Abstract
Background
People with severe mental illness often struggle with social relationships, but differences among diagnostic groups are unclear. We assessed and compared objective and subjective social relationship indicators among patients with psychotic, mood and neurotic disorders one year after hospitalisation in five European countries (Belgium, Germany, Italy, Poland and United Kingdom).
Methods
The number of social contacts, including family members and friends during the previous week (Social Network Schedule), and satisfaction with the number and quality of friendships (Manchester Short Assessment of Quality of Life Quality) were assessed by face-to-face interview. Linear regression models were used to analyse associations with diagnostic groups.
Results
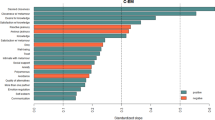
Participants (n = 2155) reported on average 2.79 ± 2.37 social contacts overall in the previous week, among whom, a mean of 1.65 ± 1.83 (59.2 ± 38.7%) were friends. Satisfaction with friendships was moderate (mean 4.62, SD 1.77). In the univariable model, patients with psychotic disorders reported having less social contact with friends than those with either mood (p < 0.05) or neurotic disorders (p < 0.001), but this difference disappeared when adjusting for socioeconomic and clinical variables (β = − 0.106, 95% CI − 0.273 to 0.061, p = 0.215). Satisfaction with friendships was similar across diagnostic groups in both univariable (β = − 0.066, 95% CI − 0.222 to 0.090, p = 0.408) and multivariable models (β = 0.067, 95% CI − 0.096 to 0.229, p = 0.421). The two indicators showed a weak correlation in the total sample (total social contacts, rs = 0.266; p < 0.001; friends, rs = 0.326, p < 0.001).
Conclusion
While objective and subjective social relationship indicators appear to be weakly correlated concepts, there is no variation in either indicator across diagnostic groups when confounders are taken into account among patients with severe mental illness. Interventions specifically targeting social relationships are needed, but they do not necessitate diagnosis-specific adaptations.

Similar content being viewed by others
References
Umberson D, Montez JK (2010) Social relationships and health: a flashpoint for health policy. J Health Soc Behav 51:S54–S66
Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, Adler N (2013) Social isolation: a predictor of mortality comparable to traditional clinical risk factors. Am J Pub Health 103:2056–2062
Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D (2015) Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci 10:227–237
Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B (2016) Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart 102:1009–1016
Jaremka LM, Andridge RR, Fagundes CP, Alfano CM, Povoski SP, Lipari AM, Kiecolt-Glaser JK (2014) Pain, depression, and fatigue: loneliness as a longitudinal risk factor. Health Psychol 33:948–957
Brugha T, Jenkins R, Bebbington P, Meltzer H, Lewis G, Farell M (2004) Risk factors and the prevalence of neurosis and psychosis in ethnic groups in Great Britain. Soc Psychiatry Psychiatr Epidemiol 39:939–946
Borge L, Martinsen EW, Ruud R, Watne Ø, Friis S (1999) Quality of life, loneliness, and social contact among long-term psychiatric patients. Psychiatr Serv 50:81–84
Bengtsson-Tops A, Hansson L (2001) Quantitative and qualitative aspects of the social network in schizophrenic patients living in the community. Relationship to sociodemographic characteristics and clinical factors and subjective quality of life. Int J Soc Psychiatry 47:67–77
Shiovitz-Ezra S, Ayalon L (2010) Situational versus chronic loneliness as risk factors for all-cause mortality. Int Psychogeriatr 22:455–462
Rico-Uribe LA, Caballero FF, Martín-María N, Cabello M, Ayuso-Mateos JL, Miret M (2018) Association of loneliness with all-cause mortality: a meta-analysis. PLoS ONE 13(1):e0190033
Meltzer H, Bebbington P, Dennis MS, Jenkins R, McManus S, Brugha TS (2013) Feelings of loneliness among adults with mental disorder. Soc Psychiatry Psychiatr Epidemiol 48:5–13
Palumbo C, Volpe U, Matanov A, Priebe S, Giacco D (2015) Social networks of patients with psychosis: a systematic review. BMC Res Notes 8:560
Holwerda T, Beekman A, Deeg D, Stek M, Van Tilburg T, Visser P, Schoevers R (2012) Increased risk of mortality associated with social isolation in older men: only when feeling lonely? Results from the Amsterdam Study of the Elderly (AMSTEL). Psychol Med 42:843–853
Wang J, Lloyd-Evans B, Giacco D, Forsyth R, Nebo C, Mann F, Johnson S (2017) Social isolation in mental health: a conceptual and methodological review. Soc Psychiatry Psychiatr Epidemiol 52:1451–1461
Anderson-Gayer XC, Morgan C (2013) Social networks, support and early psychosis: a systematic review. Epidemiol Psychiatr Sci 22:131–146
Cannon M, Jones P, Gilvarry C, Rifkin L, McKenzie K, Foerster A, Murray R (1997) Premorbid social functioning in schizophrenia and bipolar disorder: similarities and differences. Am J Psychiatry 154:1544–1550
Visentini C, Cassidy M, Bird VJ, Priebe S (2018) Social networks of patients with chronic depression: a systematic review. J Affect Disord 241:571–578
Giacco D, Palumbo C, Strappelli N, Catapano F, Priebe S (2016) Social contacts and loneliness in people with psychotic and mood disorders. Compr Psychiatry 66:59–66
Terzian E, Tognoni G, Bracco R, De Ruggieri E, Ficociello RA, Mezzina R, Pillo G (2013) Social network intervention in patients with schizophrenia and marked social withdrawal: a randomized controlled study. Can J Psychiatry 58:622–631
Anderson K, Laxhman N, Priebe S (2015) Can mental health interventions change social networks? A systematic review. BMC Psychiatry 15:297
Giacco D, Bird VJ, Ahmad T, Bauer M, Lasalvia A, Lorant V, Miglietta E, Moskalewicz J, Nicaise P, Pfenning A, Welbel M, Priebe S (2018) The same or different psychiatrists for in- and out-patient treatment? A multi-country natural experiment. Epidemiol Psychiatr Sci 18:1–9
World Health Organization (1992) The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. WHO, Geneva
Dunn M, O'Driscoll C, Dayson D, Wills W, Leff J (1990) The TAPS Project. 4: an observational study of the social life of long-stay patients. Br J Psychiatry 157:842–848
Priebe S, Huxley P, Knight S, Evans S (1999) Application and results of the Manchester Short Assessment of Quality of Life (MANSA). Int J Soc Psychiatry 45:7–12
Guy W (2000) Clinical global impressions (CGI) scale. Psychiatric measures. APA, Washington DC
Ormel J, Jeronimus BF, Kotov R, Riese H, Bos EH, Hankin B, Rosmalen JGM, Oldehinkel AJ (2013) Neuroticism and common mental disorders: meaning and utility of a complex relationship. Clin Psychol Rev 33:686–697
Li X, Wong W, Lamoureux EL, Wong TY (2012) Are linear regression techniques appropriate for analysis when the dependent (outcome) variable is not normally distributed? Investig Ophthalmol Vis Sci 53:3082–3083
Gariepy G, Honkaniemi H, Quesnel-Vallee A (2016) Social support and protection from depression: systematic review of current findings in Western countries. Br J Psychiatry 209:284–293
Wyngaerden F, Nicaise P, Dubois V, Lorant V (2019) Social support network and continuity of care: an ego-network study of psychiatric services. Soc Psychiatry Psychiatr Epidemiol 54:725–735
Dozier M, Harris M, Bergman H (1987) Social network density and rehospitalization among young adult patients. Hosp Community Psychiatry 38:61–65
Sörgaard K, Hansson L, Heikkilä J, Vinding HR, Bjarnason O, Bengtsson-Tops A, Merinder L, Nilsson LL, Sandlund M, Middlenoe T (2001) Predictors of social relations in persons with schizophrenia living in the community: a Nordic multicentre study. Soc Psychiatry Psychiatr Epidemiol 36:13–19
Putnam R (1995) Bowling alone: America’s declining social capital. J Democr 6:64–78
Ehsan AM, de Silva MJ (2015) Social capital and common mental disorder: a systematic review. J Epidemiol Comm Health 69:1021–1028
Rüesch P, Graf J, Meyer PC, Rössler W, Hell D (2004) Occupation, social support and quality of life in persons with schizophrenic or affective disorders. Soc Psychiatry Psychiatr Epidemiol 39:686–694
Nagy E, Moore S (2017) Social interventions: an effective approach to reduce adult depression? J Aff Dis 218:131–152
Giacco D, McCabe R, Kallert T, Hansson L, Fiorillo A, Priebe S (2012) Friends and symptom dimensions in patients with psychosis: a pooled analysis. PLoS ONE 7(11):e50119
Nasser EH, Overholser JV (2005) Recovery from major depression: the role of support from family, friends, and spiritual beliefs. Acta Psychiatr Scand 111:125–132
Acknowledgements
The authors would like to thank the wider COFI study group, the support of the funders, the supporting services and the participants who took part in the study.
Funding
This study was funded by the European Commission 7th Framework Programme. Grant agreement number is 602645.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Ethical approval was obtained in all participating countries: Belgium: Comité d’Ethique hospitalo-facultaire des Cliniques St-Luc Brussels; Germany: Ethical Board, Technische Universität Dresden; Italy: Comitati Etici per la sperimentazione clinica (CESC) delle provincie di Verona, Rovigo, Vicenza, Treviso, Padova; Poland: Komisja Bioetyczna przy Instytucie Psychiatrii i Neurologii w Warszawie; and UK: National Research Ethics Committee North East—Newcastle & North Tyneside (ref: 14/NE/1017).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Buhagiar, K., Priebe, S., Klingemann, J. et al. Social contacts, friends and satisfaction with friendships in patients with psychotic, mood and neurotic disorders 1 year after hospitalisation: data from five European countries. Soc Psychiatry Psychiatr Epidemiol 56, 363–373 (2021). https://doi.org/10.1007/s00127-020-01915-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-020-01915-8