Abstract
Background
Identifying predictors of suicidal ideation (SI) is important to inform suicide prevention efforts, particularly among high-risk populations like military veterans. Although many studies have examined the contribution of psychopathology to veterans’ SI, fewer studies have examined whether experiencing good psychosocial well-being with regard to multiple aspects of life can protect veterans from SI or evaluated whether SI risk prediction can be enhanced by considering change in life circumstances along with static factors.
Methods
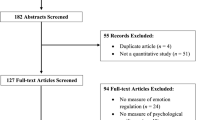
The study drew from a longitudinal population-based sample of 7141 U.S. veterans assessed throughout the first three years after leaving military service. Machine learning methods (cross-validated random forests) were applied to examine the predictive utility of static and change-based well-being indicators to veterans’ SI, as compared to psychopathology predictors.
Results
Although psychopathology models performed better, the full set of well-being predictors demonstrated acceptable discrimination in predicting new-onset SI and accounted for approximately two-thirds of cases of SI in the top strata (quintile) of predicted risk. Greater engagement in health promoting behavior and social well-being were most important in predicting reduced SI risk, with several change-based predictors of SI identified but stronger associations observed for static as compared to change-based indicator sets as a whole.
Conclusions
Findings support the value of considering veterans’ broader well-being in identifying individuals at risk for suicidal ideation and suggest the possibility that well-being promotion efforts may be useful in reducing suicide risk. Findings also highlight the need for additional attention to change-based predictors to better understand their potential value in identifying individuals at risk for SI.


Similar content being viewed by others
Data availability
These data are owned by VA. VA supports efforts to provide limited, restricted access to research data under written agreements that are consistent with commitments made to protecting subjects’ privacy and confidentiality and subject to resource availability. Contact the corresponding author for further information.
References
Hoffmire CA, Monteith LL, Forster JE, Bernhard PA, Blosnich JR, Vogt D, Maguen S, Smith AA, Schneiderman AI (2021) Gender differences in lifetime prevalence and onset timing of suicidal ideation and suicide attempt among post-9/11 veterans and nonveterans. Med Care 59:S84–S91. https://doi.org/10.1097/MLR.0000000000001431
Sokol Y, Gromatsky M, Edwards ER, Greene AL, Geraci JC, Harris RE, Goodman M (2021) The deadly gap: understanding suicide among veterans transitioning out of the military. Psychiatry Res 300:113875. https://doi.org/10.1016/j.psychres.2021.113875
Jobes DA, Joiner TE (2019) Reflections on suicidal ideation. Crisis 40(4):227–230. https://doi.org/10.1027/0227-5910/a000615
Kleiman EM (2020) Suicidal thinking as a valuable clinical endpoint. EClin Med 23:100399. https://doi.org/10.1016/j.eclinm.2020.100399
Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, Nock MK (2017) Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol Bull 143(2):187–232. https://doi.org/10.1037/bul0000084
Kline A, Ciccone DS, Falca-Dodson M, Black CM, Losonczy M (2011) Suicidal ideation among National Guard troops deployed to Iraq: the association with postdeployment readjustment problems. J Nervous Mental Dis 199(12):914–920. https://doi.org/10.1097/NMD.0b013e3182392917
Nock MK, Ramirez F, Rankin O (2019) Advancing our understanding of the who, when, and why of suicide risk. JAMA Psychiat 76(1):11–12. https://doi.org/10.1001/jamapsychiatry.2018.3164
Carroll D, Kearney LK, Miller MA (2020) Addressing suicide in the veteran population: engaging a public health approach. Front Psychiatry 11:569069. https://doi.org/10.3389/fpsyt.2020.569069
Schafer KM, Duffy M, Kennedy G, Stentz L, Leon J, Herrerias G, Fulcher S, Joiner TE (2022) Suicidal ideation, suicide attempts, and suicide death among Veterans and service members: a comprehensive meta-analysis of risk factors. Mil Psychol 34(2):129–146. https://doi.org/10.1080/08995605.2021.1976544
Haller M, Angkaw A, Hendricks BA, Norman SB (2015) Does reintegration stress contribute to suicidal ideation among returning veterans seeking PTSD treatment? Suicide Life-Threatening Behav 46(2):160–171. https://doi.org/10.1111/sltb.12181
Elbogen EB, Molloy K, Wagner HR, Kimbrel NA, Beckham JC, Van Male L, Leinbach J, Bradford DW (2020) Psychosocial protective factors and suicidal ideation: results from a national longitudinal study of veterans. J Affect Disord 260:703–709. https://doi.org/10.1016/j.jad.2019.09.062
Borowski S, Rosellini AJ, Street AE, Gradus JL, Vogt D (2022) The first year after military service: predictors of U.S. veterans’ suicidal ideation. Am J Preventive Med. https://doi.org/10.1016/j.amepre.2022.03.017
Hoffmire CA, Borowski S, Vogt D (in press) Contribution of veterans’ initial post separation vocational, financial, and social experiences to their suicidal ideation trajectories following military service. Suicide Life-Threatening Behav. doi:https://doi.org/10.1111/sltb.12955
Pisani AR, Murrie DC, Silverman MM (2016) Reformulating suicide risk formation: from prediction to prevention. Acad Psychiatry 40:623–629. https://doi.org/10.1007/s40596-015-0434-6
Turner BJ, Kleiman EM, Nock MK (2018) Psychopathology and risk of suicide. In: Butcher JN, Hooley JM (eds) APA handbook of psychopathology: psychopathology: understanding, assessing, and treating adult mental disorders. American Psychological Association, pp 609–630. https://doi.org/10.1037/0000064-024
Vogt D, Perkins DF, Copeland LA, Finley EP, Jamieson CS, Booth B, Lederer S, Gilman C (2018) The Veterans Metrics Initiative study of U.S. veterans’ experiences during their transition from military service. BMJ Open 8(6):e020734. https://doi.org/10.1136/bmjopen-2017-020734
Dillman DA, Smyth JD, Christian LM (2011) Internet, phone, mail, and mixed-mode surveys: the tailored design method, 3rd edn. Wiley, Hoboken
Kroenke K, Spitzer RL, Williams JBW (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16:606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
U.S. Department of Veterans Affairs (2018) VA research on suicide prevention
Wisco BE, Marx BP, Wolf EJ, Miller MW, Southwick SM, Pietrzak RH (2014) Posttraumatic stress disorder in the U.S. veteran population: results from the National Health and Resilience in Veterans study. J Clin Psychiatry 75(12):1338–1346. https://doi.org/10.4088/JCP.14m09328
Na PJ, Yaramala SR, Kim JA, Kim H, Goes FS, Zandi PP, Vande Voort LJ, Sutor B, Croarkin P, Bobo WV (2018) The PHQ-9 Item 9 based screening for suicide risk: a validation study of the Patient Health Questionnaire (PHQ)−9 Item 9 with the Columbia Suicide Severity Rating Scale (C-SSRS). J Affect Disord 232:34–40. https://doi.org/10.1016/j.jad.2018.02.045
Corson K, Denneson LM, Bair MJ, Helmer DA, Goulet JL, Dobscha SK (2013) Prevalence and correlates of suicidal ideation among Operation Enduring Freedom and Operation Iraqi Freedom veterans. J Affect Disord 149(1–3):291–298. https://doi.org/10.1016/j.jad.2013.01.043
Vogt D, Taverna EC, Nillni YI, Booth B, Perkins DF, Copeland LA, Finley EP, Tyrell FA, Gilman CL (2019) Development and validation of a tool to assess military veterans’ status, functioning, and satisfaction with key aspects of their lives. Appl Psychol 11(2):328–349. https://doi.org/10.1111/aphw.12161
Kroenke K, Spitzer RL, Williams JB, Löwe B (2009) An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics 50(6):613–621. https://doi.org/10.1176/appi.psy.50.6.613
Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR (2007) AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res 31(7):1208–1217. https://doi.org/10.1111/j.1530-0277.2007.00403.x
Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, Kaloupek DG, Schnurr PP, Kaiser AP, Leyva YE, Tiet QQ (2016) The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. J Gen Intern Med 31(10):1206–1211. https://doi.org/10.1007/s11606-016-3703-5
Price M, Szafranski DD, van Stolk-Cooke K, Gros DF (2016) Investigation of abbreviated 4 and 8 item versions of the PTSD checklist 5. Psychiatry Res 239:124–130. https://doi.org/10.1016/j.psychres.2016.03.014
Stekhoven DJ, Bühlmann P (2012) MissForest–non-parametric missing value imputation for mixed-type data. Bioinformatics 28(1):112–118. https://doi.org/10.1093/bioinformatics/btr597
Webb CA, Cohen ZD, Beard C, Forgeard M, Peckham AD, Björgvinsson T (2020) Personalized prognostic prediction of treatment outcome for depressed patients in a naturalistic psychiatric hospital setting: a comparison of machine learning approaches. J Consult Clin Psychol 88(1):25–38. https://doi.org/10.1037/ccp0000451
Schwartz B, Cohen ZD, Rubel JA, Zimmermann D, Wittmann WW, Lutz W (2021) Personalized treatment selection in routine care: integrating machine learning and statistical algorithms to recommend cognitive behavioral or psychodynamic therapy. Psychother Res 31(1):33–51. https://doi.org/10.1080/10503307.2020.1769219
Hothorn T, Hornik K, Zeileis A (2006) Unbiased recursive partitioning: a conditional inference framework. J Comput Graph Stat 15(3):651–674. https://doi.org/10.1198/106186006X133933
R Core Team (2020) R: a language and environment for statistical computing. Version 1.3.1093. R Foundation for Statistical Computing. Kuhn, M., (2020). Caret: Classification and regression training. R package version 6.0–86.
Kuhn M, (2020) Caret: Classification and regression training. R package version 6.0-86.
Strobl C, Boulesteix A-L, Zeileis A, Hothorn T (2007) Bias in random forest variable importance measures: illustrations, sources and a solution. BMC Bioinform 8(1):25–25. https://doi.org/10.1186/1471-2105-8-25
Therneau T (2021) A package for survival analysis in R_. R package version 3.2-11, https://CRAN.R-project.org/package=survival
Ravindran C, Morley SW, Stephens BM, Stanley IH, Reger MA (2020) Association of suicide risk with transition to civilian life among US military service members. JAMA Network Open 3(9):e2016261. https://doi.org/10.1001/jamanetworkopen.2020.16261
Na PJ, De Angelis F, Nichter B, Wendt FR, Krystal JH, Southwick SM, Levey DF, Gelernter J, Polimanti R, Pietrzak RH (2021) Psychosocial moderators of polygenic risk for suicidal ideation: results from a 7-year population-based, prospective cohort study of U.S. veterans. Mol Psychiatry 27:1068–1074. https://doi.org/10.1038/s41380-021-01352-2
Warner CH, Appenzeller GN, Grieger T, Blelnkiy S, Breitbach J, Parker J, Warner CM, Hoge C (2011) Importance of anonymity to encourage honest reporting in mental health screening after combat deployment. Arch Gen Psychiatry 68(10):1065–1071. https://doi.org/10.1001/archgenpsychiatry.2011.112
U.S. Department of Health and Human Services (2001) Mental Health: culture, race, and ethnicity—a supplement to mental health: a report of the surgeon general. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services
Crum-Cianflone NF, Powell TM, Leardmann CA, Russell DW, Boyko EJ (2016) Mental health and comorbidities in U.S. military members. Military Med 181(6):537–545. https://doi.org/10.7205/MILMED-D-15-00187
Vogt D (2011) Mental health-related beliefs as a barrier to service use for military personnel and veterans: a review. Psychiatr Serv 62(2):135–142. https://doi.org/10.1176/ps.62.2.pss6202_0135
Posner K, Brown G, Stanley B, Brent D, Yershova K, Oquendo M, Currier GW, Melvin GA, Greenhill L, Shen S, Mann J (2011) The Columbia-Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry 168(12):1266–1277. https://doi.org/10.1176/appi.ajp.2011.10111704
Horowitz LM, Bridge JA, Teach SJ, Ballard E, Klima J, Rosenstein DL, Wharff EA, Ginnis K, Cannon E, Joshi P, Pao M (2012) Ask Suicide-Screening Questions (ASQ): a brief instrument for the pediatric emergency department. Arch Pediatr Adolesc Med 166(12):1170–1176. https://doi.org/10.1001/archpediatrics.2012.1276
Acknowledgements
This research was funded by a grant from Veterans Health Administration Health Services Research and Development Service (PI: Vogt), and drew from data collected as part of a previously funded project managed by the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc. (HJF); and collaboratively sponsored by the Bob Woodruff Foundation, Health Net Federal Services, The Heinz Endowments, HJF, Lockheed Martin Corporation, May and Stanley Smith Charitable Trust, National Endowment for the Humanities, Northrop Grumman, Philip and Marge Odeen, Prudential, Robert R. McCormick Foundation, Rumsfeld Foundation, Schultz Family Foundation, Walmart Foundation, Wounded Warrior Project, Inc., and the Veterans Health Administration Health Services Research and Development Service (PI: Vogt). The views expressed are those of the authors and do not necessarily represent the views or policy of the Department of Veterans Affairs or the United States Government.
Author information
Authors and Affiliations
Contributions
DV: conceptualization, methodology, investigation, resources, writing—review & editing, supervision, project administration, funding acquisition. AJR: conceptualization, methodology, software, validation, formal analysis, resources, data curation, writing—review & editing, visualization; SB: conceptualization, methodology, formal analysis, resources, data curation, writing—original draft, visualization, project administration; AES: conceptualization, methodology, writing—review & editing; RWO: conceptualization, writing—review & editing; NT: conceptualization, writing—review & editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical approval
This study was approved by the local Institutional Review Board.
Patient consent
All participants provided informed consent to participate.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vogt, D., Rosellini, A.J., Borowski, S. et al. How well can U.S. military veterans’ suicidal ideation be predicted from static and change-based indicators of their psychosocial well-being as they adapt to civilian life?. Soc Psychiatry Psychiatr Epidemiol 59, 261–271 (2024). https://doi.org/10.1007/s00127-023-02511-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-023-02511-2