Abstract
Background
Increasing rates of antipsychotic prescribing have been reported previously, particularly for second-generation antipsychotics (SGAs), which are generally better tolerated than the older first-generation antipsychotics (FGAs). Prescribers, however, may exert bias, favouring prescriptions of novel drugs for patients of higher socioeconomic status (SES). We aimed to examine time trends in: (1) prescriptions of oral FGAs vs. SGAs and (2) associations between antipsychotic prescriptions and neighbourhood-level SES in England between 2011 and 2016.
Methods
We used publicly available data for prescriptions made in primary care and linked general practices’ postcodes with the Index of Multiple Deprivation (IMD) as a measure for neighbourhood-level SES. Absolute numbers of antipsychotic prescriptions were calculated. Linear regression analysis was used to examine the association of SGA vs. FGA prescription pattern with time and with SES.
Results
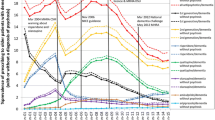
A total of 27,486,000 oral antipsychotics were prescribed during the study period, mostly SGAs (n = 21,700,000; 78.9%). There was a significant increase in the ratio of SGA/FGA prescriptions over time (β = 0.376, 95% CI 0.277–0.464, P < 0.001). Individual FGAs were increasingly prescribed in areas of lower SES and the converse for SGAs except amisulpride. During the study period, a significantly larger proportion of total SGA prescriptions relative to total FGAs were made in areas of higher SES (β = 0.182, 95% CI 0.117–0.249, P < 0.001).
Conclusion
Prescriptions of antipsychotics continue to rise overall, with SGAs taking preference especially in areas of higher SES. The pattern of antipsychotic prescription favouring people in areas of lower social deprivation carries implications on inequalities even among sub-groups of people with mental disorders.


Similar content being viewed by others
References
Davis JM, Chen N, Glick ID (2003) A meta-analysis of the efficacy of second-generation antipsychotics. Arch Gen Psychiatry 60:553–564
Strejilevich SA, Palatnik A, Avila R, Bustin J, Cassone J, Figueroa S, Gimenez M, de Erausquin GA (2005) Lack of extrapyramidal side effects predicts quality of life in outpatients treated with clozapine or with typical antipsychotics. Psychiatry Res 133:277–280
Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, Samara M, Barbui Engel R, Geddes JR, Kissling W, Stapf MP, Lassig B, Salanti G, Davis JM (2013) Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet 382:951–962
Leucht S, Corves C, Arbeter D, Engel RR, Li C, David JM (2002) Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet 373:31–34
Chen VC, Liao YT, Lai TJ, Lane HY, Shao WJ, Dewey M, Lee CTC, Lu ML (2015) Survival analysis of the use of first and second generation antipsychotics among patients suffering from schizophrenia: a nationwide population-based cohort study. Schizophrenia Res 169:406–411
Martin D, Park J, Langan J, Connolly M, Smith D, Taylor M (2014) Socioeconomic status and prescribing for schizophrenia: analysis of 3200 cases from the Glasgow Psychosis Clinical Information System (PsyCIS). Psychiatric Bull 38:54–57
Marston L, Nazareth I, Petersen I, Walters K, Osborn DPJ (2014) Prescribing of antipsychotics in UK primary care: a cohort study. BMJ Open 4:e006135
Verdoux H, Tournier M, Begaud B (2010) Antipsychotic prescribing trends: a review of pharmaco-epidemiological studies. Acta Psychiatr Scand 121:4–10
Kaye JA, Bradbury BD, Jick H (2003) Changes in antipsychotic drug prescribing by general practitioners in the United Kingdom from 1991 to 2000: a population-based observational study. Br J Clin Pharmacol 56:569–575
de Hert M, Detraux J, van Winkel R, Yu W, Correll CU (2011) Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat Rev Endocrinol 18:114–126
Kiviniemi M, Suvisaari J, Koivumaa-Honkanen H, Hakkinen U, Isohanni M, Hakko H (2013) Antipsychotics and mortality in first-onset schizophrenia: prospective Finnish register study with 5-year follow-up. Schizophr Res 150:274–280
Wheeler A (2007) Sociodemographic, functional and clinical correlates in outpatients with schizophrenia: comparison with affective disorders. Aust N Z J Psychiatry 41:809–818
Corcoran C, Perrin M, Harlap S, Deutsch L, Fennig S, Manor O, Nahon D, Kimhy D, Malaspina D, Susser E (2009) Effect of socioeconomic status and parents’ education at birth on risk of schizophrenia in offspring. Soc Psychiatry Psychiatr Epidemiol 44:265–271
Sariaslan S, Fazel BM, D’Onofrio N, Långström H Larsson, Bergen SE, Kuja-Halkola R, Lichtenstein P (2016) Schizophrenia and subsequent neighbourhood deprivation: revisiting the social drift hypothesis using population, twin and molecular genetic data. Transl Psychiatry 6:e796
Goodman AB, Siegel C, Craig T, Lin SP (1983) The relationship between socioeconomic class and prevalence of schizophrenia, alcoholism, and affective disorders treated by inpatient care in a suburban area. Am J Psychiatry 140:166–170
Giacco D, Palumbo C, Strappelli N, Catapano F, Priebe S (2016) Social contacts and loneliness in people with psychotic and mood disorders. Compr Psychiatry 66:59–66
Eid L, Heim K, Doucette S, McCloskey S, Duffy A, Grof P (2013) Bipolar disorder and socioeconomic status: what is the nature of this relationship? Int J Bipolar Disord 1:9
Fitzgerald C, Hurst S (2017) Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics 18:19
Xue Q, Xoing X, Feng Y, Yao L, Chen S, Xiang L (2014) Socioeconomic factors influencing antipsychotic prescription for schizophrenia inpatients in China: a cross-sectional study. Int Clin Psychopharmacol 29:288–295
Ren XS, Kazis LE, Lee AF, Lee AF, Hamed A, Huang YH, Cunningham F, Miller DR (2002) Patient characteristics and prescription patterns of atypical antipsychotics among patients with schizophrenia. J Clin Pharm Therap 27:441–445
Franz M, Ranger J, Hanewals B, Gallhofer B, Lay B (2012) Influences on therapist’s decisions for neuroleptic treatment in schizophrenia: the role of characteristics of the patient and the physician. Pharmacopsychiatry 45:261–268
Hayes J, Prah P, Nazareth I, King M, Walters K, Petersen I, Osborn D (2011) Prescribing trends in bipolar disorder: cohort study in the United Kingdom THIN primary care database 1995–2009. PLoS One 6:e28725
Earwicker R (2007) Progress in tackling health inequality: a policymaker’s reflections. In: Dowler E, Spencer N (eds) Challenging health inequalities. From Acheson to “Choosing health”. Policy Press, Bristol, pp 17–30
Department for Communities and Local Government (2015) The English Indices of Deprivation 2015. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/465791/English_Indices_of_Deprivation_2015_-_Statistical_Release.pdf. Accessed 15 Jun 2019
McKinney W (2010) Data structures for statistical computing in python. In: Proceedings of the 9th Python in Science Conference, vol 445, pp 51–56
R Core Team (2013) R: A language and environment for statistical computing. In: R Foundation for Statistical Computing, Vienna, Austria
Joint Formulary Committee (2016) British National Formulary, 72nd edn. BMJ Group and Pharmaceutical Press, London
Office for National Statistics, England population mid-year estimates (2019) https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/timeseries/enpop/pop. Accessed 15 Jun 2019
Kirkbride JB, Errazuriz A, Croudace TJ, Morgan C, Jackson D, Boydell J, Murray RM, Jones PB (2012) Incidence of schizophrenia and other psychoses in England, 1950–2009: a systematic review and meta-Analyses. PLoS One 7(3):e31660
Ilyas S, Moncrieff J (2012) Trends in prescriptions and costs of drugs for mental disorders in England, 1998-2010. Br J Psychiatry 200:393–398
Prah P, Petersen I, Nazareth I, Walters K, Osborn D (2012) National changes in oral antipsychotic treatment for people with schizophrenia in primary care between 1998 and 2007 in the United Kingdom. Pharmacoepidemiol Drug Saf 21:161–169
Chinburapa Vijit, Larson Lon N, Brucks Merrie, JoLaine Draugalis J, Bootman Lyle, Puto Christopher P (1993) Physician prescribing decisions: the effects of situational involvement and task complexity on information acquisition and decision making. Soc Sci Med 36:1473–1482
Hull Sally A, Cornwell Jo, Harvey Charlotte, Eldridge Sandra, Bare Portia Omo (2001) Prescribing rates for psychotropic medication amongst east London general practices: low rates where Asian populations are greatest. Fam Prac 18:167–173
NHS England (2019) https://www.england.nhs.uk/allocations/. Accessed 15 Jun 2019
Leucht S, Pitschel-Walz G, Engel RR, Kissling W (2002) Amisulpride, an unusual “atypical” antipsychotic: a meta-analysis of randomized controlled trials. Am J Psychiatry 159:180–190
Barnes TR, Leeson VC, Paton C, Marston L, Davies L, Whittaker W, Osborn D, Kumar R, Keown P, Zafar R, Iqbal K, Singh V, Fridrich P, Fitzgerald Z, Bagalkote H, Haddad PM, Husni M, Amos T (2017) Amisulpride augmentation in clozapine-unresponsive schizophrenia (AMICUS): a double-blind, placebo-controlled, randomised trial of clinical effectiveness and cost-effectiveness. Health Technol Assess 2017:21. https://doi.org/10.3310/hta21490
García S, Martínez-Cengotitabengoa M, López-Zurbano S, Zorrilla I, López P, Vieta E, González-Pinto A (2016) Adherence to antipsychotic medication in bipolar sisorder and schizophrenic patients: a systematic review. J Clin Psychopharmacol 36:355–371
Townsend P, Phillimore P, Beattie A (1988) Health and Deprivation: Inequality and the North. Routledge, London
NHS Information Centre for Health and Social Care (2011) Data quality. (Prescription cost analysis). NHS Information Centre. Accessed 15 June 2019
Mordecai L, Reynolds C, Donaldson LJ, de Williams CA (2018) Patterns of regional variation of opioid prescribing in primary care in England: a retrospective observational study. Br J Gen Prac 8(668):e225–e233
Frangou S, Lewis M (2000) Atypical antipsychotics in ordinary clinical practice: a pharmaco-epidemiologic survey in a south London service. Eur Psychiatry 15:220–226
Donohue J, O’Malley AJ, Horvitz-Lennon M, Taub AL, Berndt ER, Huskamp HA (2014) Changes in physician antipsychotic prescribing preferences, 2002–2007. Psychiatr Serv 65:315–322
Thompson Coon J, Abbott R, Rogers M, Whear R, Pearson S, Lang I, Cartmell N, Stein K (2014) Interventions to reduce inappropriate prescribing of antipsychotic medications in people with dementia resident in care homes: a systematic review. J Am Med Dir Assoc 5:706–718
Funding
No specific funding was available for this study.
Author information
Authors and Affiliations
Contributions
KB and MG conceived the original idea for the study and collected, analysed and interpreted the data. KB wrote the original draft of the manuscript. MD contributed to data interpretation and later drafts of the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The author(s) declare that they have no conflict of interests
Ethics approval
Ethical approval was not required for the study as it is based on publicly available data sources and no human participants were involved.
Rights and permissions
About this article
Cite this article
Buhagiar, K., Ghafouri, M. & Dey, M. Oral antipsychotic prescribing and association with neighbourhood-level socioeconomic status: analysis of time trend of routine primary care data in England, 2011–2016. Soc Psychiatry Psychiatr Epidemiol 55, 165–173 (2020). https://doi.org/10.1007/s00127-019-01793-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-019-01793-9