter in predicting fluid responsiveness would not be demonstrated in patients with higher intra-abdominal pressures. This represents a significant limitation of routine use of the distensibility index of IVC. In our study, the intra-abdominal pressures, when measured, proved only slightly increased. Unfortunately, this was only measured in six patients, precluding any conclusion regarding the impact of intra-abdominal pressure on IVC diameter value. Lastly, the distensibility index of the IVC depends on IVC compliance. Plasma volume is not the only factor that could explain changes in IVC compliance. It is probable that the infusion of vasoconstrictors (14 patients in our study) can alter respiratory variation in IVC, as well as severe pulmonary hypertension.
In conclusion, evaluation of IVC distensibility by echocardiography can be of value in the management of ventilated intensive care patients. In circulatory failure during severe sepsis, a distensibility index above 18% is a good argument in favor of volume expansion. However, the impact of intra-abdominal pressure remains to be evaluated, especially in patients admitted to a surgical intensive care unit.
References
Weil MH, Nishjima (1978) Cardiac output in bacterial shock. Am J Med 64:920–922
Murakawa K, Kobayashi A (1988) Effect of vasopressors on renal tissue gas tensions during hemorrhagic shocks in dogs. Crit Care Med 16:789–792
Magder S (1992) Shock physiology. In: Pinsky MR, Dhainault JF (eds) Physiological foundation of critical care medicine. Williams and Wilkins, Philadelphia, pp 140–160
Guyton AC, Jones CE, Coleman TG (1973) Circulatory physiology: cardiac output and its regulation. Saunders, Philadelphia
Michard F, Teboul JL (2002) Predicting fluid responsiveness in ICU patients. A critical analysis of the evidence. Chest 121:2000–2008
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, Richard C, Pinsky MR, Teboul JL (2000) Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure . Am J Respir Crit Care Med 162:134–138
Comolet R (1984) Biomécanique Circulatoire. Abrégé Masson, pp 36–53
American College of Chest Physicians/Society of Critical Care Medicine Consensus conference (1992) Definitions for sepsis and organ failure and guidelines for use of innovative therapies in sepsis (review). Crit Care Med 27:864–874
Fusco MA, Shayn Martin R, Chang MC (2001) Estimation of intra-abdominal pressure by bladder pressure measurement: validity and methodology. J Trauma 50:297–302
Maslow A, Comunale ME, Haering JM, Watkins J (1996) Pulsed wave Doppler measurement of cardiac output from the right ventricular outflow tract. Anesth Analg 83:466–471
Calvin JE, Driedger AA, Sibbald WJ (1981) The hemodynamic effect of rapid fluid infusion in critically ill patients. Surgery 90:61–76
Reuse C, Vincent JL, Pinsky MR (1990) Measurements of right ventricular volumes during fluid challenge. Chest 98:1450–1454
Natori H, Tamaki S, Kira S (1979) Ultrasonographic evaluation of ventilatory effect on inferior vena caval configuration. Am Rev Respir Dis 120:421–427
Jeffrey RB, Federle MP (1988) The collapsed inferior vena cava: CT evidence of hypovolemia. Am J Roentgen 150:431–432
Nakao S, Come P, Mckay RG, Ransil BJ (1987) Effect of positional changes on inferior vena caval size and dynamics and correlation with right-sided cardiac pressure. Am J Cardiol 59:125–132
Takata M, Wise RA, Robotham JL (1990) Effect of abdominal pressure on venous return: abdominal vascular zone conditions. J Appl Physiol 69:1961–1972
Jardin F, Dubourg O, Margairaz A, Bourdarias JP (1987) Inspiratory impairment in right ventricular performance during acute asthma. Chest 92:789–795
Kircher BJ, Himelman RB, Schiller NB (1990) Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardiol 66:493–496
Nagueh SF, Kopelen HA, Zoghbi WA (1996) Relation of mean right atrial pressure to echocardiographic and Doppler parameters of the right atrial and right ventricular function. Circulation 93:1160–1169
Jue J, Chung W, Schiller NB (1992) Does inferior vena cava size predict right atrial pressures in patients receiving mechanical ventilation? J Am Soc Echocardiogr 5:613–619
Mitaka C, Nagura T, Sakanishi N, Tsunoda Y, Amaha K (1989) Two-dimensional echographic evaluation of inferior vena cava, right and left ventricle during positive-pressure ventilation with varying level of positive end-expiratory pressure. Crit Care Med 17:205–210
Van Den Berg PC, Jansen JRC, Pinsky MR (2002) Effect of positive pressure on venous return in volume-loaded surgical patients. J Appl Physiol 92:1223–1231
Antunes T, Anbar J, Barbas C (2003) Effects of PEEP and external abdominal weight on respiratory mechanics. Intensive Care Med 28:S34
Jardin F, Genevray B, Brun-Ney D, Bourdarias JP (1985) Influence of lung and chest wall compliance on transmission of airway pressure to the pleural space in critically ill patients. Chest 88:653–658
Vieillard-Baron A, Augarde R, Prin S, Page B, Beauchet A, Jardin F (2001) Influence of superior vena caval zone condition on cyclic changes in right ventricular outflow during respiratory support. Anesthesiology 95:1083–1088
Feissel M, Michard F, Mangin I, Ruyer O, Faller JP, Teboul JL (2001) Respiratory changes in aortic blood velocity as an indicator of fluid responsiveness in ventilated patients with septic shock. Chest 119:867–873
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barbier, C., Loubières, Y., Schmit, C. et al. Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients. Intensive Care Med 30, 1740–1746 (2004). https://doi.org/10.1007/s00134-004-2259-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2259-8