Abstract
Purpose
Social support is an important correlate of health behaviors and outcomes. Studies suggest that veterans have lower social support than civilians, but interpretation is hindered by methodological limitations. Furthermore, little is known about how sex influences veteran–civilian differences. Therefore, we examined veteran–civilian differences in several dimensions of social support and whether differences varied by sex.
Methods
We performed a cross-sectional analysis of the 2012–2013 National Epidemiologic Survey of Alcohol and Related Conditions-III, a nationally representative sample of 34,331 respondents (male veterans = 2569; female veterans = 356). We examined veteran–civilian differences in functional and structural social support using linear regression and variation by sex with interactions. We adjusted for socio-demographics, childhood experiences, and physical and mental health.
Results
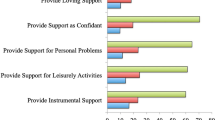
Compared to civilians, veterans had lower social network diversity scores (difference [diff] = − 0.13, 95% confidence interval [CI] − 0.23, − 0.03). Among women but not men, veterans had smaller social network size (diff = − 2.27, 95% CI − 3.81, − 0.73) than civilians, attributable to differences in religious groups, volunteers, and coworkers. Among men, veterans had lower social network diversity scores than civilians (diff = − 0.13, 95% CI − 0.23, − 0.03); while among women, the difference was similar but did not reach statistical significance (diff = − 0.13, 95% CI − 0.23, 0.09). There was limited evidence of functional social support differences.
Conclusion
After accounting for factors that influence military entry and social support, veterans reported significantly lower structural social support, which may be attributable to reintegration challenges and geographic mobility. Findings suggest that veterans could benefit from programs to enhance structural social support and improve health outcomes, with female veterans potentially in greatest need.
Similar content being viewed by others
References
Holt-Lunstad J, Smith TB, Layton JB (2010) Social relationships and mortality risk: a meta-analytic review. PLoS Med 7:e1000316. https://doi.org/10.1371/journal.pmed.1000316
Lindsay Smith G, Banting L, Eime R et al (2017) The association between social support and physical activity in older adults: a systematic review. Int J Behav Nutr Phys Act 14:56. https://doi.org/10.1186/s12966-017-0509-8
Gallant MP (2003) The influence of social support on chronic illness self-management: a review and directions for research. Health Educ Behav 30:170–195. https://doi.org/10.1177/1090198102251030
Cohen S (1997) Social ties and susceptibility to the common cold. JAMA J Am Med Assoc 277:1940. https://doi.org/10.1001/jama.1997.03540480040036
Wang H-X, Mittleman MA, Orth-Gomer K (2005) Influence of social support on progression of coronary artery disease in women. Soc Sci Med 60:599–607. https://doi.org/10.1016/j.socscimed.2004.05.021
Leavy RL (1983) Social support and psychological disorder: a review. J Community Psychol 11:3–21
Kleiman EM, Liu RT (2013) Social support as a protective factor in suicide: findings from two nationally representative samples. J Affect Disord 150:540–545. https://doi.org/10.1016/j.jad.2013.01.033
Cohen S, Mermelstein R, Kamarck T, Hoberman HM (1985) Measuring the Functional Components of Social Support. In: Sarason IG, Sarason BR (eds) Social support: theory, research and applications. Springer Netherlands, Dordrecht, pp 73–94
Antonucci TC, Akiyama H (1987) Social networks in adult life and a preliminary examination of the convoy model. J Gerontol 42:519–527
U.S. Department of Veterans Affairs National Center for Veterans Analysis and Statistics. https://www.va.gov/vetdata/. Accessed 30 Jan 2019
Hoerster KD, Lehavot K, Simpson T et al (2012) Health and Health Behavior Differences. Am J Prev Med 43:483–489. https://doi.org/10.1016/j.amepre.2012.07.029
Lehavot K, Hoerster KD, Nelson KM et al (2012) Health indicators for military, veteran, and civilian women. Am J Prev Med 42:473–480. https://doi.org/10.1016/j.amepre.2012.01.006
Elnitsky CA, Blevins CL, Fisher MP, Magruder K (2017) Military service member and veteran reintegration: a critical review and adapted ecological model. Am J Orthopsychiatry 87:114–128. https://doi.org/10.1037/ort0000244
Nagy E, Moore S (2017) Social interventions: an effective approach to reduce adult depression? J Affect Disord 218:131–152. https://doi.org/10.1016/j.jad.2017.04.043
Siette J, Cassidy M, Priebe S (2017) Effectiveness of befriending interventions: a systematic review and meta-analysis. BMJ Open 7:e014304. https://doi.org/10.1136/bmjopen-2016-014304
Vorderstrasse A, Lewinski A, Melkus GD, Johnson C (2016) Social support for diabetes self-management via eHealth interventions. Curr Diab Rep. https://doi.org/10.1007/s11892-016-0756-0
Angel CM, Woldetsadik MA, Armstrong NJ et al (2020) The Enriched Life Scale (ELS): Development, exploratory factor analysis, and preliminary construct validity for US military veteran and civilian samples. Transl Behav Med 10:278–291. https://doi.org/10.1093/tbm/iby109
Kobau R, Bann C, Lewis M et al (2013) Mental, social, and physical well-being in New Hampshire, Oregon, and Washington, 2010 Behavioral Risk Factor Surveillance System: implications for public health research and practice related to Healthy People 2020 foundation health measures on well-being. Popul Health Metr 11:19. https://doi.org/10.1186/1478-7954-11-19
Fisher GG, Matthews RA, Gibbons AM (2016) Developing and investigating the use of single-item measures in organizational research. J Occup Health Psychol 21:3–23. https://doi.org/10.1037/a0039139
Jordan BK, Schlenger WE, Hough R et al (1991) Lifetime and current prevalence of specific psychiatric disorders among vietnam veterans and controls. Arch Gen Psychiatry 48:207–215. https://doi.org/10.1001/archpsyc.1991.01810270019002
Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM (2000) Are patients at veterans affairs medical centers sicker?: a comparative analysis of health status and medical resource use. Arch Intern Med 160:3252–3257. https://doi.org/10.1001/archinte.160.21.3252
Blosnich JR, Dichter ME, Cerulli C et al (2014) Disparities in adverse childhood experiences among individuals with a history of military service. JAMA Psychiatry 71:1041. https://doi.org/10.1001/jamapsychiatry.2014.724
Katon JG, Lehavot K, Simpson TL et al (2015) Adverse childhood experiences, military service, and adult health. Am J Prev Med 49:573–582. https://doi.org/10.1016/j.amepre.2015.03.020
Bareis N, Mezuk B (2016) The relationship between childhood poverty, military service, and later life depression among men: evidence from the Health and Retirement Study. J Affect Disord 206:1–7. https://doi.org/10.1016/j.jad.2016.07.018
Antonucci TC, Akiyama H (1987) An examination of sex differences in social support among older men and women. Sex Roles 17:737–749. https://doi.org/10.1007/BF00287685
Frayne SM, Parker VA, Christiansen CL et al (2006) Health status among 28,000 women veterans: the VA women’s health program evaluation project. J Gen Intern Med 21:S40–S46. https://doi.org/10.1111/j.1525-1497.2006.00373.x
Grant BF, Amsbary M, Chu A et al (2014) Source and accuracy statement: national epidemiologic survey on alcohol and related conditions-III (NESARC-III). National Institute on Alcohol Abuse and Alcoholism, Rockville, MD. https://www.niaaa.nih.gov/sites/default/files/NESARC_Final_Report_FINAL_1_8_15.pdf. Accessed 06 Dec 2019
Cohen S (2004) Social relationships and health. Am Psychol 59:676–684
Merz EL, Roesch SC, Malcarne VL et al (2014) Validation of Interpersonal Support Evaluation List-12 (ISEL-12) scores among English- and Spanish-Speaking Hispanics/Latinos from the HCHS/SOL Sociocultural Ancillary Study. Psychol Assess 26:384–394. https://doi.org/10.1037/a0035248
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Publishing, Arlington
Dube SR, Felitti VJ, Dong M et al (2003) Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics 111:564–572. https://doi.org/10.1542/peds.111.3.564
Ross J, Waterhouse-Bradley B, Contractor AA, Armour C (2018) Typologies of adverse childhood experiences and their relationship to incarceration in U.S. military veterans. Child Abuse Negl 79:74–84. https://doi.org/10.1016/j.chiabu.2018.01.023
Schüssler-Fiorenza Rose SM, Eslinger JG, Zimmerman L et al (2016) Adverse childhood experiences, support, and the perception of ability to work in adults with disability. PLoS ONE 11:e0157726. https://doi.org/10.1371/journal.pone.0157726
Nurius PS, Fleming CM, Brindle E (2019) Life course pathways from adverse childhood experiences to adult physical health: a structural equation model. J Aging Health 31:211–230. https://doi.org/10.1177/0898264317726448
Hughes K (2017) The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health 2:e356–e366. https://doi.org/10.1016/S2468-2667(17)30118-4
Pearl J (1995) Causal diagrams for empirical research. Biometrika 82:669–688. https://doi.org/10.2307/2337329
Textor J, van der Zander B, Gilthorpe MS et al (2016) Robust causal inference using directed acyclic graphs: the R package ‘dagitty’. Int J Epidemiol 45:1887–1894. https://doi.org/10.1093/ije/dyw341
Patulny R, Siminski P, Mendolia S (2015) The front line of social capital creation—a natural experiment in symbolic interaction. Soc Sci Med 125:8–18. https://doi.org/10.1016/j.socscimed.2014.04.026
Sayer NA, Friedemann-Sanchez G, Spoont M et al (2009) A qualitative study of determinants of PTSD treatment initiation in veterans. Psychiatry Interpers Biol Process 72:238–255. https://doi.org/10.1521/psyc.2009.72.3.238
Han SC, Castro F, Lee LO et al (2014) Military unit support, postdeployment social support, and PTSD symptoms among active duty and National Guard soldiers deployed to Iraq. J Anxiety Disord 28:446–453. https://doi.org/10.1016/j.janxdis.2014.04.004
Sandstrom GM, Dunn EW (2014) Social interactions and well-being: the surprising power of weak ties. Pers Soc Psychol Bull 40:910–922. https://doi.org/10.1177/0146167214529799
Lehavot K, Litz B, Millard SP et al (2017) Study adaptation, design, and methods of a web-based PTSD intervention for women Veterans. Contemp Clin Trials 53:68–79. https://doi.org/10.1016/j.cct.2016.12.002
Drebing CE, Reilly E, Henze KT et al (2018) Using peer support groups to enhance community integration of veterans in transition. Psychol Serv 15:135–145. https://doi.org/10.1037/ser0000178
Heisler M, Vijan S, Makki F, Piette JD (2010) Diabetes control with reciprocal peer support versus nurse care management: a randomized Trial. Ann Intern Med 153:507. https://doi.org/10.7326/0003-4819-153-8-201010190-00007
Eisen SV, Schultz MR, Mueller LN et al (2012) Outcome of a randomized study of a mental health peer education and support group in the VA. Psychiatr Serv 63:1243–1246. https://doi.org/10.1176/appi.ps.201100348
Fischer EP, Sherman MD, Han X, Owen RR (2013) Outcomes of participation in the REACH multifamily group program for veterans with PTSD and their families. Prof Psychol Res Pract 44:127–134. https://doi.org/10.1037/a0032024
Holt-Lunstad J, Robles TF, Sbarra DA (2017) Advancing social connection as a public health priority in the United States. Am Psychol 72:517–530. https://doi.org/10.1037/amp0000103
National Association of Community Health Centers (2019) Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences: About the PRAPARE Assessment Tool. In: Protoc. Responding Assess. Patients Assets Risks Exp. https://www.nachc.org/research-and-data/prapare/about-the-prapare-assessment-tool/. Accessed 9 Sept 2019
Mota NP, Tsai J, Sareen J et al (2016) High burden of subthreshold DSM-5 post-traumatic stress disorder in U.S. military veterans. World Psychiatry 15:185–186. https://doi.org/10.1002/wps.20313
Jakupcak M, Hoerster KD, Varra A et al (2011) Hopelessness and suicidal ideation in Iraq and Afghanistan War Veterans reporting subthreshold and threshold posttraumatic stress disorder. J Nerv Ment Dis 199:272–275
National Center for Veterans Analysis and Statistics (2017) Women Veterans Report: The Past, Present, and Future of Women Veterans. Department of Veterans Affairs
Althouse AD (2016) Adjust for Multiple Comparisons? It’s Not That Simple. Ann Thorac Surg 101:1644–1645. https://doi.org/10.1016/j.athoracsur.2015.11.024
Meffert BN, Morabito DM, Sawicki DA et al (2019) US veterans who do and do not utilize veterans affairs health care services: demographic, military, medical, and psychosocial characteristics. Prim Care Companion CNS Disord. https://doi.org/10.4088/PCC.18m02350
Griffith J (2010) Citizens coping as soldiers: a review of deployment stress symptoms among reservists. Mil Psychol 22:176–206. https://doi.org/10.1080/08995601003638967
Elovainio M, Hakulinen C, Pulkki-Råback L et al (2017) Contribution of risk factors to excess mortality in isolated and lonely individuals: an analysis of data from the UK Biobank cohort study. Lancet Public Health 2:e260–e266. https://doi.org/10.1016/S2468-2667(17)30075-0
McPherson M, Smith-Lovin L, Brashears ME (2006) Social isolation in america: changes in core discussion networks over two decades. Am Sociol Rev 71:353–375. https://doi.org/10.1177/000312240607100301
Sachs JD, Layard R, Helliwell JF (2018) World Happiness Report 2018. Sustainable Development Solutions Network, New York. https://s3.amazonaws.com/happiness-report/2018/WHR_web.pdf. Accessed 4 Jan 2020
Acknowledgements
Dr. Gray and Dr. Hoerster were supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development Program (CDAs 16–154 and 12–263). Dr. Campbell was supported by VA Office of Academic Affiliations’ Advanced Fellowship in Health Services Research and Development (TPH 61–000-23). Dr. Fortney was supported by a VA Research Career Scientist Award (RCS 17–153). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical approval
This was a secondary data analysis and does not contain clinical studies or patient data.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Campbell, S.B., Gray, K.E., Hoerster, K.D. et al. Differences in functional and structural social support among female and male veterans and civilians. Soc Psychiatry Psychiatr Epidemiol 56, 375–386 (2021). https://doi.org/10.1007/s00127-020-01862-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-020-01862-4