Abstract
Purpose
There is a substantial gap between people having a mental disorder and those treated for this disorder. Studies that assessed the influence of age on healthcare use for major depressive disorder (MDD) have provided inconsistent results. We aimed to assess healthcare use in terms of treatment-seeking and psychotropic medication use in four age groups of 45- to 85-year-old community dwellers meeting criteria for MDD.
Methods
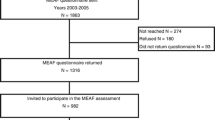
Data stemmed from CoLaus|PsyCoLaus, a population-based prospective cohort study. Diagnostic information on mental disorders, utilization of professional healthcare and psychotropic drugs was elicited using a semi-structured interview. Associations between age groups and healthcare use were established using logistic regression models with serial adjustments for socio-demographic and depression characteristics as well as comorbid mental disorders and cardio-metabolic features.
Results
Compared to participants of the youngest age group (ages 45 to 54 years), (1) those older than 75 years were less likely to use healthcare from psychiatrists or psychologists (OR: 0.4 [95% CI 0.17–0.96]), although the frequency of using any professional health care did not vary across age groups; (2) those older than 55 years used any psychotropic medication more frequently; and (3) those aged 55–64 years used antidepressants more frequently (OR: 1.61 [95% CI 1.07–2.44]), whereas those aged 65–74 years used anxiolytics more frequently (OR: 2.30 [95% CI 1.15–4.58]).
Conclusion
Age is a complex biological and social factor that influences healthcare use.

Similar content being viewed by others
Data availability
Data are available on request.
Code availability
Software applications and custom codes are available on request.
References
Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJ, Vos T, Whiteford HA (2013) Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med 10(11):e1001547. https://doi.org/10.1371/journal.pmed.1001547
Hoertel N, Sabatier J, Blanco C, Olfson M, Schuster JP, Airagnes G, Peyre H, Limosin F (2020) Contributing factors to heterogeneity in the timing of the onset of nonfatal suicidal behavior: results from a nationally representative study. J Clin Psychiatry 81(3):19m13017. https://doi.org/10.4088/JCP.19m13017
Global Burden of Disease Study 2013 Collaborators (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 386(9995):743–800. https://doi.org/10.1016/S0140-6736(15)60692-4
Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, de Girolamo G, Graaf R, Demyttenaere K, Gasquet I, Haro JM, Katz SJ, Kessler RC, Kovess V, Lépine JP, Ormel J, Polidori G, Russo LJ, Vilagut G, Almansa J, Arbabzadeh-Bouchez S, Autonell J, Bernal M, Buist-Bouwman MA, Codony M, Domingo-Salvany A, Ferrer M, Joo SS, Martínez-Alonso M, Matschinger H, Mazzi F, Morgan Z, Morosini P, Palacín C, Romera B, Taub N, Vollebergh WA, ESEMeD/MHEDEA 2000 Investigators (2004) Use of mental health services in Europe: European study of the epidemiology of mental disorders (ESEMeD) project. Acta Psychiatr Scand Suppl 420:47–54. https://doi.org/10.1111/j.1600-0047.2004.00330.x
Andreas S, Schulz H, Volkert J, Dehoust M, Sehner S, Suling A, Ausín B, Canuto A, Crawford M, Da Ronch C, Grassi L, Hershkovitz Y, Muñoz M, Quirk A, Rotenstein O, Santos-Olmo AB, Shalev A, Strehle J, Weber K, Wegscheider K, Wittchen HU, Härter M (2017) Prevalence of mental disorders in elderly people: the European MentDis_ICF65+ study. Br J Psychiatry 210(2):125–131. https://doi.org/10.1192/bjp.bp.115.180463
Volkert J, Härter M, Dehoust MC, Schulz H, Sehner S, Suling A, Wegscheider K, Ausín B, Canuto A, Crawford MJ, Da Ronch C, Grassi L, Hershkovitz Y, Muñoz M, Quirk A, Rotenstein O, Santos-Olmo AB, Shalev AY, Strehle J, Weber K, Wittchen HU, Andreas S (2017) Study approach and field work procedures of the MentDis_ICF65+ project on the prevalence of mental disorders in the older adult European population. BMC Psychiatry 17(1):366. https://doi.org/10.1186/s12888-017-1534-5
Kohn R, Saxena S, Levav I, Saraceno B (2004) The treatment gap in mental health care. Bull World Health Organ 82(11):858–866
Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, Olesen J, Allgulander C, Alonso J, Faravelli C, Fratiglioni L, Jennum P, Lieb R, Maercker A, van Os J, Preisig M, Salvador-Carulla L, Simonn R, Steinhausen HC (2011) The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol 21(9):655–679. https://doi.org/10.1016/j.euroneuro.2011.07.018
Bristow K, Patten S (2002) Treatment-seeking rates and associated mediating factors among individuals with depression. Can J Psychiatry 47(7):660–665. https://doi.org/10.1177/070674370204700708
Barry LC, Abou JJ, Simen AA, Gill TM (2012) Under-treatment of depression in older persons. J Affect Disord 136(3):789–796. https://doi.org/10.1016/j.jad.2011.09.038
Etchepare F, Pambrun E, Verdoux H, Tournier M (2017) Trends in patterns of antidepressant use in older general population between 2006 and 2012 following publication of practice guidelines. Int J Geriatr Psychiatry 32(8):849–859. https://doi.org/10.1002/gps.4536
Horackova K, Kopecek M, Machů V, Kagstrom A, Aarsland D, Motlova LB, Cermakova P (2019) Prevalence of late-life depression and gap in mental health service use across European regions. Eur Psychiatry 57:19–25. https://doi.org/10.1016/j.eurpsy.2018.12.002
Andreas S, Dehoust M, Volkert J, Schulz H, Sehner S, Suling A, Wegscheider K, Ausín B, Canuto A, Crawford MJ, Da Ronch C, Grassi L, Hershkovitz Y, Muñoz M, Quirk A, Rotenstein O, Belén Santos-Olmo A, Shalev AY, Weber K, Wittchen HU, Härter M (2019) Affective disorders in the elderly in different European countries: results from the MentDis_ICF65+ study. PLoS ONE 14(11):e0224871. https://doi.org/10.1371/journal.pone.0224871
Magaard JL, Seeralan T, Schulz H, Brütt AL (2017) Factors associated with help-seeking behaviour among individuals with major depression: a systematic review. PLoS ONE 12(5):e0176730. https://doi.org/10.1371/journal.pone.0176730
Firmann M, Mayor V, Vidal PM, Bochud M, Pecoud A, Hayoz D, Paccaud F, Preisig M, Song KS, Yuan X, Danoff TM, Stirnadel HA, Waterworth D, Mooser V, Waeber G, Vollenweider P (2008) CoLaus study: a population-based study to investigate the epidemiology and genetic determinants of cardiovascular risk factors and metabolic syndrome. BMC Cardiovasc Disord 8:6. https://doi.org/10.1186/1471-2261-8-6
Preisig M, Waeber G, Vollenweider P, Bovet P, Rothen S, Vandeleur C, Guex P, Middleton L, Waterworth D, Mooser V, Tozzi F, Muglia P (2009) The PsyCoLaus study: methodology and characteristics of the sample of a population-based survey on psychiatric disorders and their association with genetic and cardiovascular risk factors. BMC Psychiatry 9:9. https://doi.org/10.1186/1471-244X-9-9
Nurnberger JI, Blehar MC, Kaufmann CA, York-Cooler C, Simpson SG, Harkavy-Friedman J, Severe JB, Malaspina D, Reich T (1994) Diagnostic interview for genetic studies. Rationale, unique features, and training. NIMH genetics initiative. Arch Gen Psychiatry 51(11):849–859. https://doi.org/10.1001/archpsyc.1994.03950110009002
Leboyer M, Barbe B, Gorwood P, Teherani M, Allilaire JF, Preisig M, Matthey ML, Poyetton V, Ferrero F (1995) Interview diagnostique pour les etudes génétiques. INSERM, Paris
Preisig M, Fenton BT, Matthey ML, Berney A, Ferrero F (1999) Diagnostic interview for genetic studies (DIGS): inter-rater and test-retest reliability of the French version. Eur Arch Psychiatry Clin Neurosci 249(4):174–179. https://doi.org/10.1007/s004060050084
Berney A, Preisig M, Matthey ML, Ferrero F, Fenton BT (2002) Diagnostic interview for genetic studies (DIGS): inter-rater and test-retest reliability of alcohol and drug diagnoses. Drug Alcohol Depend 65(2):149–158. https://doi.org/10.1016/s0376-8716(01)00156-9
Leboyer M, Maier W, Teherani M, Lichtermann D, D’Amato T, Franke P, Lepine JP, Minges J, McGuffin P (1991) The reliability of the SADS-LA in a family study setting. Eur Arch Psychiatry Clin Neurosci 241(3):165–169. https://doi.org/10.1007/BF02219716
Endicott J, Spitzer RL (1978) A diagnostic interview: the schedule for affective disorders and schizophrenia. Arch Gen Psychiatry 35(7):837–844. https://doi.org/10.1001/archpsyc.1978.01770310043002
American Psychiatric Association (2000) DSM-IV-TR: diagnostic and statistical manual of mental disorders, 4th edn, text revision. Washington DC USA
Hollingshead AB (1975) Four factor index of social status. Yale University Press
Volkert J, Andreas S, Härter M, Dehoust MC, Sehner S, Suling A, Ausin B, Canuto A, Crawford MJ, Da Ronch C, Grassi L, Hershkovitz Y, Munoz M, Quirk A, Rotenstein O, Santos-Olmo AB, Shalev AY, Strehle J, Weber K, Wegscheider K, Wittchen HU, Schulz H (2018) Predisposing, enabling, and need factors of service utilization in the elderly with mental health problems. Int Psychogeriatr 30(7):1027–1037. https://doi.org/10.1017/S1041610217002526
Handley TE, Kay-Lambkin FJ, Inder KJ, Lewin TJ, Attia JR, Fuller J, Perkins D, Coleman C, Weaver N, Kelly BJ (2014) Self-reported contacts for mental health problems by rural residents: predicted service needs, facilitators and barriers. BMC Psychiatry 6(14):249. https://doi.org/10.1186/s12888-014-0249-0
Crabb R, Hunsley J (2006) Utilization of mental health care services among older adults with depression. J Clin Psychol 62(3):299–312. https://doi.org/10.1002/jclp.20231
Gabilondo A, Rojas-Farreras S, Rodriguez A, Fernandez A, Pinto-Meza A, Vilagut G, Haro JM, Alonso J (2011) Use of primary and specialized mental health care for a major depressive episode in Spain by ESEMeD respondents. Psychiatr Serv 62(2):152–161. https://doi.org/10.1176/ps.62.2.pss6202_0152
Manetti A, Hoertel N, Le Strat Y, Schuster JP, Lemogne C, Limosin F (2014) Comorbidity of late-life depression in the United States: a population-based study. Am J Geriatr Psychiatry 22(11):1292–1306. https://doi.org/10.1016/j.jagp.2013.05.001
Gonçalves DC, Coelho CM, Byrne GJ (2014) The use of healthcare services for mental health problems by middle-aged and older adults. Arch Gerontol Geriatr 59(2):393–397. https://doi.org/10.1016/j.archger.2014.04.013
Luppa M, Sikorski S, Motzek T, Konnopka A, König HH, Riedel-Heller SG (2012) Health service utilization and costs of depressive symptoms in late life-a systematic review. Curr Pharm Des 18(36):5936–5957. https://doi.org/10.2174/138161212803523572
Chaplin R, Farquharson L, Clapp M, Crawford M (2015) Comparison of access, outcomes and experiences of older adults and working age adults in psychological therapy. Int J Geriatr Psychiatry 30(2):178–184. https://doi.org/10.1002/gps.4122
Schnyder N, Panczak R, Groth N, Schultze-Lutter F (2017) Association between mental health-related stigma and active help-seeking: systematic review and meta-analysis. Br J Psychiatry 210(4):261–268. https://doi.org/10.1192/bjp.bp.116.189464
Wuthrich VM, Frei J (2015) Barriers to treatment for older adults seeking psychological therapy. Int Psychogeriatr 27(7):1227–1236. https://doi.org/10.1017/S1041610215000241
Stark A, Kaduszkiewicz H, Stein J, Maier W, Heser K, Weyerer S, Werle J, Wiese B, Mamone S, König HH, Bock JO, Riedel-Heller SG, Scherer M (2018) A qualitative study on older primary care patients’ perspectives on depression and its treatments-potential barriers to and opportunities for managing depression. BMC Fam Pract 19(1):2. https://doi.org/10.1186/s12875-017-0684-3
Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS, Replication NCS (2003) The epidemiology of major depressive disorder: results from the National comorbidity survey replication (NCS-R). JAMA 289(23):3095–3105. https://doi.org/10.1001/jama.289.23.3095
Beck CA, Patten SB, Williams JV, Wang JL, Currie SR, Maxwell CJ, El-Guebaly N (2005) Antidepressant utilization in Canada. Soc Psychiatry Psychiatr Epidemiol 40(10):799–807. https://doi.org/10.1007/s00127-005-0968-0
Carragher N, Adamson G, Bunting B, McCann S (2010) Treatment-seeking behaviours for depression in the general population: results from the National epidemiologic survey on alcohol and related conditions. J Affect Disord 121(1–2):59–67. https://doi.org/10.1016/j.jad.2009.05.009
Kok RM, Reynolds CF 3rd (2017) Management of depression in older adults: a review. JAMA 317(20):2114–2122
Haller E, Watzke B, Blozik E, Rosemann T, Reich O, Huber CA, Wolf M (2019) Antidepressant prescription practice and related factors in Switzerland: a cross-sectional analysis of health claims data. BMC Psychiatry 19(1):196. https://doi.org/10.1186/s12888-019-2178-4
Hansen DG, Rosholm JU, Gichangi A, Vach W (2007) Increased use of antidepressants at the end of life: population-based study among people aged 65 years and above. Age Ageing 36(4):449–454. https://doi.org/10.1093/ageing/afm056
Sun Y, Möller J, Lundin A, Wong SYS, Yip BHK, Forsell Y (2018) Utilization of psychiatric care and antidepressants among people with different severity of depression: a population-based cohort study in Stockholm, Sweden. Soc Psychiatry Psychiatr Epidemiol 53(6):607–615. https://doi.org/10.1007/s00127-018-1515-0
Rhodes AE, Fung K (2004) Self-reported use of mental health services versus administrative records: care to recall? Int J Methods Psychiatr Res 13(3):165–175. https://doi.org/10.1002/mpr.172
Acknowledgements
The authors express their gratitude to the Lausanne inhabitants who volunteered to participate in the CoLaus|PsyCoLaus study and to all the collaborators who contributed to the coordination of the study and the collection of data.
Funding
The CoLaus|PsyCoLaus study was and is supported by research grants from GlaxoSmithKline, the Faculty of Biology and Medicine of Lausanne, and the Swiss National Science Foundation (grants 3200B0–105993, 3200B0-118308, 33CSCO-122661, 33CS30-139468; 33CS30-148401 and 33CS30_177535).
Author information
Authors and Affiliations
Contributions
JPS: design, analysis, literature search, manuscript drafting. MPFS: design, analysis, figures, statistical analysis and data visualization, manuscript drafting and review. NH: design, literature search, analysis, manuscript drafting and review. PMV, CLV, FL: analysis, manuscript drafting and review. MP: design, analysis, funding acquisition, manuscript drafting and review. AvG: design, analysis, manuscript drafting and review. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The institutional Ethics Committee of the University of Lausanne, which afterwards became the Ethics Commission of Canton Vaud (www.cer-vd.ch) approved the baseline CoLaus|PsyColaus study (reference 16/03). The approval was renewed for the first (reference 33/09) and the second (reference 26/14) follow-ups. The study was performed in agreement with the Helsinki declaration and its former amendments, and in accordance with the applicable Swiss legislation.
Consent to participate
All participants signed a written informed consent, prior to their inclusion in the study.
Consent for publication
Patients signed informed consent regarding publishing their data, provided that individuals could not be identified as a subject.
Rights and permissions
About this article
Cite this article
Schuster, JP., Strippoli, MP.F., Hoertel, N. et al. Healthcare use for major depressive disorders among middle-aged and older adults in the community. Soc Psychiatry Psychiatr Epidemiol 57, 953–961 (2022). https://doi.org/10.1007/s00127-021-02193-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-021-02193-8