Abstract
A surface water isolate of Raoultella sp. having both multidrug- and multimetal-resistant ability was isolated and identified as Raoultella planticola. R. planticola displayed resistance to 15 drugs like ampicillin, amoxicillin/clavulanic acid, aztreonam, erythromycin, imipenem, oxacillin, pefloxacin, penicillin, piperacillin, piperacillin/tazobactam, rifampin, sulbactam/cefoperazone, ticarsillin, ticarsillin/clavulanic acid, vancomycin, and to 11 heavy metals like aluminum, barium, copper, iron, lead, lithium, manganese, nickel, silver, strontium, and tin. The multidrug and multi-metal-resistant R. planticola may remain present in the environment for a long time. Due to a possible health risk of these pathogenic bacteria, a need exists for an accurate assessment of their acquired resistance to multiple drugs and metals.
Similar content being viewed by others
Raoultella planticola was first described in 1981 as Klebsiella planticola (Bagley et al. 1981). In 1983, Klebsiella trevisanii was also reported as a new species (Ferragut et al. 1983). These two species were recognized as K. planticola in 1986, based on phenotypic and genetic similarities (Gavini et al. 1986). Drancourt et al. (2001) analysed the sequence of the 16S rRNA and rpoB genes and renamed K. planticola as R. planticola. R. planticola was originally reported as being isolated from soil and water in the environment (Bagley et al. 1981; Ferragut et al. 1983). Recent studies show that human infections caused by R. planticola have become common (Yokota et al. 2012). Bacteria of the genus Klebsiella are a frequent cause of nosocomial infections. While the medical significance of Klebsiella obtained in the natural environment is far from clear, such habitats are thought to be potential reservoirs for the growth and spread of these bacteria which may colonize animals and humans. R. planticola (previously known as K. planticola), in particular, has often been found, accounting for up to 18 % of all clinical Klebsiella isolates in some studies (Podschun et al. 1998).
Data on the prevalence of multidrug and heavy metal resistant R. planticola in surface waters are necessary to estimate the risk of these surface waters to human. The research into how dispersal of antibiotics and heavy metals affect the bacterial community in nonclinical settings is essential and urgent. Therefore, surface waters have been thought to play an important role in the dissemination and development of antibiotic and heavy metal resistance in these bacteria. The aim of this study was to characterize river isolates of R. planticola resistant to multiple drugs and heavy metals. Identification of the isolate was done by using biochemical tests and 16S rDNA sequencing. After determination of multiple antibiotic and metal resistance profiles, the isolate was further characterized in order to find out the locations of the resistance determinants.
Materials and Methods
Water samples were collected along the river Kızılırmak extending from 39°56′53.25″N. 33°25′04.24″E. 699.5 m to 39°23′53.41″N. 33°25′18.44″E. 775 m of the city Kırıkkale, Turkey. The samples were put into sterile screw capped bottles aseptically, kept in an icebox containing ice packs, and taken immediately to the laboratory. A quantity of 1 mL of water from each of the collected samples was dissolved in 9 mL sterile distilled water and serial dilutions were made. Each dilution was plated on Luria–Bertani (LB) agar plates by the standard pour plate method. Plates were incubated at 30°C for 3 days and colonies differing in morphological characteristics were selected. After the growth of different microorganisms on the plate, each bacterial colony on the basis of its morphological characteristics was picked up and further purified by repeated streaking on nutrient agar plates and identified with gram staining. Each bacterial culture was then inoculated in nutrient broth, incubated and glycerol stocks were made and frozen at −70°C. For isolation and purification, strains were routinely grown in LB medium at 30°C. The Analytical Profile Index (API 20E) strep micromethod for the primary identification of isolates, using 8 conventional biochemical tests and 12 carbohydrate assimilation tests, was performed as described by the manufacturer (Bio Merieux, France) and the results were analyzed using Apiweb, version 1.2.1. R. planticola strain ATCC 33531 was used as a positive control and Pseudomonas aeruginosa ATCC 9027 was used as a negative control. Confirmation of the taxonomical status of the selected strain was done by molecular methods. Genomic DNA was isolated and analyzed from R. planticola by the method of Chen and Kuo (1993). Bacterial 16S rDNA was amplified by using the universal bacterial 16S rDNA primers, F (5′-AGAGTT TGATCCTGGCTCAG-3′) and R (5′-GGTGTTTGATTGTTACGACTT-3′). PCR was performed with a 50 μL reaction mixture containing 1 μL (10 ng) of DNA extract as a template, each primer at a concentration of 5, 25 mM·MgCl2 and dNTPs at a concentration of 2 mM, as well as 1.5 U of Taq polymerase and buffer used as recommended by the manufacturer (Fermentas, Germany). After the initial denaturation for 5 min at 94°C, there were 35 cycles consisting of denaturation at 94°C for 1 min, annealing at 55°C for 1 min, extension at 72°C for 1 min, and final extension at 72°C for 5 min. PCR was carried out in a gene Piko Thermal Cycler (Thermo Scientific, USA). The obtained PCR products were purified, using the GeneJET™ PCR Purification Kit (Fermentas, Germany), according to the instructions of the manufacturer, and sequenced. The PCR product was sequenced by 3,730 × 1 DNA synthesizer (Applied Biosystems, USA). The two 16S rRNA sequences were aligned and compared with other 16S rRNA genes in the GenBank by using the NCBI basic local alignment search tools BLASTn program (Benson and Karsch-Mizrachi 2000). A distance matrix was generated using the Jukes-Cantor corrected distance model. The phylogenetic trees were created using Weighbor (Weighted Neighbor Joining: A Likelihood-Based Approach to Distance-Based Phylogeny Reconstruction). The 16S rRNA gene sequences have been deposited to GenBank using the BankIt submission tool, and have been assigned with NCBI accession numbers.
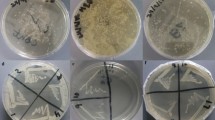
To determine multi-metal resistance, NA plates supplemented with heavy metals were used (Mergeay and Nies 1985). The concentrations of metals used in this study were observed earlier (Ozer et al. 2013; Aktan et al. 2013). R. planticola isolate was inoculated in radial streaks on NA media supplemented with each heavy metal salt AlCl36H2O, LiCl, BaCl22H2O, CrN3O99H2O, MnSO4H2O, Pb(NO3)2, Co(NO3)26H2O, FeCl36H2O, Hg(NO3)2H2O, CuSO45H2O, SnCl22H2O, NiSO46H2O, ZnSO47H2O, K(SbO)C4H4O60.5H2O, Cd(NO3)24H2O, Ag(NO3), and Sr(NO3)2 in concentrations of 300, 5,000, 2,700, 1,050, 1,000, 1,200, 750, 450, 195, 450, 160, 395, 825, 1,400, 750, 8, and 2,000 μg mL−1, respectively. For the evaluation of antibiotic tolerance, overnight-grown cultures of R. planticola isolate were used for antibiotic resistance or susceptibility. R. planticola strain ATCC 33531 was used as a reference strain. The disk diffusion method was used to check the resistance or sensitivity of bacterial strains towards given antibiotics (Bauer and Kirby 1966). Antibiotic disks used in this study were amikacin (30 μg mL−1), amoxicillin/CA (30 μg mL−1), ampicillin (10 μg mL−1), aztreonam (30 μg mL−1), bacitracin (10 μg mL−1), cefepime (5 μg mL−1), ceftazidime (30 μg mL−1), ciprofloxacin (5 μg mL−1), chloramphenicol (30 μg mL−1), erythromycin (15 μg mL−1), gentamicine (10 μg mL−1), imipenem (10 μg mL−1), netilmicin (30 μg mL−1), oxacillin (1 μg mL−1), pefloxacin (5 μg mL−1), penicillin (10 μg mL−1), piperacillin (100 μg mL−1), piperacillin/tazobactam (100/10 μg mL−1), rifampin (10 μg mL−1), sulbactam/CFP (105 μg mL−1), tetracycline (30 μg mL−1), ticarcillin (75 μg mL−1), ticarcillin/CA (75/10 μg mL−1), trimeth-sulfa (25 μg mL−1), tobramycin (10 μg mL−1), and vancomycin (30 μg mL−1).
The R. planticola isolate was analyzed for its plasmid content according to the procedures of Birnboim and Doly (1979) and of Kado and Liu (1981). The approximate molecular weight of each plasmid was consequently obtained by extrapolation on graphical plots of the molecular weight of marker Agrobacterium tumefaciens C58C1 against the distance traveled by the respective band. Total DNA was isolated from all selected R. planticola strains using classical protocol for isolation (Chen and Kuo 1993). Plasmid curing was carried out in order to determine the location of the drug resistance marker(s). The curing of the resistant plasmids was done using a sub-inhibitory concentration of 10 μg mL−1 ethidium bromide as described by Edward Raja and Selvam (2009). The direct transfer of plasmid DNA from R. planticola strain to Escherichia coli DH5α was attempted by liquid and solid mating assays, as previously described (Granier et al. 2003).
Results and Discussion
Bacterial isolates were identified using the traditional morphological and biochemical tests. During this study, gram-negative, aerobic, non-motile, encapsulated rod bacteria were screened as presumptive Raoultella spp. Isolates were positive for indole production, histamine assimilation and growth at 10°C, and did not utilize ornithine or D-melezitose, and were identified as R. planticola. Biochemical identification was confirmed by the analysis of the 16S rDNA sequences. Based on the phylogenetic analysis, the isolate was affiliated with R. planticola with an accession number of AF129443. The isolate showed 99 % homology with R. ornithinolytica with an accession number of U78182 (Fig. 1). However, due to the negative ornithine biochemical test, the isolate was identified as R. planticola. Raoultella species are gram-negative aerobic bacilli belonging to the Enterobacteriaceae family that are closely related to Klebsiella spp. (Morais et al. 2009). R. planticola was originally reported as being isolated from soil and water in the environment (Bagley et al. 1981; Ferragut et al. 1983). In more recent studies, R. planticola has been found in humans. Sources of clinical isolates of R. planticola have included sputum, urine, feces, wounds and bile (Podschun et al. 1998). This study also reports the isolation and the identification of R. planticola from a river. Microbial aquatic ecosystems, mainly those integrating the urban water cycle, represent important vehicles for the dissemination of human-associated microorganisms and they may act as a reservoir for the dissemination of resistance genes to other species, including potential pathogens. The ability of R. planticola, particularly antibiotic-resistant strains, to survive for long periods in diverse environments has received considerable attention by public health authorities. Since the aquatic environment is implicated as the reservoir for these microorganisms, and consequently responsible for their transmission in humans, it is obvious that detailed studies on the pathogenic potential of the environmental strains will certainly contribute to understanding the virulence properties of these bacteria and to establish the importance of these significant pathogens of aquatic systems.
Bacteria that are resistant to antibiotics have been found in the aquatic environment (Ozer et al. 2013; Aktan et al. 2013) and in soil (Schmidt and Römbke 2008). Our study also confirmed the widespread emergence of multidrug resistance in the R. planticola surface water isolate. R. planticola displayed resistance to 15 drugs like ampicillin, amoxicillin/clavulanic acid, aztreonam, erythromycin, imipenem, oxacillin, pefloxacin, penicillin, piperacillin, piperacillin/tazobactam, rifampin, sulbactam/cefoperazone, ticarsillin, ticarsillin/clavulanic acid and vancomycin. The multidrug-resistant river isolate of R. planticola was resistant to β-lactams, cephalosporins, quinolones, rifamycins, macrolides and glycopeptides tested. Such a β-lactam resistance phenotype suggests that the river isolate of R. planticola produces β-lactamases as isolates of Klebsiella species. Clinical isolates of Klebsiella and Raoultella are easily confused, especially since the species of these genera display identical β-lactam resistance patterns. In this study, the river isolate of R. planticola showed resistance to cephalosporins including aztreonam and sulbactam/cefoperazone. Indeed, the species are resistant to amino- and carboxy-penicillins but are susceptible to these molecules when they are combined with clavulanate (Stock and Wiedemann 2001). However, this was not in agreement with what we found in our study. The river isolate of R. planticola was also resistant to amoxicillin/clavulanic acid, piperacillin/tazobactam, sulbactam/cefoperazone, and ticarsillin/clavulanic acid combinations. Although the inhibitor-resistant β-lactamases are not extended to the spectrum of β-lactamases (ESBLs), they are often discussed with ESBLs because they are also derivatives of the classical TEM- or SHV-type enzymes. These enzymes are at first given the designation IRT for inhibitor-resistant TEM β-lactamase; however, all have subsequently been renamed with numerical TEM designations. There are at least 19 distinct inhibitor-resistant TEM β-lactamases. Inhibitor-resistant TEM β-lactamases have been found mainly in clinical isolates of E. coli, but also some strains of Klebsiella pneumoniae, Klebsiella oxytoca, P. mirabilis, and Citrobacter freundii. Clavulanate, sulbactam, and tazobactam are potent suicide inhibitors of serine β-lactamases, most of which belong to Ambler class A or C (Ambler 1980). These inhibitors block β-lactamases through the initial formation of stable acylated compound enzyme intermediates. Therefore, several combinations of these inhibitors and β-lactams, such as clavulanate/amoxicillin, sulbactam/ampicillin, sulbactam/cefoperazone, and tazobactam/piperacillin, have been developed for clinical use, and they have opened a new era in the chemotherapy of infectious diseases caused by gram-negative bacteria producing β-lactamases. However, several clinical isolates demonstrating resistance to these combinations have emerged (Bradford 2001), and these were found to produce mainly TEM-related β-lactamases such as TEM-30 to TEM-41, which have been classified into the functional group 2br by Bush et al. (1995). Our results were in agreement with those findings. We also found that the isolate did not show any resistance to aminoglycosides, sulfonamides, polypeptides, and polyketides tested.
The main risk for public health is that resistance genes are transferred from environmental bacteria to human pathogens. R. planticola can be exposed to antibiotics at their source and in the environment; therefore, waters with increased R. planticola may also contain higher levels of antibiotic-resistant bacteria. If bacteria that cause illness become resistant to antibiotics, then treatment of the illness becomes more difficult and treatment options more limited. Because the river Kızılırmak serves as an important water resource for the region, antibiotic-resistant bacteria in the river waters may pose a risk to human health for those who use these resources. Microorganisms resistant to antibiotics and tolerant to metals appear as the result of exposure to metal contaminated environments which cause coincidental co-selection of resistance factors for antibiotics and heavy metals. Heavy metal tolerance in the environment may contribute to the maintenance of antibiotic resistance genes by increasing the selective pressure of the environment. The river isolate of R. planticola was also tested for its resistance to the heavy metals such as Al2+, Pb2+, Li2+, Ba2+, Cr3+, Mn2+, Ag2+, Co2+, Fe2+, Hg2+, Cu2+, Sn2+, Ni2+, Zn2+, Sb2+, Cd2+, and Sr2+ at different concentrations from 8 to 5,000 mg L−1. The R. planticola isolates were found to be resistant to multiple metals. Resistance to multiple antibiotics coincided with a general tendency to be resistant to multiple heavy metals. R. planticola was found to be resistant to the heavy metals aluminum, barium, copper, iron, lead, lithium, manganese, nickel, silver, strontium, and tin. Although resistance phenotype determination is of paramount importance for clinical isolates, the tolerance to antimicrobial substances, even when these are below the resistance/susceptibility breakpoints, may represent a selective advantage for the organism in the environment. It has been hypothesized that in the environment, bacteria may face different types of chemical aggressions, capable of selecting positively or negatively for antibiotic tolerance. Presumably, bacteria thriving in wastewater, where antibiotic residues or heavy metals may be discharged, face different challenges than those surviving in a drinking water supply system, where the organic content and chemical contamination is absent or at trace levels. Such environmental pressures may also be responsible for the prevalence of specific groups of organisms that are able to deal with the imposed environmental conditions (Faria et al. 2009). The combined resistance to heavy metals was also reported by Enne et al. (2001), Ozer et al. (2013), and Aktan et al. (2013). Many have speculated and have even shown that a correlation exists between metal tolerance and antibiotic resistance in bacteria because of the likelihood that resistance genes to both antibiotics and heavy metals may be located closely together on the same plasmid in bacteria, and are thus more likely to be transferred together in the environment. However, microorganisms may develop resis-tance at their source, where antibiotic concentrations might be higher, or by acquisition of an antibiotic-resistance gene that was carried on a genetic element and transferred to that organ-ism via exposure to a different chemical.
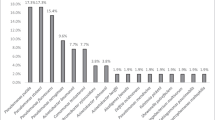
In order to determine the resistance determinants, the river isolate of R. planticola was screened for the presence of plasmid DNA. Our study showed that R. planticola harbored a high molecular weight plasmid ca. 127.5 kb (Fig. 2). The high molecular weight of ca. 127.5 kb plasmid cured derivative of R. planticola was found to be still resistant to β-lactams, while resistance to erythromycin, rifampin, and vancomycin was lost. This finding indicated that resistance to β-lactams of this isolate was chromosome-encoded while the resistance to erythromycin, rifampin, and vancomycin was plasmid-encoded. In order to confirm these findings, 127.5 kb plasmid DNA of R. planticola was transformed into erythromycin, rifampin, and vancomycin sensitive E. coli DH5α by the calcium chloride method as per standard molecular biology protocol. Although, the transformant E. coli DH5α isolates were able to grow on LB medium containing erythromycin, rifampin, and vancomycin, they were not able to grow on LB medium containing β-lactams. The transformation frequency of E. coli DH5α was calculated to be approximately 2.7 × 10−5 per recipient. The transformants were also checked for the presence of ca. 127.5 kb plasmid DNA, and the gel patterns showed that transformant strains contained a single plasmid with mobility identical to that of the donor strain’s plasmid (Fig. 2). β-Lactamases are classified into four classes based on substrate affinity and amino acid sequence. Two of these classes are much more common than the others; classes A and C. Class A includes various plasmid mediated β-lactamases (TEM-1, SHV-1), the plasmid-mediated extended-spectrum β-lactamases derived from TEM or SHV, and some chromosomally encoded β-lactamases, such as that produced by K. pneumoniae (Arakawa et al. 1986). Our findings also showed chromosomally encoded β-lactamases by R. planticola.
Plasmid profiles of R. planticola (lane 1), transformant E. coli DH5α (lane 2), and cured derivative of R. planticola (lane 3), Agrobacterium tumefaciens C58C1 marker (M), chromosomal DNA (chr). M, A. tumefaciens C58C1 marker (the DNA bands and their corresponding molecular weights from top to down; 127.5 kb, chromosomal DNA, and 13.9 kb, respectively); Lanes 1 and 2 contain 127.5 kb plasmid DNA and chromosomal DNA; Lane 3, contains only chromosomal DNA
The widespread emergence of antibiotic resistance, particularly multidrug resistance, among bacterial pathogens has become one of the most serious challenges in clinical therapy. Acquisition of resistance genes through horizontal transfer has been found to be ubiquitous in clinical pathogens. Environmental bacteria have been shown to be a reservoir of antibiotic resistance genes and a potential source of novel resistance genes in clinical pathogens (Dantas et al. 2008). Horizontal transfer of genes between bacterial strains could be facilitated by mobile genetic elements, such as plasmids, transposons, bacteriophages, integrons, insertion elements (IS), and genomic islands (Frost et al. 2005). Some elements, including class I integrons, conjugative plasmids, and transposons, are frequently linked to antibiotic resistance as they harbor rather diverse resistance genes and possibly promote the distribution of these genes in phylogenetically diverse bacteria. In light of the potential health risk, many studies have focused on antibiotic and heavy metal-resistant bacteria recovered from various ecosystems. Environments that contain antibiotic and heavy metal residues are particularly worrisome because these antimicrobials could exert selective pressure and might contribute to the appearance of resistant bacteria. Hospital sewage is considered the major source of antibiotics in aquatic environments, followed by municipal, agricultural, and aquacultural wastewater, which have also been shown to be important sources of these compounds and resistant bacteria. The water quality is affected by human activities around the areas, which include industrial processes, health care centers, farms, slaughterhouses, mines and homes. Thus, the main source of R. planticola in the river may be wastewater discharges from effluent as well as domestic sewage around the catchment areas. The water-borne and food-borne spread of this pathogen is possibly due to drinking water contamination, recreational activities, and fisheries. Since the aquatic environment is implicated as the reservoir for microorganisms, and consequently responsible for their transmission in humans, it is obvious that detailed studies on the pathogenic potential of the environmental strains will certainly contribute to understanding the virulence properties of these bacteria and to establish the importance of these pathogens of aquatic systems. Importantly, once in the environment, bacteria of different origin come into physical contact and may exchange resistance genes with the endogenous bacterial populations. Despite the generally believed negative impact of acquired resistance on fitness of the bacteria, the multidrug and multi-metal-resistant R. planticola may remain present in the environment for a long time and pose a health risk. Therefore, a need exists for an accurate assessment of acquired resistance in these pathogenic bacteria.
References
Aktan Y, Tan S, Icgen B (2013) Characterization of lead-resistant river isolate Enterococcus faecalis and assessment of its multiple metal and antibiotic resistance. Environ Monit Assess 185:5285–5293
Ambler RP (1980) The structure of β-lactamases. Phil Trans R Soc London Ser B 289:321–331
Arakawa Y, Ohta M, Kido N, Fujii Y, Komatsu T, Kato N (1986) Close evolutionary relationship between the chromosomally encoded β-lactamase gene of K. pneumoniae and the TEM β-lactamase gene mediated by R plasmids. FEBS Lett 207:69–74
Bagley ST, Seidler RJ, Brenner DJ (1981) K. planticola sp. nov.: a new species of Enterobacteriaceae found primarily in nonclinical environments. Curr Microbiol 6:105–109
Bauer AW, Kirby WWM (1966) Antibiotic susceptibility tests by standard single disc method. Am J Clin Pathol 45:493–496
Benson DA, Karsch-Mizrachi I (2000) GenBank. Nucleic Acids Res 28:15–18
Birnboim HC, Doly J (1979) A rapid alkaline extraction procedure for screening recombinant plasmid DNA. Nucleic Acids Res 7:1513–1523
Bradford PA (2001) Extended-spectrum β-lactamases in the 21st century: characterization, epidemiology, and detection of this important resistance threat. Clin Microbiol Rev 48:933–951
Bush K, Jacoby GA, Medeiros AA (1995) A functional classification scheme for β-lactamases and its correlation with molecular structure. Antimicrob Agents Chemother 39:1211–1233
Chen WP, Kuo TT (1993) A simple and rapid method for the preparation of gram negative bacterial genomic DNA. Nucleic Acid Res 21:2260
Dantas G, Sommer MOA, Oluwasegun RD, Church GM (2008) Bacteria subsisting on antibiotics. Science 320:100–103
Drancourt M, Bollet C, Carta A, Rousselier P (2001) Phylogenetic analyses of Klebsiella species delineate Klebsiella and Raoultella gen. nov., with description of R. ornithinolytica comb. nov., R. terrigena comb. nov. and R. planticola comb. nov. Int J Syst Evol Microbiol 51:925–932
Edward Raja C, Selvam GS (2009) Plasmid profile and curing analysis of P. aeruginosa as metal resistant. Int J Environ Sci Tech 6:259–266
Enne VI, Livermore DM, Stephens P, Hall L (2001) Persistence of sulphonamide resistance in E. coli in the UK despite national prescribing restriction. Lancet 357:1325–1328
Faria C, Vaz-Moreira I, Serapicos E, Nunes OC, Manaia CM (2009) Antibiotic resistance in coagulase negative staphylococci isolated from wastewater and drinking water. Sci Total Environ 407:3876–3882
Ferragut C, Izard D, Gavini F, Kersters K, De Ley J, Leclerc H (1983) Klebsiella trevisanii: a new species from water and soil. Int J Syst Bacteriol 33:133–142
Frost LS, Leplae R, Summers AO, Toussaint A (2005) Mobile genetic elements: the agents of open source evolution. Nat Rev Microbiol 3:722–732
Gavini F, Izard D, Grimont PAD, Beji A, Ageron E, Leclerc H (1986) Priority of K. planticola Bagley, Seidler, and Brenner 1982 over K. trevisanii Ferragut, Izard, Gavini, Kersters, DeLey, and Leclerc 1983. Int J Syst Bacteriol 36:486–488
Granier SA, Plaisance L, Leflon-Guibout V, Lagier E, Morand S, Goldstein F, Nicolas-Chanoine MH (2003) Recognition of two genetic groups in K. oxytoca taxon on the basis of the chromosomal β-lactamase and housekeeping gene sequences as well as ERIC-1R PCR typing. Int J Syst Evol Microbiol 53:661–668
Kado CI, Liu ST (1981) Rapid procedure for detection and isolation of large and small plasmids. J Bacteriol 145:1365–1373
Mergeay M, Nies D (1985) Alcaligenes eutrophus CH34 is a facultative chemolithotroph with plasmid-bound resistance to heavy metals. J Bacteriol 162:328–334
Morais VP, Daporta MT, Bao AF, Campello MG, Andres GQ (2009) Enteric fever-like syndrome caused by Raoultella ornithinolytica (K. ornithinolytica). J Clin Microbiol 47:868–869
Ozer G, Ergene A, Icgen B (2013) Biochemical and molecular characterization of strontium resistant environmental isolates of P. fluorescens and S. paucimobilis. Geomicrobiol J 30:381–390
Podschun R, Acktun H, Okpara J, Linderkamp O, Ullmann U, Borneff-Lipp M (1998) Isolation of K. planticola from newborns in a neonatal ward. J Clin Microbiol 36:2331–2332
Schmidt H, Römbke J (2008) The ecotoxicological effects of pharmaceuticals (antibiotics and antiparasiticides) in the terrestrial environment—a review. In: Kümmerer K (ed) Pharmaceuticals in the environment, sources, fate effects and risk. Springer, Berlin
Stock I, Wiedemann B (2001) Natural antibiotic susceptibility of K. pneumoniae, K. oxytoca, K. planticola, K. ornithinolytica and K. terrigena strains. J Med Microbiol 50:396–406
Yokota K, Gomi H, Miura Y, Sugano K, Morisawa Y (2012) Cholangitis with septic shock caused by R. planticola. J Med Microbiol 61:446–449
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koc, S., Kabatas, B. & Icgen, B. Multidrug and Heavy Metal-Resistant Raoultella planticola Isolated from Surface Water. Bull Environ Contam Toxicol 91, 177–183 (2013). https://doi.org/10.1007/s00128-013-1031-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00128-013-1031-6