Abstract
Purpose
The purpose of the study is to identify early vulnerabilities for psychiatric disorders among Brazilian elementary school children, controlling for familial and community adversities.
Methods
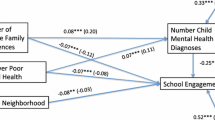
This is a cross-sectional study examining the association between child psychiatric disorders and potential early vulnerabilities (disability, low intellectual quotient, and negative dimensions of the temperament trait self-directedness (low resourcefulness, low purposefulness, low enlightened second nature), controlling for the potential confounders: familial and community adversities. Sample: Four probabilistic samples of second-to-sixth grade students from public schools in four towns from different Brazilian regions (N = 1620). The following instruments were applied: the K-SADS-PL (to assess child/adolescent psychiatric disorders); the Ten-Question Screen (to measure child disability); three structured questions used as proxy of self-directedness; and the reduced version of the WISC-III to measure IQ. To evaluate familial/community adversities: Self-Report Questionnaire—SRQ-20 (to assess maternal/primary caretaker anxiety/depression); questions derived from structured questionnaires (to measure child abuse, marital physical violence, neighborhood violence); Brazilian Association of Research Companies questionnaire (to evaluate poverty/socioeconomic status). Trained psychologists interviewed mothers/primary caretakers and evaluated children/adolescents individually.
Results
A final logistic regression model showed that children/adolescents with low resourcefulness, low purposefulness, low enlightened second nature, lower IQ and disability were more likely to present any child psychiatric disorders.
Conclusion
Early vulnerabilities such as low IQ, presence of disability, and dimensions of temperament were associated with psychiatric disorders among Brazilian elementary school children, after controlling for familial and ecological confounders. These early vulnerabilities should be considered in mental health prevention/intervention programs in low-middle-income countries like Brazil.
Similar content being viewed by others
References
Goodman A, Joyce R, Smith JP (2011) The long shadow cast by childhood physical and mental problems on adult life. Proc Natl Acad Sci USA 108(15):6032–6037
Valdez CR, Lambert SF, Ialongo NS (2011) Identifying patterns of early risk for mental health and academic problems in adolescence: a longitudinal study of urban youth. Child Psychiatry Hum Dev 42(5):521–538
Pihlakoski L, Sourander A, Aromaa M, Rautava P, Helenius H, Sillanpää M (2006) The continuity of psychopathology from early childhood to preadolescence: a prospective cohort study of 3–12-year-old children. Eur Child Adolesc Psychiatry 15(7):409–417
Althoff RR, Verhulst FC, Rettew DC, Hudziak JJ, van der Ende J (2010) Adult outcomes of childhood dysregulation: a 14-year follow-up study. J Am Acad Child Adolesc Psychiatry 49(11):1105–1116
Signoretta S, Maremmani I, Liguori A, Perugi G, Akiskal HS (2005) Affective temperament traits measured by TEMPS-I and emotional-behavioral problems in clinically-well children, adolescents, and young adults. J Affect Disord 85(1–2):169–180
Kushner SC, Tackett JL, Bagby RM (2012) The structure of internalizing disorders in middle childhood and evidence for personality correlates. J Psychopathol Behav Assess 34(1):22–34. https://doi.org/10.1007/s10862-011-9263-4
Dougherty LR, Tolep MR, Bufferd SJ, Olino TM, Dyson M, Traditi J et al (2013) Preschool anxiety disorders: comprehensive assessment of clinical, demographic, temperamental, familial, and life stress correlates. J Clin Child Adolesc Psychol 42(5):577–589. https://doi.org/10.1080/15374416.2012.759225
Bagner DM, Pettit JW, Lewinsohn PM, Seeley JR (2010) Effect of maternal depression on child behavior: a sensitive period? J Am Acad Child Adolesc Psychiatry 49(7):699–707
Ramchandani PG, Stein A, O’connor TG, Heron J, Murray L, Evans J (2008) Depression in men in the postnatal period and later child psychopathology: a population cohort study. J Am Acad Child Adolesc Psychiatry 47(4):390–398
Battaglia M, Przybeck TR, Bellodi L, Cloninger CR (1996) Temperament dimensions explain the comorbidity of psychiatric disorders. Compr Psychiatry 37(4):292–298
Fassino S, Amianto F, Sobrero C, Abbate Daga G (2013) Does it exist a personality core of mental illness? A systematic review on core psychobiological personality traits in mental disorders. Panminerva Med 55(4):397–413
Miettunen J, Raevuori A (2012) A meta-analysis of temperament in axis I psychiatric disorders. Compr Psychiatry 53(2):152–166
Loftus ST, Garno JL, Jaeger J, Malhotra AK (2008) Temperament and character dimensions in bipolar I disorder: a comparison to healthy controls. J Psychiatr Res 42(13):1131–1136
Siddiqi SH, Chockalingam R, Cloninger CR, Lenze EJ, Cristancho P (2016) Use of the temperament and character inventory to predict response to repetitive transcranial magnetic stimulation for major depression. J Psychiatr Pract 22(3):193–202
Cloninger CR, Svrakic DM, Przybeck TR (1993) A psychobiological model of temperament and character. Arch Gen Psychiatry 50(12):975–990
Celikel FC, Kose S, Cumurcu BE, Erkorkmaz U, Sayar K, Borckardt JJ et al (2009) Cloninger’s temperament and character dimensions of personality in patients with major depressive disorder. Compr Psychiatry 50(6):556–561
Koenen KC, Moffitt TE, Roberts AL, Martin LT, Kubzansky L, Harrington H et al (2009) Childhood IQ and adult mental disorders: a test of the cognitive reserve hypothesis. Am J Psychiatry 166(1):50–57. https://doi.org/10.1176/appi.ajp.2008.08030343
Goodman A, Fleitlich-Bilyk B, Patel VI, Goodman R (2007) Child, family, school and community risk factors for poor mental health in Brazilian schoolchildren. J Am Acad Child Adolesc Psychiatry 46(4):448–456
Zammit S, Allebeck P, David AS, Dalman C, Hemmingsson T, Lundberg I et al (2004) A longitudinal study of premorbid IQ score and risk of developing schizophrenia, bipolar disorder, severe depression, and other nonaffective psychoses. Arch Gen Psychiatry 61(4):354. https://doi.org/10.1001/archpsyc.61.4.354
Cooper S-A, Smileye E, Morrison J, Williamson A, Allan L (2007) Mental ill-health in adults with intellectual disabilities: prevalence and associated factors. Br J Psychiatry 190(1):27–35. https://doi.org/10.1192/bjp.bp.106.022483
Einfeld SL, Ellis LA, Emerson E (2011) Comorbidity of intellectual disability and mental disorder in children and adolescents: a systematic review. J Intellect Dev Disabil 36(2):137–143. https://doi.org/10.1080/13668250.2011.572548
Imran N, Azeem MW, Sattar A, Bhatti MR (2015) Frequency of ICD-10 psychiatric diagnosis in children with intellectual disability in Lahore, Pakistan & caregivers perspective. Pakistan J Med Sci 31(2):285–289
United Nation—UN in collaboration with Leonard Cheshire Disability and Inclusive Development Centre at University College London & United Nations Children’s Fund (UNICEF) (2014) Convention on the Rights of Persons with Disabilities and Optional Protocol from United Nation (UN), p 35. Available from: http://www.un.org/disabilities/documents/convention/convoptprot-e.pdf
Gottlieb C, Maenner MJ, Cappa C, Durkin MS (2009) Child disability screening, nutrition, and early learning in 18 countries with low and middle incomes: data from the third round of UNICEF’s Multiple Indicator Cluster Survey (2005–06). Lancet 374(9704):1831–1839
Maulik PK, Darmstadt GL (2007) Childhood disability in low- and middle-income countries: overview of screening, prevention, services, legislation, and epidemiology. Pediatrics 120(Suppl 1):S1–S55
Lowenthal R, Zaqueu L, Rohde LA, Mari J, Paula CS (2014) Developmental disability in schoolchildren from four Brazilian regions. Rev Bras Psiquiatr 36(3):273–273
Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O et al (2011) Child and adolescent mental health worldwide: evidence for action. Lancet 378(9801):1515–1525
Paula CS, Lauridsen-Ribeiro E, Wissow L, Bordin IS, Evans-Lacko S (2012) How to improve the mental health care of children and adolescents in Brazil: actions needed in the public sector. Rev Bras Psiquiatr 34(3):334–341
Instituto Brasileiro de Geografia e Estatística., IBGE (2010) Séries historicas e estatísticas. http://seriesestatisticas.ibge.gov.br/series.aspx?no=10&op=0&vcodigo=CD97&t=numero-municipios-censo-demografico-classes-tamanho
Presidência da Republica do Brasil (1996) Diretrizes e Bases da Educação. Lei no 9.394, de 20 de dezembro de 1996. http://www.planalto.gov.br/ccivil_03/leis/l9394.htm
Instituto Brasileiro de Geografia e Estatística., IBGE. Cidades@. 2013. http://www.ibge.gov.br/cidadesat
Paula CS, Bordin IS, Mari JJ, Velasque L, Rohde L, Coutinho ESF (2014) The mental health care gap among children and adolescents: data from an epidemiological survey from four Brazilian regions. Takei N, editor. PLoS One 9(2):e88241. https://doi.org/10.1371/journal.pone.0088241
Kaufman J, Birmaher B, Brent D, Rao U, Flynn C et al (1997) Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36(7):980–988
Brasil HH, Bordin IA (2010) Convergent validity of K-SADS-PL by comparison with CBCL in a Portuguese speaking outpatient population. BMC Psychiatry 10(1):83
Urgesi C, Romanò M, Fornasari L, Brambilla P, Fabbro F (2012) Investigating the development of temperament and character in school-aged children using a self-report measure. Compr Psychiatry 53(6):875–883
Kose SA (2003) Psychobiological model of temperament and character: TCI. Yeni Symp 41(2):86–97
Cruz M (2005) WISC III: Escala de Inteligência Wechsler para crianças: Manual. Avaliação Psicológica 4(2):199–201
Figueiredo V (2002) WISC-III: Escala de Inteligência Weschler para crianças—adaptação brasileira da 3° edição. Casa do Psicólogo, São Paulo, p 50
Furgueson C, Greenstein D, McGuffin P, Furgueson C, Greenstein D, McGuffin PPMP (1999) Efficacy of the WISC-III short form for children diagnosed with conduct and oppositional defiant disorders. Arch Clin Neuropsychol 14:6–7
Mello CB, Argollo N, Shayer BPM, Abreu N, Godinho KT, Durán P, Vargem F, Muszkat M, Miranda MC (2011) Versão abreviada do WISC-III: correlação entre QI estimado e QI total em crianças brasileiras. Psicol Teor e Pesqui 27:149–155
Oliveira GE, Magalhães LC, Salmela LFT (2011) Relationship between very low birth weight, environmental factors, and motor and cognitive development of children of 5 and 6 years old. Rev Bras Fisioter 15(2):138–145
Silverstein AB (1985) Two- and four-subtest short forms of the WAIS-R: a closer look at validity and reliability. J Clin Psychol 41(1):95–97
Veenstra R, Lindenberg S, Oldehinkel AJ, De Winter AF, Verhulst FC, Ormel J (2008) Prosocial and antisocial behavior in preadolescence: teachers’ and parents’ perceptions of the behavior of girls and boys. Int J Behav Dev 32(3):243–251. https://doi.org/10.1177/0165025408089274
Silverstein AB (1990) Short forms of individual intelligence tests. Psychol Assess 2(1):3–11. https://doi.org/10.1037/1040-3590.2.1.3
Durkin MS, Hasan ZM, Hasan KZ (1995) The ten questions screen for childhood disabilities: its uses and limitations in Pakistan. J Epidemiol Community Health 49(4):431–436
Stein Z, Durkin M, Belmont L (1986) “Serious” mental retardation in developing countries: an epidemiologic approach. Ann N Y Acad Sci 477:8–21
Durkin MS, Davidson LL, Desai P, Hasan ZM, Khan N, Shrout PE et al (1994) Validity of the ten questions screened for childhood disability: results from population-based studies in Bangladesh, Jamaica, and Pakistan. Epidemiology 5(3):283–289
Bordin IAS, Duarte CS, Peres CA, Nascimento R, Curto BM, Paula CS (2009) Severe physical punishment: risk of mental health problems for poor urban children in Brazil. Bull World Health Organ 87(5):336–344
Fleitlich B, Goodman R (2001) Social factors associated with child mental health problems in Brazil: cross sectional survey Skin cancer surveillance in renal transplant recipients: questionnaire survey of current UK practice. Br Med J 323(7313):599–600
Beusenberg M, Orley J (1994) A users guide to the self reporting questionnaire—SRQ, 1st edn. World Health Organization, Washington, DC
Espinola-Nadurille M, Vargas Huicochea I, Raviola G, Ramirez-Bermudez J, Kutcher S (2010) Mental health care reforms in Latin America: child and adolescent mental health services in Mexico. Psychiatr Serv Washingt DC 61(5):443–445
Mari J, Williams P (1986) A validity study of a psychiatric screening questionnaire (SRQ-20) in primary care in the city of Sao Paulo. Rev Bras Psiquiatr 148:23–26
Associaçao Brasileira de Pesquisa de Mercado A. Critério de classificação econômica Brasil. 2007. http://www.abep.org/codigosguias/ABEP_CCEB.pdf
Mickey RM, Greenland S (1989) The impact of confounder selection criteria on effect estimation. Am J Epidemiol 129(1):125–137
Paula CS, Coutinho ES, Mari JJ, Rohde L, Miguel EC, Bordin I (2015) Prevalence of psychiatric disorders among children and adolescents from four Brazilian regions. Rev Bras Psiquiatr 37(2):178–179
Fortes IS, Paula CS, Oliveira MC, Bordin IA, Mari JJ, Rohde LA (2016) A cross—sectional study to assess the prevalence of DSM—5 specific learning disorders in representative school samples from the second to sixth grade in Brazil. Eur Child Adolesc Psychiatry 25(2):195–207
Polanczyk GV, Salum G, Sugaya LS, Caye A, Rohde L (2015) Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry 56(3):345–365. https://doi.org/10.1111/jcpp.12381
Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, Koretz DS (2010) Prevalence and treatment of mental disorders among US children in the 2001–2004 NHANES. Pediatrics 125(1):75–81
van der Heijden PT, Rossi GMP, van der Veld WM, Derksen JJL, Egger JIM (2013) Personality and psychopathology: higher order relations between the five factor model of personality and the MMPI-2 Restructured Form. J Res Pers 47(5):572–579. https://doi.org/10.1016/j.jrp.2013.05.001
Krueger RF, Tackett JL (2003) Personality, psychopathology: working toward the bigger picture. J Pers Disord 17(2):109–128. https://doi.org/10.1521/pedi.17.2.109.23986
Cho S-C, Hwang J-W, Lyoo I-K, Yoo H-J, Kin B-N, Kim J-W (2008) Patterns of temperament and character in a clinical sample of Korean children with attention-deficit hyperactivity disorder. Psychiatry Clin Neurosci 62(2):160–166. https://doi.org/10.1111/j.1440-1819.2008.01749.x
Zappitelli MC, Bordin IA, Hatch JP, Caetano SC, Zunta-Soares G, Olvera RL et al (2013) Temperament and character traits in children and adolescents with major depressive disorder: a case–control study. Compr Psychiatry 54(4):346–353. https://doi.org/10.1016/j.comppsych.2012.10.009
Hatch JP, Ph D, Hunter K, Nicoletti M, Sc M, Pliszka SR et al (2009) Assessment of personality dimensions in children and adolescents with bipolar disorder using the junior temperament and character inventory. J Child Adoles Psychopharmacol 19(1):13–21
Rajput S, Hassiotis A, Richards M, Hatch SL, Stewart R (2011) Associations between IQ and common mental disorders: the 2000 British National Survey of Psychiatric Morbidity. Eur Psychiatry 26(6):390–395. https://doi.org/10.1016/j.eurpsy.2010.07.002
Batty GD (2005) Childhood IQ in relation to later psychiatric disorder: evidence from a Danish birth cohort study. Br J Psychiatry 187(2):180–181. https://doi.org/10.1192/bjp.187.2.180
Castaneda AE, Tuulio-Henriksson A, Marttunen M, Suvisaari J, Lönnqvist J (2008) A review on cognitive impairments in depressive and anxiety disorders with a focus on young adults. J Affect Disord 106(1–2):1–27
Hatch SL, Jones PB, Kuh D, Hardy R, Wadsworth MEJ, Richards M (2007) Childhood cognitive ability and adult mental health in the British 1946 birth cohort. Soc Sci Med 64(11):2285–2296
Hoffmann MS, Leibenluft E, Stringaris A, Laporte PP, Pan PM, Gadelha A et al (2016) Positive attributes buffer the negative associations between low intelligence and high psychopathology with educational outcomes. J Am Acad Child Adolesc Psychiatry 55(1):47–53
Cederblad M, Dahlin L, Hagnell O, Hansson K (1995) Intelligence and temperament as protective factors for mental health. A cross-sectional and prospective epidemiological study. Eur Arch Psychiatry Clin Neurosci 245(1):11–19
Costello EJ, Maughan B (2015) Annual research review: optimal outcomes of child and adolescent mental illness. J Child Psychol Psychiatry 56(3):324–341. https://doi.org/10.1111/jcpp.12371
David AS, Zammit S, Lewis G, Dalman C, Allebeck P (2008) Impairments in cognition across the spectrum of psychiatric disorders: evidence from a swedish conscript cohort. Schizophr Bull 34(6):1035–1041. https://doi.org/10.1093/schbul/sbn028
Barnett JH, Salmond CH, Jones PB, Sahakian BJ (2006) Cognitive reserve in neuropsychiatry. Psychol Med 36(8):1053
Siebald C, Khandaker GM, Zammit S, Lewis G, Jones PB (2016) Association between childhood psychiatric disorders and psychotic experiences in adolescence: a population-based longitudinal study. Compr Psychiatry 69:45–52. https://doi.org/10.1016/j.comppsych.2016.05.004
Einfeld SL, Piccinin AM, Mackinnon A, Hofer SM, Taffe J, Gray KM et al (2006) Psychopathology in young people with intellectual disability. JAMA 296(16):1981
Ervin DA, Williams A, Merrick J (2014) Primary care: mental and behavioral health and persons with intellectual and developmental disabilities. Front Public Heal 2:76
Kok L, van der Waa A, Klip H, Staal W (2016) The effectiveness of psychosocial interventions for children with a psychiatric disorder and mild intellectual disability to borderline intellectual functioning: a systematic literature review and meta-analysis. Clin Child Psychol Psychiatry 21(1):156–171. https://doi.org/10.1177/1359104514567579
Acknowledgements
This study was funded by the State of São Paulo Funding Agency—FAPESP “INPD—Psiquiatria do Desenvolvimento para Infância e Adolescência” Instituto Nacional de Ciência e Tecnologia (INCT). Grant Number: [2008/57896-8], and by the National Research Council—CNPQ,—“Instituto Nacional de Ciência e Tecnologia de Psiquiatria do Desenvolvimento para Infância e Adolescência” Sigla: INPD—Edital nº 15/2008. Grant number [573974/2008]. CSP, JJM, ECM, LAR and ESFC are researchers from the National Research Council (CNPQ).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The 7th author (LAR) has been a member of the speakers’ bureau/advisory board and/or acted as a consultant for Eli-Lilly, Janssen-Cilag, Medice, Novartis, and Shire in the last 3 years. He receives authorship royalties from Oxford Press and ArtMed. The ADHD and Juvenile Bipolar Disorder Outpatient Programs chaired by him received unrestricted educational and research support from the following pharmaceutical companies in the last 3 years: Eli-Lilly, Janssen-Cilag, Novartis, and Shire. He also receives research support from Brazilian governmental institutions (CNPq, FAPERGS, HCPA, and CAPES). On behalf of the other authors, the corresponding author states that there is no conflict of interest. All authors declare that the submitted work has not been published before (neither in English nor in any other language) and that the work is not under consideration for publication elsewhere. A single study is not split up into several parts to increase the quantity of submissions and submitted to various journals or to one journal over time (e.g., “salami-publishing”). No data have been fabricated or manipulated to support our conclusions. No data, text, or theories by others are presented as if they were the author’s own (“plagiarism”). All authors gave consent to submit this manuscript before the submission and all eight authors have contributed sufficiently to the scientific work and therefore share collective responsibility and accountability for the results. The dataset and any additional data related to this manuscript will be provided by the first author upon request.
Ethical standards
All procedures performed in this study involving human participants were in accordance with the ethical standards of the University of São Paulo institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Paula, C.S., Mari, J.J., Bordin, I.A.S. et al. Early vulnerabilities for psychiatric disorders in elementary schoolchildren from four Brazilian regions. Soc Psychiatry Psychiatr Epidemiol 53, 477–486 (2018). https://doi.org/10.1007/s00127-018-1503-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-018-1503-4