Abstract
Objective
To assess the effects of the angiotensin-converting enzyme (ACE) inhibitor (ACEI) perindopril on prolonged endothelial cell dysfunction in a rabbit endotoxic model.
Design
Randomized, controlled, interventional trial.
Setting
University animal laboratory.
Subjects
A total of 65 male New Zealand White rabbits, randomly assigned to one of eight groups.
Interventions
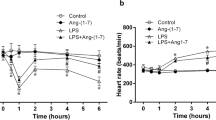
Endotoxic shock was induced by a single lipopolysaccharide (LPS, serotype O55:B5) bolus (0.5 mg.kg−1, i.v., Escherichia coli endotoxin). Coagulation factors and expression of monocyte tissue factor (TF) were determined by functional assay. Endothelium-dependent vascular relaxation was assessed by in vitro vascular reactivity. Immunohistochemical staining (CD31) was performed to assess endothelial injury of the abdominal aorta. These parameters were studied 5 days (D5) after the onset of endotoxic shock. Rabbits were randomized to receive perindopril (1 mg kg−1 day−1 orally) alone, or with NG-nitro-L-arginine methyl ester (L-NAME; 15 mg kg−1 day−1 orally), or L-NAME alone initiated 7 days before the onset of endotoxic shock and maintained for 5 days afterward.
Measurements and results
Perindopril prevented altered endothelium-dependent relaxation to acetylcholine induced by LPS injection (Emax=75.6±3.7 vs 42.3±9.4% in LPS group, p<0.05). This effect was inhibited by co-treatment with L-NAME. Perindopril had no effect on either LPS-induced endothelial histological injury or monocyte TF expression.
Conclusion
These data suggest that perindopril can prevent endothelial dysfunction in endotoxin-induced shock through an NO-dependent mechanism.





Similar content being viewed by others
References
Cotran RS, Pober JS (1990) Cytokine-endothelial interactions in inflammation, immunity, and vascular injury. J Am Soc Nephrol 1:225–235
Vallet B (1998) Vascular reactivity and tissue oxygenation. Intensive Care Med 24:3–11
Astiz ME, Rackow EC (1998) Septic shock. Lancet 351:1501–1505
Myers PR, Zhong Q, Jones JJ, Tanner MA, Adams HR, Parker JL (1995) Release of EDRF and NO in ex vivo perfused aorta: inhibition by in vivo E. coli endotoxemia. Am J Physiol Heart Circ Physiol 268:H955–H961
Parker JL, Adams HR (1993) Selective inhibition of endothelium-dependent vasodilatation capacity by Escherichia coli endotoxemia. Circ Res 72:539–551
Baker CH, Sutton ET (1993) Arteriolar endothelium-dependent vasodilation occurs during endotoxin shock. Am J Physiol Heart Circ Physiol 264:1118–1123
Leclerc J, Pu Q, Corseaux D, Haddad E, Decoene C, Bordet R, Six I, Jude B, Vallet B (2000) A single endotoxin injection in the rabbit causes prolonged blood vessel dysfonction and a procoagulant state. Crit Care Med 28:3672–3678
Tavernier B, Guarrigue D, Boulle C, Vallet B, Adnet P (1998) Myofilament calcium sensitivity is decreased in skinned cardiac fibres of endotoxin-treated rabbits. Cardiovasc Res 38:472–479
Kessler P, Bauersachs J, Busse R, Schini-Kerth VB (1997) Inhibition of inducible NO synthase restores the impaired endothelium-dependent relaxations in isolated arteries exposed to proinflammatory mediators. Arterioscler Thromb Vasc Biol 17:1746–1755
Park JL, Chang KM, Lee SH, Shin SH (1996) Protective effect of nitric oxide in an endotoxin-induced septic shock. Am J Surg 171:340–345
Becker RHA, Weimer G, Linz W (1991) Preservation of endothelial function by ramipril in rabbits on a long-term atherogenic diet. J Cardiovasc Pharmacol 18 (Suppl 2):110–115
Hickey H, Makdissi M, Hyland R, Wilks D, Dusting GJ (1996) Perindopril treatment prevents the loss of endothelial nitric oxide function and development of nitric oxide function and development of neo-intima in rabbits. J Mol Cell Cardiol 28:1985–1994
Van Belle E, Vallet B, Auffray JL, Bauters C, Hamon M, McFadden EP, Lablanche JM, Dupuis B, Bertrand ME (1996) NO synthesis is involved in structural and functional effect of ACE inhibitors in injured arteries. Am J Physiol Heart Circ Physiol 270:H298–H305
DeJonge A, Tholen MJ, Timmermanns PB (1984) Interaction of angiotensin converting enzyme inhibitors with the sympathetic nervous system. Prog Pharmacol 5:25–38
Yang HYT, Erdös EG (1967) Second kinase in human blood plasma. Nature 215:1402–1043
McMurray J, Chopra M (1991) Influence of ACE inhibitors on free radicals and reperfusion injury: pharmacological curiosity or therapeutic hope ? Br J Clin Pharmacol 31:373–379
Monbouli JV, Illiano S, Scott-Burden T, Vanhoutte PM (1992) The potentiation of endothelium-dependent relaxations to bradykinin by angiotensin converting enzyme inhibitors in canine coronary artery involves both endothelium-derived relaxing and contracting factors. Circ Res 71:137–144
Napoleone E, Di Santo A, Camera M, Tremoli E, Lorenzet R (2000) Angiotensin-converting enzyme inhibitors downregulate tissue factor synthesis in monocytes. Circ Res 86:139–143
Boldt J, Papsdorf M, Kumle B, Piper S, Hempelmann G (1998) Influence of angiotensin-converting enzyme inhibitor enalaprilat on endothelial-derived substances in the critically ill. Crit Care Med 26:1663–1670
Gennari R, Alexander JW, Boyce ST, Lilly N, Babcock GF, Cornaggia M (1996) Effects of the angiotensin converting enzyme inhibitor enalapril on bacterial translocation after thermal injury and bacterial challenge. Shock 6:95–100
Kincaid EH, Miller PR, Meredith JW, Chang MC (1998) Enalaprilat improves gut perfusion in critically injured patients. Shock 9:79–83
Hamon M, Vallet B, Bauters C, Wernert N, McFadden EP, Lablanche JM, Dupuis B, Bertrand M (1994) Long-term oral administration of L-arginine reduces intimal thickening and enhances neoendothelium-dependent acetylcholine-induced relaxation after arterial injury. Circulation 90:1357–1362
Carson S (1987) Continuous chromogenic tissue factor assay: comparison to clot-based assays and sensitivity established using pure tissue factor. Thromb Res 47:379–387
Corseaux D, Le Tourneau T, Six I, Ezekowitz MD, McFadden EP, Meurice T, Asseman P, Bauters C, Jude B (1998) Enhanced monocyte tissue factor response after experimental balloon angioplasty in hypercholesterolemic rabbit: inhibition with dietary L-arginine. Circulation 98:1776–1782
Mulder P, Elfertak L, Richard V, Compagnon P, Devaux B, Henry JP, Scalbert E, Desche P, Mace B, Thuillez C (1996) Peripheral artery structure and endothelial function in heart failure: effect of ACE inhibition. Am J Physiol Heart Circ Physiol 271:H469–H477
Frenette PS, Moyna C, Hartwell DW, Lowe JB, Hynes RO, Wagner DD (1998) Platelet-endothelial interactions in inflamed mesenteric venules. Blood 91:1318–1324
Warr T, Rao M, Rapaport S (1990) Disseminated intravascular coagulation in rabbits induced by administration of endotoxin or tissue factor: effect of anti-tissue factor antibodies and measurement of plasma extrinsic pathway inhibitor activity. Blood 75:1481–1489
Gupta RK, Kjeldsen SE, Motley E, Weder AB, Zweifler AJ, Julius S (1991) Platelet function during antihypertensive treatment with quinapril, a novel angiotensin converting enzyme inhibitor. J Cardiovasc Pharmacol 17:13–19
Okrucka A, Pechan J, Kratochvilova H (1998) Effect of the angiotensin-converting enzyme (ACE) inhibitor perindopril on endothelial and platelet functions in essential hypertension. Platelets 9:63–67
Zhuo J, Casley D, Murone C, Mendelsohn FAO (1997) Acute and chronic in vivo inhibition of angiotensin-converting enzyme by perindopril in the endothelium and adventitia of large arteries and organs of the rabbit. J Cardiovasc Pharmacol 29:297–310
Aoki N, Siegfried M, Lefer AM (1989) Anti-EDRF effect of tumor necrosis factor in isolated, perfused cat carotid arteries. Am J Physiol Heart Circ Physiol 256:H1509–H1512
Julou-Schaeffer G, Gray GA, Fleming I, Schott C, Parratt JR, Stoclet JC (1990) Loss of vascular responsiveness induced by endotoxin involves L-arginine pathway. Am J Physiol Heart Circ Physiol 259:H1038–H1043
Rees DD, Monkhouse JE, Cambridge D, Moncada S (1998) Nitric oxide and the haemodynamic profile of endotoxin shock in the conscious mouse. Br J Pharmacol 124:540–546
Adeagbo ASO, Triggle CR (1993) Interactions of nitric oxide synthase inhibitors and dexamethasone with α-adrenoceptor-mediated responses in rat. Br J Pharmacol 109:495–501
Tiffany CW, Burch RM (1989) Bradykinin stimulates tumor necrosis factor and interleukin-1 release from macrophages. FEBS Lett 247:189–192
Daemen MJAP, Lombardi DM, Bosman FT, Schwartz SM (1991) Angiotensin II induces smooth muscle cell proliferation in the normal and injured rat arterial wall. Circ Res 68:450–456
Chopra M, Beswick M, Clapperton M, Dargie HJ, Smith WE, McMurray J (1992) Antioxidant effect of angiotensin-converting enzyme (ACE) inhibitors: free radical and oxidant scavenging are sulfhydryl dependent, but lipid peroxidation is inhibited by both sulfhydryl-and nonsulfhydryl-containing ACE inhibitors. J Cardiovasc Pharmacol 19:330–340
Matsubara T, Ziff M (1986) Increased superoxide anion release from human endothelial cells in response to cytokines. J Immunol 137:3295–3298
Szabó C, Cuzzocrea S, Zinngarelli B, O’Connor M, Salzman AL (1997) Endothelial dysfunction in a rat model of endotoxic shock. Importance of the activation of poly (ADP-ribose) synthetase by peroxynitrite. J Clin Invest 100:723–735
Acknowledgements
The ACE activity measurements were performed in collaboration with Dr. Racadot and Mrs. Michiels, Department of Biochemistry and Perinatal Endocrinology (University Hospital of Lille). Perindopril was kindly provided by Institut de Recherches Internationales Servier, France.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wiel, E., Pu, Q., Leclerc, J. et al. Effects of the angiotensin-converting enzyme inhibitor perindopril on endothelial injury and hemostasis in rabbit endotoxic shock. Intensive Care Med 30, 1652–1659 (2004). https://doi.org/10.1007/s00134-004-2198-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2198-4