Abstract
Purpose
Individuals with bipolar disorder (BD) may have an increased risk of exposure to prescription opioids. However, it is still unknown whether such risk also occurs in their offspring. This study aimed to investigate the risk of exposure to prescription opioid use and related medical conditions in the offspring of parents with BD.
Methods
This study used the Taiwan National Health Research Database and included offspring who had any parent with a diagnosis of BD. The matched-control cohort was randomly identified from the offspring of parents without any major psychiatric disorders (MPD). We identified data pertaining to opioid prescription and related medical conditions, namely pain disorder, malignancy, autoimmune disease, and arthropathy. The Poisson regression was used to estimate odds ratios and 95% confidence intervals.
Results
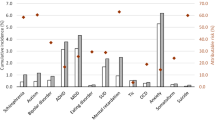
In total, 11,935 offspring of parents with BD and 119,350 offspring of parents without any MPD were included. After controlling for demographics and mental disorders, offspring of parents with BD demonstrated higher rates of prescription opioid use than those of parents without MPD, especially the intravenous/intramuscular form of opioids and prescription in hospital settings. In addition, offspring of parents with BD had a higher odds of pain disorders than those of parents without MPD.
Conclusion
Our study identifies a higher odd for developing pain disorders and exposure to prescription opioids among children of parents with BD.

Similar content being viewed by others
References
Grande I, Berk M, Birmaher B, Vieta E (2016) Bipolar disorder. Lancet 9(387):1561–1572
Murray CJL, Lopez AD, Harvard School of Public Health., World Health Organization., World Bank (1996) The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Published by the Harvard School of Public Health on behalf of the World Health Organization and the World Bank Harvard University Press, Cambridge
Novick DM, Swartz HA, Frank E (2010) Suicide attempts in bipolar I and bipolar II disorder: a review and meta-analysis of the evidence. Bipolar Disord 12:1–9
Nourse R, Reade C, Stoltzfus J, Mittal V (2014) Demographics, clinical characteristics, and treatment of aggressive patients admitted to the acute behavioral unit of a community general hospital: a prospective observational study. Prim Care Companion CNS Disord. https://doi.org/10.4088/PCC.13m01589
Rosa AR, Reinares M, Michalak EE et al (2010) Functional impairment and disability across mood states in bipolar disorder. Value Health 13:984–988
Woods SW (2000) The economic burden of bipolar disease. J clin psychiatry 61(Supp 13):38–41
Ketter TA (2015) Advances in treatment of bipolar disorders, 1st edn. American Psychiatric Pub, Washington, DC
Franklin GM, American Academy of N (2014) Opioids for chronic noncancer pain: a position paper of the American Academy of Neurology. Neurology 83:1277–1284
Spivak S, Cullen B, Eaton W et al (2018) Prescription opioid use among individuals with serious mental illness. Psychiatry Res 267:85–87
Martins SS, Keyes KM, Storr CL, Zhu H, Chilcoat HD (2009) Pathways between nonmedical opioid use/dependence and psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend 1(103):16–24
Merrill JO, Von Korff M, Banta-Green CJ et al (2012) Prescribed opioid difficulties, depression and opioid dose among chronic opioid therapy patients. Gen Hosp Psychiatry 34:581–587
Owen-Smith A, Stewart C, Sesay MM et al (2020) Chronic pain diagnoses and opioid dispensings among insured individuals with serious mental illness. BMC Psychiatry 20:40
Vadivelu N, Kai AM, Kodumudi G, Babayan K, Fontes M, Burg MM (2017) Pain and psychology-A reciprocal relationship. Ochsner J 17:173–180
Craddock N, Sklar P (2013) Genetics of bipolar disorder. Lancet 11(381):1654–1662
Kerner B (2014) Genetics of bipolar disorder. Appl Clin Genet 7:33–42
Huang JS, Yang FC, Chien WC et al (2021) Risk of Substance use disorder and its associations with comorbidities and psychotropic agents in patients with autism. JAMA Pediatr 1(175):e205371
Liang CS, Bai YM, Hsu JW et al (2020) The risk of sexually transmitted infections following first-episode schizophrenia among adolescents and young adults: a Cohort Study of 220 545 subjects. Schizophr Bull 8(46):795–803
Chen MH, Hsu JW, Huang KL et al (2018) Sexually transmitted infection among adolescents and young adults with attention-deficit/hyperactivity disorder: a Nationwide Longitudinal Study. J Am Acad Child Adolesc Psychiatry 57:48–53
Chen MH, Hsu JW, Huang KL et al (2018) Risk and coaggregation of major psychiatric disorders among first-degree relatives of patients with bipolar disorder: a nationwide population-based study. Psychol Med 12:1–8
Chen MH, Lan WH, Hsu JW et al (2016) Risk of developing type 2 diabetes in adolescents and young adults with autism spectrum disorder: a Nationwide Longitudinal Study. Diabetes Care 39:788–793
Zhang B, Wang HE, Bai YM et al (2021) Inflammatory bowel disease is associated with higher dementia risk: a nationwide longitudinal study. Gut 70:85–91
Charlson ME, Pompei P, Ales KL, Mackenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Arias F, Szerman N, Vega P, Mesias B, Basurte I, Rentero D (2017) Bipolar disorder and substance use disorders. Madrid study on the prevalence of dual disorders/pathology. Adicciones 29:186–194
Martins SS, Fenton MC, Keyes KM, Blanco C, Zhu H, Storr CL (2012) Mood and anxiety disorders and their association with non-medical prescription opioid use and prescription opioid-use disorder: longitudinal evidence from the National Epidemiologic Study on Alcohol and Related Conditions. Psychol Med 42:1261–1272
Huang B, Dawson DA, Stinson FS et al (2006) Prevalence, correlates, and comorbidity of nonmedical prescription drug use and drug use disorders in the United States: results of the national epidemiologic survey on alcohol and related conditions. J clin psychiatry 67:1062–1073
Edlund MJ, Martin BC, Fan MY, Devries A, Braden JB, Sullivan MD (2010) Risks for opioid abuse and dependence among recipients of chronic opioid therapy: results from the TROUP study. Drug Alcohol Depend 1(112):90–98
Park TW, Lin LA, Hosanagar A, Kogowski A, Paige K, Bohnert AS (2016) Understanding risk factors for opioid overdose in clinical populations to inform treatment and policy. J Addict Med 10:369–381
Albanese MJ, Clodfelter JR, Pardo RC, Ghaemi TB, Nassir S (2006) Underdiagnosis of bipolar disorder in men with substance use disorder. J Psychiatr Pract 12:124–127
Raouna A, Osam CS, Macbeth A (2018) Clinical staging model in offspring of parents with bipolar disorder: a systematic review. Bipolar Disord 20:313–333
Smith VC, Wilson CR, Committee on substance use, prevention (2016) Families affected by parental substance use. Pediatrics. https://doi.org/10.1542/peds.2016-1575
Straussner SLA, Fewell CH (2018) A review of recent literature on the impact of parental substance use disorders on children and the provision of effective services. Curr Opin Psychiatry 31:363–367
McHugh RK, Votaw VR, Sugarman DE, Greenfield SF (2018) Sex and gender differences in substance use disorders. Clin Psychol Rev 66:12–23
Lalli M, Brouillette K, Kapczinski F, De Azevedo CT (2021) Substance use as a risk factor for bipolar disorder: a systematic review. J Psychiatr Res 144:285–295
Stubbs B, Eggermont L, Mitchell AJ et al (2015) The prevalence of pain in bipolar disorder: a systematic review and large-scale meta-analysis. Acta Psychiatr Scand 131:75–88
Borsbo B, Peolsson M, Gerdle B (2009) The complex interplay between pain intensity, depression, anxiety and catastrophising with respect to quality of life and disability. Disabil Rehabil 31:1605–1613
Goesling J, Henry MJ, Moser SE et al (2015) Symptoms of depression are associated with opioid use regardless of pain severity and physical functioning among treatment-seeking patients with chronic pain. J Pain 16:844–851
Katon W, Lin EH, Kroenke K (2007) The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiatry 29:147–155
Stahl S, Briley M (2004) Understanding pain in depression. Hum Psychopharmacol 19(Suppl 1):S9–S13
Strigo IA, Simmons AN, Matthews SC, Craig AD, Paulus MP (2008) Association of major depressive disorder with altered functional brain response during anticipation and processing of heat pain. Arch Gen Psychiatry 65:1275–1284
Scherrer JF, Svrakic DM, Freedland KE et al (2014) Prescription opioid analgesics increase the risk of depression. J Gen Intern Med 29:491–499
Chen M, Jiang Q, Zhang L (2021) The prevalence of bipolar disorder in autoimmune disease: a systematic review and meta-analysis. Ann Palliat Med 10:350–361
Mariani SM (2004) Genes and autoimmune diseases - a complex inheritance. Med Gen Med 6:18
Jeanty C, Derderian SC, Mackenzie TC (2014) Maternal-fetal cellular trafficking: clinical implications and consequences. Curr Opin Pediatr 26:377–382
Busse JW, Craigie S, Juurlink DN et al (2017) Guideline for opioid therapy and chronic noncancer pain. CMAJ 8(189):E659–E666
Davis MA, Lin LA, Liu H, Sites BD (2017) Prescription opioid use among adults with mental health disorders in the United States. J Am Board Fam Med 30:407–417
Acknowledgements
The authors thank Mr I-Fan Hu, MA (Courtauld Institute of Art, University of London; National Taiwan University) for his friendship and support. Mr Hu declares no conflicts of interest.
Funding
The study was supported by grants from the Taipei Veterans General Hospital (V106B-020, V107B-010, V107C-181, V108B-012, V110C-025, V110B-002), the Yen Tjing Ling Medical Foundation (CI 109-21, CI 109-22, CI 110-30) and the Ministry of Science and Technology, Taiwan (107-2314-B-075-063-MY3, 108-2314-B-075-037). The funding source had no role in any process of our study.
Author information
Authors and Affiliations
Contributions
Drs MHC, YMB, and CSL: designed the study. Drs DJL, MHC, CSL: wrote the draft. Drs DJL, SJT, CMC, TPS, TCY and TJC: performed the literature review and revised the manuscript. Dr MHC performed the statistical analysis; all authors reviewed the final manuscript and agreed on its publication.
Corresponding authors
Ethics declarations
Conflict of interest
No conflict of interest. All authors have no financial relationships relevant to this article to disclose.
Ethical approval
This study was approved by the Institutional Review Board of the Taipei Veterans General Hospital (approval number: 2018-7-016AC) according to the current revision of the Declaration of Helsinki and national legal requirements (Human Subjects Research Act, Taiwan). Requirement for patient consent was waived because this study’s data were anonymous and derived wholly from a sizeable national database.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, DJ., Chen, MH., Bai, YM. et al. Association between parental bipolar disorder and increased risk of exposure to prescription opioids for their offspring. Soc Psychiatry Psychiatr Epidemiol 58, 267–275 (2023). https://doi.org/10.1007/s00127-022-02360-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-022-02360-5