Abstract
Purpose
To describe the rates, types and comorbidity of emotional and behavioural disorders among perinatally HIV-infected children and adolescents attending care at five HIV youth clinics in Central and Southwestern Uganda.
Methods
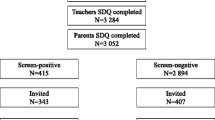
1339 CA-HIV attending care at HIV youth clinics in Uganda were interviewed using the DSM-5-based Child and Adolescent Symptom Inventory-5 (CASI-5; caregiver reported) and the Youth Inventory-4R (YI-4R; youth reported). Prevalence, risk factors and comorbidity for psychiatric disorders were estimated using logistic regression models.
Results
According to caregiver or youth report, the prevalence of ‘any DSM-5 psychiatric disorder’ was 17.4% (95% CI 15.4–19.5%), while that of ‘any behavioural disorder’ was 9.6% (95% CI 8.1–11.2%) and that of ‘any emotional disorder’ was 11.5% (95% CI 9.9–13.3%). The most prevalent behavioural disorder was attention deficit hyperactivity disorder (5.3%), while the most prevalent emotional disorder was separation anxiety disorder (4.6%). The statistically significant risk factors were: for behavioural disorders, sex (more among males than females) and age group (more among adolescents than among children); for emotional disorders, age group (more among adolescents than among children) and the caregiver’s highest educational attainment (more among CA-HIV with caregivers with secondary education and higher, than among CA-HIV with caregivers with no formal education or only primary level education). About a quarter (24.5%) of CA-HIV with at least one emotional disorder and about a third (33.5%) of the CA-HIV with at least one behavioural disorder had a comorbid psychiatric disorder.
Conclusion
There was a considerable burden of psychiatric disorders among CA-HIV that spanned a broad spectrum and showed considerable comorbidity.
Similar content being viewed by others
References
UNAIDS (2014) The Gap Report. http://files.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2014/UNAIDS_Gap_report_en.pdf. Accessed 15 Feb 2017
Mellins CA, Malee KM (2013) Understanding the mental health of youth living with perinatal HIV infection: lessons learned and current challenges. J Int AIDS Soc 16:18593
Mellins CA, Elkington KS, Leu CS, Santamaria EK, Dolezal C, Wiznia A, Bamji M, Mckay MM, Abrams EJ (2012) Prevalence and change in psychiatric disorders among perinatally HIV-infected and HIV-exposed youth. AIDS Care 24(8):953–962
Gadow KD, Chernoff M, Williams PL, Brouwers P, Morse E, Heston J, Hodge J, Di Poalo V, Deygoo NS, Nachman S (2010) Co-occuring psychiatric symptoms in children perinatally infected with HIV and peer comparison sample. J Dev Behav Pediatr 31(2):116–128
Nachman S, Chernoff M, Williams P, Hodge J, Heston J, Gadow KD (2012) Human immunodeficiency virus disease severity, psychiatric symptoms, and functional outcomes in perinatally infected youth. Arch Pediatr Adolesc Med 166(6):528–535
Vreeman RC, Scanlon ML, Marete I, Mwangi A, Inui TS, McAteer CI, Nyandiko WM (2015) Characteristics of HIV-infected adolescents enrolled in a disclosure intervention trial in western Kenya. AIDS Care 27(Suppl 1):6–17
Mavhu W, Berwick J, Chirawu P, Makamba M, Copas A, Dirawo J, Willis N, Araya R, Abas MA, Corbett EL, Mungofa S, Laver SM, Cowan FM (2013) Enhancing psychosocial support for HIV positive adolescents in Harare, Zimbabwe. PLoS One 8(7):e70254.9
Musisi S, Kinyanda E (2009) Emotional and behavioural disorders in HIV seropositive adolescents in urban Uganda. East Afr Med J 86(1):16–24
Kamau JW, Kuria W, Mathai M, Atwoli L, Kangethe R (2012) Psychiatric morbidity among HIV-infected children and adolescents in a resource-poor Kenyan urban community. AIDS Care 24(7):836–842
Chida Y, Vedhara K (2009) Adverse psychosocial factors predict poorer prognosis in HIV disease: a meta-analytic review of prospective investigations. Brain Behav Immun 23(4):434–445
Ironson G, O’Cleirigh C, Fletcher MA, Laurenceau JP, Balbin E, Klimas N (2005) Psychosocial factors predict CD4 and viral load change in men and women with human immunodeficiency virus in the era of highly active antiretroviral treatment. Psychosom Med 67(6):1013–1021
Kinyanda E, Levin J, Nakasujja N, Birabwa H, Nakku J, Mpango R, Grosskurth H, Seedat S, Araya R, Shahmanesh M, Patel V (2018) Major depressive disorder: longitudinal analysis of impact on clinical and behavioural outcomes in Uganda. J Acquir Immune Defic Syndr 78(2):136–143
Springer SA, Dushaj A, Azar MM (2012) The impact of DSM-IV mental disorders on adherence to combination antiretroviral therapy among adult persons living with HIV/AIDS: a systematic review. AIDS Behav 16(8):21119–21143
Mpango RS, Kinyanda E, Rukundo GZ, Levin J, Gadow KD, Patel V (2017) Prevalence and correlates for ADHD and relation with social and academic functioning among children and adolescents with HIV/AIDS in Uganda. BMC Psychiatry 17(1):336
Bhatia R, Hartman C, Kallen MA, Graham J, Giordano TP (2011) Persons newly diagnosed with HIV infection are at high risk for depression and poor linkage to care: results from the Steps Study. AIDS Behav 15(6):1161–1170
Remien RH, Mellins CA (2007) Long-term psychosocial challenges for people living with HIV: let’s not forget the individual in our global response to the pandemic. AIDS 21(Suppl 5):S55–S63.14
Abas M, Ali GC, Nakimuli-Mpungu E, Chibanda D (2014) Depression in people living with HIV in sub-Saharan Africa: time to act. Trop Med Int Health 19(12):1392–1396
Kigozi FN, Ssebunnya J (2009) Integration of mental health into primary health care in Uganda: opportunities and challenges. Ment Health Fam Med 6(1):37–42
Wagner GJ, Ngo V, Glick P, Obuku EA, Musisi S, Akena (2014) INtegration of DEPression Treatment into HIV Care in Uganda (INDEPTH-Uganda): study protocol for a randomized controlled trial. Trials 15:248
World Health Organisation (2015) Treat all people living with HIV, offer antiretrovirals as additional prevention choice for people at “substantial” risk. http://www.who.int/mediacentre/news/releases/2015/hiv-treat-all-recommendation/en/. Accessed 20 July 2017
Ministry of Health, Uganda (2016) Consolidated guidelines for prevention and treatment of HIV in Uganda. HIV in Uganda. https://elearning.idi.co.ug/pluginfile.php/83/mod_page/content/57/CONSOLIDATED%20GUIDELINES%20FOR%20PREVENTION%20AND%20TREATMENT%20OF%20HIV%20IN%20UGANDA.PDF Accessed 11 May 2018
Ministry of Health, Community Development, Gender, Elderly and Children, Tanzania (2017) National guidelines for the management of HIV and AIDS. http://www.nacp.go.tz/site/download/NATIONAL_DECEMBER_2017.pdf. Accessed 11 May 2018
Gadow KD, Sprafkin J (2013) Child and Adolescent Symptom Inventory-5. Checkmate Plus. 2013. Stony Brook. https://www.checkmateplus.com/product/casi5.htm. Accessed 20 Feb 2019
Mpango RS, Kinyanda E, Rukundo GZ, Gadow KD, Patel V (2017) Cross-cultural adaptation of the Child and Adolescent Symptom Inventory-5 (CASI-5) for use in central and south-western Uganda: the CHAKA project. Trop Doct 47(4):347–354
Gadow KD, Sprafkin J (1999) Youth’s Inventory-4 (YI-4). https://www.checkmateplus.com/product/yi-4.htm. Accessed 20 Feb 2019
Kinyanda E, Waswa L, Baisley K, Maher D (2011) Prevalence of severe mental distress and its correlates in a population-based study in rural south-west Uganda. BMC Psychiatry 11:97
Pallant J (2007) Designing a study. In: SPSS survival manual: a step by step guide to data analysis using SPSS for Windows, 3rd edn. Open University Press, London, pp 3–10
Mellins CA, Brackis-Cott E, Leu CS, Elkington KS, Dolezal C, Wiznia A, McKay M, Bamji M, Abrams EJ (2009) Rates and types of psychiatric disorders in perinatally human immunodeficiency virus-infected youth and seroreverters. J Child Psychol Psychiatry 50(9):1131–1138
Ozbay F, Johnson DC, Dimoulas E, Morgan CA, Charney D, Southwick S (2007) Social support and resilience to stress. Psychiatry (Edgmont) 4(5):35–40
Osafo J, Knizek BL, Mugisha J, Kinyanda E (2017) The experiences of caregivers of children living with HIV and AIDS in Uganda: a qualitative Study. Glob Health 13(1):72
Kinyanda E, Weiss HA, Levin J, Nakasujja N, Birabwa H, Nakku J, Mpango R, Grosskurth H, Seedat S, Araya R, Patel V (2017) Incidence and persistence of major depressive disorder among people living with HIV in Uganda. AIDS Behav 21:1641
Patel V, Kirkwood BR, Pednekar S, Weiss H, Mabey D (2006) Risk factors for common mental disorders in women. Population-based longitudinal study. Br J Psychiatry 189:547–555
Helmchen H, Linden M (2000) Subthreshold disorders in psychiatry: clinical reality, methodological artifact, and the double-threshold problem. Compr Psychiatry 41(2 Suppl 1):1–7
Acknowledgements
We would like to acknowledge the work and support provided by the staff of the Mental Health Project at the MRC/UVRI & LSHTM Uganda Research Unit. We would also like to acknowledge the support and corporation of children/adolescents, caregivers and management of The AIDS Support Organisation (TASO) clinic (Masaka), Kitovu Mobile AIDS organisation (Masaka), The Uganda Cares clinic (Masaka), Joint Clinical Research Centre clinic (Kampala) and Nsambya Home care Department (Kampala). This work was supported by a Medical Research Council / Department for International Development—African Leadership Award to Eugene Kinyanda, Number MR/L004623/1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest to declare.
Rights and permissions
About this article
Cite this article
Kinyanda, E., Salisbury, T.T., Levin, J. et al. Rates, types and co-occurrence of emotional and behavioural disorders among perinatally HIV-infected youth in Uganda: the CHAKA study. Soc Psychiatry Psychiatr Epidemiol 54, 415–425 (2019). https://doi.org/10.1007/s00127-019-01675-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-019-01675-0