Abstract
Aims/hypothesis
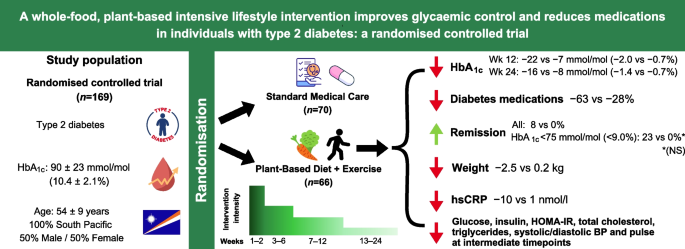
We conducted the largest and longest clinical trial comparing a whole-food, plant-based intervention with standard medical care (SMC) in individuals with type 2 diabetes.
Methods
We randomised (parallel-arm; computerised 1:1 randomisation ratio) 169 adults aged 18–75 years with type 2 diabetes in the Marshall Islands to an intensive whole-food, plant-based intervention with moderate exercise (PB+Ex) or SMC for 24 weeks. The PB+Ex intervention included 12 weeks of meals, exercise sessions and group classes. Primary outcomes were glycaemic control (HbA1c, glucose, insulin and HOMA-IR) and glucose-lowering medication use. Secondary outcomes included lipids, blood pressure, heart rate and C-reactive protein. Only lab analysts were blinded.
Results
Compared with SMC (n=90 randomised; n=70 analysed), the PB+Ex (n=79 randomised; n=66 analysed) intervention decreased HbA1c by an additional 14 mmol/mol (1.3%) at week 12 (−22 vs −7 mmol/mol [−2.0% vs −0.7%]; p<0.0001) and 8 mmol/mol (0.7%) at week 24 (−16 vs −8 mmol/mol [−1.4% vs −0.7%]; p=0.01). Concomitantly, 63% of medicated PB+Ex participants reduced their glucose-lowering medications (vs 24%; p=0.006), and 23% of PB+Ex participants with a baseline HbA1c <75 mmol/mol (<9%) achieved remission. Additionally, the PB+Ex intervention reduced weight (−2.7 kg; p<0.0001), C-reactive protein (−11 nmol/l; p=0.005) and cardiovascular medication use compared with SMC. At intermediate timepoints, it improved glucose, insulin, HOMA-IR, cholesterol, triglycerides and heart rate, but not at week 24.
Conclusions/interpretation
A whole-food, plant-based lifestyle intervention was more effective for improving glycaemic control than SMC. It also reduced the need for diabetes and cardiovascular medications and induced diabetes remission in some participants. Therefore, it is an effective, evidence-based lifestyle option for individuals with type 2 diabetes.
Trial registration
ClinicalTrials.gov NCT03862963
Funding
This research was funded by the Department of the Army (W81XWH-05-1-0547). CJH received support through a National Institutes of Health Predoctoral T32 Obesity Fellowship (T32 HL105349).
Graphical Abstract
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Diabetes is a pressing global health issue, affecting 10.5% of adults worldwide [1]. Although the causes of type 2 diabetes are complex, diet is a leading risk factor. Data from the Global Burden of Disease study suggest that a poor diet (low in vegetables, fruit, whole grains and fibre, and high in sugar-sweetened beverages, processed meat and red meat) is the second leading risk factor for diabetes, behind only a high BMI [2].
Increasingly, data suggest that a healthy diet can not only prevent type 2 diabetes but may also treat and reverse it. The Diabetes Remission Clinical Trial (DiRECT) found that a diet very low in energy (very-low-calorie diet [VLCD]) decreased HbA1c by 10 mmol/mol (0.9%), and 46% of participants with early-stage type 2 diabetes went into remission vs only 4% receiving standard care [3]. However, VLCDs fail to improve HbA1c in up to 40% of individuals, they are difficult to adhere to and only a minority of individuals are willing to try them [3,4,5]. Moreover, VLCDs pose several health risks, including headaches, dizziness, muscle cramps and bone loss [3].
Therefore, improving diet quality may be a better approach for treating type 2 diabetes. Of these approaches, low-carbohydrate diets, particularly ketogenic diets, are the most well-studied. Clinical trials suggest ketogenic diets lower HbA1c [6], reduce diabetes medications [6] and induce diabetes remission in some individuals [7]. However, low-carbohydrate diets are associated with increased mortality risk [8] and can actually impair glucose tolerance [9,10,11] and increase cholesterol and inflammation [11, 12].
An alternative, potentially more promising, approach is whole-food, plant-based (WFPB) diets, which are predominated by whole foods such as vegetables, fruits, legumes, whole grains, nuts and seeds. WFPB diets include not only vegetarian and vegan diets but also other plant-predominant diets that incorporate meat and seafood. Clinical trials in adults with type 2 diabetes have found that WFPB diets lower HbA1c [13,14,15], reduce the need for diabetes medications [16,17,18,19,20] and allow some individuals to wean off all medications [16, 18, 19]. For example, one small study found that 55% of individuals with insulin-dependent type 2 diabetes no longer needed exogenous insulin after only 16 days on a WFPB diet [19]. In addition, WFPB diets can reduce body weight without deliberate energy restriction [21, 22], have fewer side effects than VLCDs and ketogenic diets and may also have better adherence and acceptability [23, 24].
Although promising, most studies examining WFPB diets and diabetes are small and short-term. Thus, we conducted the largest and longest randomised controlled trial to compare a WFPB intervention vs standard medical care (SMC) in participants with type 2 diabetes. We conducted the clinical trial in the Republic of the Marshall Islands (RMI), which has the seventh-highest diabetes prevalence globally [25]. The country’s high prevalence has been partially attributed to its increased reliance on imported foods, including white rice, refined flour, sugar-sweetened beverages and canned meats [26,27,28,29,30,31], which provides an excellent milieu to test whether improving diet quality can treat type 2 diabetes. To mirror other intensive lifestyle interventions, we paired a WFPB diet with moderate exercise and hypothesised that the combination would be more effective than SMC for improving glycaemic control and cardiovascular health and would reduce the need for glucose-lowering medications.
Methods
Study design
We conducted a 24 week parallel-arm, randomised controlled trial comparing a whole-food, plant-based intervention with moderate exercise (PB+Ex) with SMC in adults with type 2 diabetes. The study was approved by the institutional review board at Loma Linda University (protocol no. 59105) and an ad hoc institutional review board assembled by the RMI Minister of Health.
Study population
We enrolled adults with type 2 diabetes aged 18–75 years. Participants either had an HbA1c ≥64 mmol/mol (≥8.0%) or were diagnosed with type 2 diabetes and taking glucose-lowering medication. Exclusion criteria included heart disease, changes in glucose-lowering medications in the past 3 months and physical or medical conditions that hinder participation. Enrolment was generally representative of Marshallese adults with type 2 diabetes (see the electronic supplementary material [ESM]). Participants provided written informed consent before participating, and demographic variables including biological sex were collected by self-report. Participants were enrolled in five cohorts and randomised in a 1:1 ratio generated by Microsoft Excel. Participants were randomised a few days before baseline data collection to give them time to make accommodations to attend weekly classes. Further details on recruitment, randomisation, the lifestyle intervention and the methods are provided in the protocol manuscript [32].
Standard care
The control group was treated using glucose-lowering pharmacotherapy, according to SMC in the RMI. They were instructed to maintain their current diet and physical activity levels.
PB+Ex intervention
The PB+Ex intervention is described in detail in the protocol manuscript [32]. In brief, the PB+Ex group was instructed to eat a WFPB diet permitting minimal animal products and to exercise 30–60 min/day for 24 weeks. During weeks 1–12, the PB+Ex group received prepared meals, attended group exercise sessions and received group instruction on eating healthfully, cooking, exercising and managing stress (see ESM Table 1 for a list of class topics). The intervention was culturally tailored and developed in partnership with the Marshallese government and local diabetes clinics and included Marshallese staff and popular foods (see the ESM for a detailed description of the cultural adaptation and positionality statements). The intensity of support progressively decreased, with participants attending 15–21 h/week of group classes in weeks 1–2, 8–10 h/week in weeks 3–6 and 4–5 h/week in weeks 7–12. During weeks 13–24 (the follow-up phase), participants were instructed to follow the intervention on their own.
WFPB diet
The prescribed diet was high in fibre (35 g/ 4184 kJ), low in fat (20–25% of energy; saturated fat <7% of energy), moderate in protein (10–15% of energy) and low in sodium (<2400 mg/day). During weeks 1–2 (the intensive phase), PB+Ex participants received 12 prepared meals/week and were instructed to consume no animal products and minimal ground grains and refined carbohydrates. Thereafter, participants received 2 meals/week during weeks 3–6 and 1 meal/week during weeks 7–12. During weeks 3–12, participants could consume small amounts of animal foods, oils, fat-rich foods and processed foods, following a four-tiered food classification system [33]. Specifically, they were instructed to consume 75–100% of energy from whole, unprocessed plant foods (tier 1), such as vegetables, legumes, whole grains and fruit. The remainder of their diet could include ≤25% lightly processed foods (tier 2), ≤10% moderately processed foods and moderate-fat animal products (tier 3) and ≤5% heavily processed foods and high-fat animal products (tier 4).
Exercise
The PB+Ex group was instructed to do moderate-intensity aerobic and resistance exercise 60 min/day during weeks 1–2 and 30–60 min/day during weeks 3–24. During weeks 1–2, participants attended 1 h group exercise classes 4 days/week. Thereafter, they attended group exercise classes twice a week during weeks 3–6 and once a week during weeks 7–12. Participants were also counselled to walk 10–20 min before breakfast and after lunch and dinner.
Cohort differences
To increase intervention intensity, participants in cohorts 3–5 of the PB+Ex group repeated weeks 1 and 2 during weeks 4 and 6. This included a repeat of educational sessions, meals provided and exercise classes.
Study outcomes
Outcomes were assessed at weeks 0, 2, 6, 12 and 24. The primary outcome was glycaemic control, measured by HbA1c, fasting glucose, fasting insulin, HOMA-IR and diabetes medication use. Secondary endpoints were cardiovascular risk factors, including body weight, waist circumference, lipids, systolic blood pressure (SBP), diastolic blood pressure (DBP), resting heart rate, high-sensitivity C-reactive protein (hsCRP) and cardiovascular medication use. Only lab analysts performing the serum assays were blinded.
Serum chemistry
HbA1c, glucose, insulin, total cholesterol, HDL-cholesterol, triglycerides and hsCRP were analysed blinded at the Clinical Laboratory Improvement Amendments-approved laboratory in the Ministry of Health’s Hospital, while LDL-cholesterol was calculated using the Friedewald equation. Triglyceride values >4.52 mmol/l (>400 mg/dl) were Winsorised to minimise the effect of outliers on the analyses. LDL-cholesterol values were treated as missing whenever triglyceride values exceeded 4.52 mmol/l. hsCRP values ≥95 mmol/l (≥10 mg/l) were considered indicative of acute infection and treated as missing.
Medication use
Primary care physicians and/or the Diabetes Wellness Clinic’s clinicians adjusted participants’ medications based on glucometer and/or serum glucose values. PB+Ex participants on insulin were monitored daily with glucometers and instructed to reduce insulin doses when glucose fell to <3.9 mmol/l (<70 mg/dl) or hypoglycaemic symptoms manifested. For SMC participants on insulin, their physicians were responsible for adjusting their medication doses. Diabetes medication use was quantified using the medication effect score (MES) [25], which estimates the HbA1c reduction expected from all glucose-lowering pharmacotherapy [34]. Diabetes remission was defined as achieving HbA1c <48 mmol/mol (<6.5%) after not using glucose-lowering medications for at least 3 months.
Statistical power
The required sample size was estimated using the variances observed in HbA1c and glucose in cohorts 1–2. A sample size of n=120 was needed to have 80% power to detect a 1.1 mmol/l (20 mg/dl) difference in glucose and an 11 mmol/mol (1.0%) difference in HbA1c, given α=0.05.
Statistical analyses
Analyses were performed with two-sided tests and α=0.05, primarily using SAS (version 9.4; SAS Institute; Cary, NC, USA). Baseline data were compared using independent samples t tests or the Mann–Whitney U test if neither raw nor transformed values were normal. The main analysis was intention-to-treat. Continuous data were analysed using linear mixed models, adjusting for baseline values, sex and/or cohort whenever statistically merited. Categorical data were analysed using Fisher’s exact test. Missing medication doses were singly imputed whenever a missing dose was flanked by two timepoints with identical doses and were otherwise treated as missing. When HbA1c values were missing, remission status was singly imputed by assuming HbA1c values changed by no more than 16 mmol/mol (1.5%) between weeks 0 and 2 and by no more than 33 mmol/mol (3.0%) between each subsequent pair of timepoints. Insulin and HOMA-IR were analysed only in participants not on insulin, while MES was analysed only in those taking glucose-lowering medication. The proportion of participants who decreased their medication doses was calculated in the subgroup of participants on the medication(s) at baseline. Lastly, to calculate diabetes remission and decreases in medication doses, we included everyone with sufficient data at either week 12, week 24 or both timepoints, in order to increase the sample size and improve accuracy in the estimated proportions.
Results
Participants
As shown in ESM Fig. 1, we screened 530 people. Of these, 361 did not meet the eligibility criteria, primarily due to HbA1c being out of range and secondarily due to cardiovascular pathologies, such as angina. We randomised 169 participants (SMC: n=90; PB+Ex: n=79), but 31 withdrew before baseline data were collected. Seventy-two participants received the SMC intervention, while 66 received the PB+Ex intervention. Twenty-eight participants (20%) were lost to follow-up at week 24, and retention was similar between groups (p=1.00). Two completers were excluded from the analyses after we later discovered that they no longer had diabetes at baseline. There were no adverse events related to the protocol. Participant characteristics are summarised in Table 1. All participants were of Pacific Islander descent, and 50% were female. Participants had a mean age (±SD) of 54 ± 9 years, a BMI of 29.8 ± 4.9 kg/m2, an HbA1c of 90 ± 23 mmol/mol (10.4 ± 2.1%) and a fasting glucose of 12.9 ± 4.2 mmol/l, indicating high rates of uncontrolled type 2 diabetes. Sixty-one per cent of participants used ≥1 glucose-lowering agent, and metformin and sulfonylureas were each used by 40% of participants. Only 9% of participants were on insulin. Thirty-two per cent of participants were taking ≥1 cardiovascular medication. All participant characteristics were similar between groups at baseline, except SBP, which was 8 mmHg higher in the PB+Ex group (p=0.04). Thus, blood pressure analyses were adjusted for baseline values.
Glycaemic outcomes
ESM Table 2 summarises the results for all cardiometabolic outcomes. Glycaemic outcomes are illustrated in Fig. 1. Compared with SMC, the PB+Ex intervention reduced HbA1c by an additional 13 mmol/mol (1.2%) at week 6 (−20 vs −7 mmol/mol [−1.8% vs −0.6%]; 95% CI −19, −7 mmol/mol [−1.7%, −0.6%]; p<0.0001), 14 mmol/mol (1.3%) at week 12 (−22 vs −7 mmol/mol [−2.0% vs −0.7%]; 95% CI −20, −8 mmol/mol [−1.8%, −0.8%]; p<0.0001) and 8 mmol/mol (0.7%) at week 24 (−16 vs −8 mmol/mol [−1.4% vs −0.7%]; 95% CI −14, −1 mmol/mol [−1.3%, −0.1%]; p=0.01) (Fig. 1a). Since many participants decreased their glucose-lowering medication doses, we used the MES to calculate the true reduction in HbA1c if medication doses had not been adjusted (i.e. HbA1c+MES; Fig. 1b). Had medication doses not been changed, the PB+Ex intervention would have reduced HbA1c by an additional 13 mmol/mol (1.2%) at week 6 (−21 vs −8 mmol/mol [−1.9% vs −0.8%]; 95% CI −20, −6 mmol/mol [−1.8%, −0.5%]; p=0.0004), 19 mmol/mol (1.7%) at week 12 (−26 vs −7 mmol/mol [−2.4% vs −0.6%]; 95% CI −26, −12 mmol/mol [−2.4%, −1.1%]; p<0.0001) and 11 mmol/mol (1.0%) at week 24 (−18 vs −7 mmol/mol [−1.6% vs −0.6%]; 95% CI −18, −3 mmol/mol [−1.7%, −0.3%]; p=0.005). The PB+Ex intervention also reduced glucose by an additional 3.2 mmol/l at week 2 (95% CI −4.4, −2.0 mmol/l; p<0.0001), 3.0 mmol/l at week 6 (95% CI −4.2, −1.8 mmol/l; p<0.0001) and 2.1 mmol/l at week 12 (95% CI −3.3, −0.9 mmol/l; p=0.0007) relative to SMC, but not at week 24 (p=0.24) (Fig. 1c). Among participants not taking insulin (n=124), the PB+Ex intervention reduced fasting insulin at week 6 by 17.4 pmol/l (−12.6 vs −4.8 pmol/l; 95% CI −32.4, −2.5 pmol/l; p=0.02) but did not affect insulin at any other timepoint (p≥0.17; Fig. 1d). The PB+Ex intervention also reduced HOMA-IR at week 2 (−1.74; 95% CI −3.37, −0.11; p=0.04), week 6 (−2.98; 95% CI −4.61, −1.35; p=0.0004) and week 12 (−1.74; 95% CI −3.25, −0.23; p=0.02), but not at week 24 (p=0.53) (ESM Fig. 2b).
Glycaemic control. The PB+Ex intervention was more effective than SMC at improving (a) HbA1c and (b) the MES plus HbA1c (HbA1c+MES), which measures the true effect on HbA1c if glucose-lowering medication doses had not been changed. The PB+Ex intervention also improved (c) fasting glucose at all timepoints except week 24 and (d) fasting insulin at week 2 only. Data shown are least-squares means ± SEMs. *p<0.05
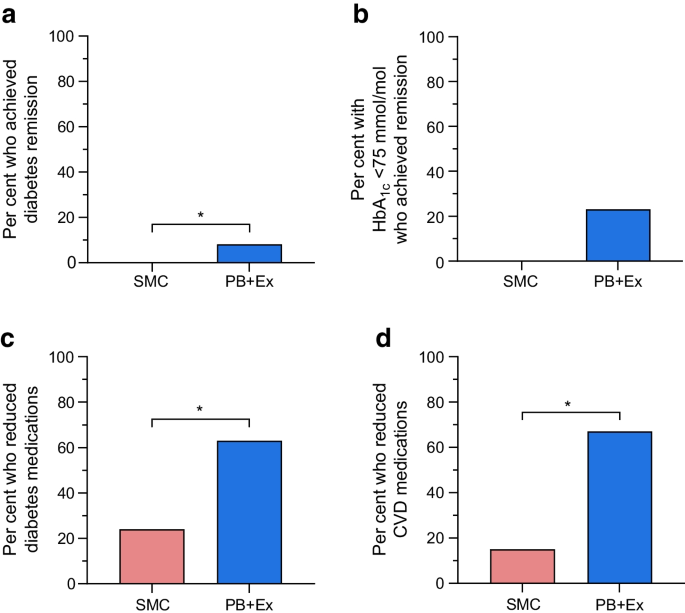
Diabetes remission and medication use
Diabetes remission rates and medication use are shown in Fig. 2. Eight per cent (n=5) of PB+Ex participants achieved diabetes remission vs 0% in the SMC group (n=127; p=0.02; Fig. 2a). All PB+Ex participants who achieved remission had a baseline HbA1c <75 mmol/mol (<9.0%). In a post hoc analysis, the PB+Ex intervention induced remission in 23% of participants with a baseline HbA1c <75 mmol/mol (<9.0%), although this was not statistically different from the SMC group (vs 0%; n=36; p=0.13; Fig. 2b). In addition, 63% of PB+Ex participants reduced their baseline dose of glucose-lowering medications vs only 24% of SMC participants (n=56; p=0.006). This was mirrored by statistically significant decreases in MES at all timepoints, including at week 12 (−6 mmol/mol [−0.5%]; 95% CI −8, −3 mmol/mol; p=0.0002) and week 24 (−9 mmol/mol [−0.7%]; 95% CI −12, −5 mmol/mol; p<0.0001) (n=91; ESM Fig. 2a). Lastly, 67% of PB+Ex participants reduced their dose of one or more cardiovascular medications vs only 15% of the SMC group (n=19; p=0.046).
Diabetes remission and medication use. (a) PB+Ex was more effective than SMC at inducing diabetes remission. (b) About one-quarter of PB+Ex participants with a baseline HbA1c <75 mmol/mol (<9%) achieved remission. The PB+Ex group also significantly reduced their doses of (c) diabetes medications and (d) cardiovascular medications. Data shown are proportions (%). *p<0.05
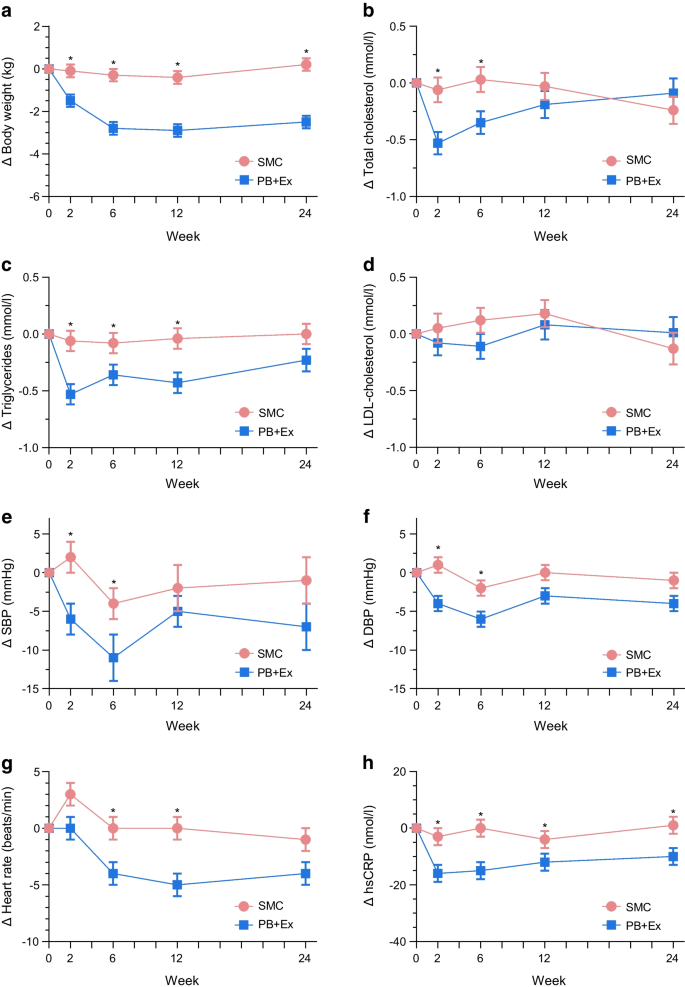
Body weight and cardiovascular disease risk factors
Figure 3 shows the effects on body weight and cardiovascular risk factors. Relative to SMC, the PB+Ex intervention modestly reduced body weight at all timepoints, including week 2 (−1.4 kg; 95% CI −2.2, −0.6 kg; p=0.001), week 6 (−2.6 kg; 95% CI −3.4, −1.7 kg; p<0.0001), week 12 (−2.5 kg; 95% CI −3.4, −1.6 kg; p<0.0001; Fig. 3a) and week 24 (−2.7 kg; 95% CI −3.6, −1.8 kg; p<0.0001). Similarly, waist circumference was significantly reduced in the PB+Ex group at weeks 6 (−1.8 cm; 95% CI −3.6, 0.0 cm; p=0.04), 12 (−1.9 cm; 95% CI −3.7, −0.1 cm; p=0.04) and 24 (−3.8 cm; 95% CI −5.8, −1.8 cm; p=0.0002), but not at week 2 (p=0.34; ESM Fig. 2c). The PB+Ex intervention also reduced total cholesterol by an additional 0.47 mmol/l at week 2 (95% CI −0.76, −0.19 mmol/l; p=0.001) and 0.38 mmol/l at week 6 (95% CI −0.67, −0.08 mmol/l; p=0.01), but not at week 12 or week 24 (p≥0.34; Fig. 3b). This was driven by large decreases in triglycerides at week 2 (−0.47 mmol/l; 95% CI −0.72, −0.23 mmol/l; p=0.0002), week 6 (−0.28 mmol/l; 95% CI −0.53, −0.04 mmol/l; p=0.02) and week 12 (−0.38 mmol/l; 95% CI −0.63, −0.13 mmol/l; p=0.003), but not at week 24 (p=0.09; Fig. 3c). There were no differences in LDL-cholesterol (p≥0.13; Fig. 3d) or HDL-cholesterol (p≥0.09; ESM Fig. 1d) at any timepoint. In addition, the PB+Ex intervention reduced SBP by 8 mmHg at both week 2 (95% CI −14, −1 mmHg; p=0.02) and week 6 (95% CI −14, −1 mmHg; p=0.03), but not at week 12 or week 24 (p≥0.13; Fig. 3e). Similarly, the PB+Ex intervention reduced DBP by 5 mmHg at week 2 (95% CI −9, −2 mmHg; p=0.003) and 4 mmHg at week 6 (95% CI −8, 0 mmHg; p=0.03), but not at week 12 or week 24 (p≥0.08; Fig. 3f). Relative to SMC, the PB+Ex intervention also reduced heart rate by 4 beats/min at week 6 (95% CI −8, −1 beats/min; p=0.02) and 5 beats/min at week 12 (95% CI −8, −1 beats/min; p=0.02), but not at week 2 or week 24 (p≥0.10; Fig. 3g). Lastly, the PB+Ex intervention more effectively lowered hsCRP at all timepoints, including week 2 (−14 nmol/l; 95% CI −21, −6 nmol/l; p=0.0003), week 6 (−14 nmol/l; 95% CI −22, −7 nmol/l; p=0.0003), week 12 (−9 nmol/l; 95% CI −16, −1 nmol/l; p=0.02) and week 24 (−11 nmol/l; 95% CI −19, −4 nmol/l; p=0.005; Fig. 3h).
Cardiovascular disease risk factors. The PB+Ex intervention was more effective than SMC at lowering (a) body weight and (h) hsCRP. The PB+Ex intervention improved (b) total cholesterol, (c) triglycerides, (e) SBP, (f) DBP and (g) heart rate at intermediate timepoints but not at week 24. There were no differences in (d) LDL-cholesterol. Data shown are least-squares means ± SEMs. *p<0.05
Discussion
We conducted the largest and longest randomised controlled trial to compare a WFPB intervention vs SMC in individuals with type 2 diabetes. We implemented a lifestyle intervention involving a WFPB diet including limited animal products and moderate exercise, which progressively decreased in intensity. The PB+Ex intervention was superior to SMC for improving HbA1c, hsCRP, weight and waist circumference. The PB+Ex intervention also reduced the need for diabetes and cardiovascular medications and induced type 2 diabetes remission in some participants. At interim timepoints, the PB+Ex intervention improved nearly every cardiometabolic endpoint, although these differences attenuated as the intervention intensity decreased.
The PB+Ex intervention was far more effective at improving glycaemic control than SMC centred on medication management: it decreased HbA1c by an additional 14 mmol/mol (1.3%) at week 12 and 8 mmol/mol (0.7%) at week 24. Importantly, the ‘true’ effect on HbA1c levels was even larger than this because the SMC group increased their dose of glucose-lowering medications by the equivalent of 360 mg/day of metformin at week 24, whereas the PB+Ex group reduced their dose by 820 mg/day (a between-group difference of 1180 mg/day) [34]. After adjusting for medication changes, the PB+Ex intervention lowered HbA1c by an additional 19 mmol/mol (1.7%) at week 12 and 11 mmol/mol (1.0%) at week 24 relative to SMC. Such a large improvement in HbA1c levels could dramatically reduce the risks of comorbidities, particularly myocardial infarction and microvascular complications, and profoundly improve clinical management of type 2 diabetes. Interestingly, much of the glycaemic improvement occurred in the first 2 weeks of the study before any substantial weight loss occurred. The PB+Ex intervention decreased fasting glucose by a dramatic 4.0 mmol/l relative to baseline within only 2 weeks. This suggests that the improvements were due to changes in diet quality and/or physical activity rather than weight loss. For comparison, the glycaemic improvements we observed were much larger than the 7–11 mmol/mol (0.6–1.1%) reduction in HbA1c reported in other clinical trials on plant-based diets [17, 35, 36] or the 3–4 mmol/mol (0.3–0.4%) reported in meta-analyses [13, 37]. Plus, most studies on plant-based interventions report no improvements in fasting glucose or insulin [17, 35, 36, 38, 39]. The larger effects we observed may be due to the very high amounts of whole foods, the addition of moderate exercise, the provision of prepared meals and intensive instruction, participants having higher baseline HbA1c values than in the USA [27] and/or participants having a lower quality diet at baseline [28,29,30,31, 40, 41]. A complex interplay of socioeconomic, geopolitical, and cultural factors involving limited arable land, displacement, a remote location, unemployment, and poverty have decreased access to nutritious foods [29, 42].
The PB+Ex intervention also reduced the need for glucose-lowering and cardiovascular medications in roughly two-thirds of PB+Ex participants. Our intervention induced a greater reduction in medication use than in any other clinical trial on plant-based diets [15, 17, 35, 36, 38, 39, 43]. The PB+Ex intervention also induced type 2 diabetes remission in 8% of all participants and 23% of those with a baseline HbA1c <75 mmol/mol (<9.0%). The participants who went into remission lost modest or no weight (~0–6 kg), and one even gained weight. For comparison, in the DiRECT trial, where participants’ mean baseline HbA1c was 61 mmol/mol (7.7%), only 7% of participants who lost 0–5 kg went into remission [3]. This important finding suggests that type 2 diabetes remission is possible through improving diet quality and/or increasing physical activity, even if individuals do not lose weight.
We also investigated the effects of a PB+Ex intervention on cardiovascular risk factors. The PB+Ex intervention reduced total cholesterol and triglycerides at intermediate timepoints but did not affect LDL-cholesterol. It is unclear why we found a dramatic reduction in triglycerides but not LDL-cholesterol, as this conflicts with a meta-analysis reporting that plant-based diets lower total and LDL-cholesterol but do not affect triglycerides [44]. The PB+Ex intervention also decreased SBP by 8 mmHg at both week 2 and week 6 and DBP by 5 and 4 mmHg at weeks 2 and 6, respectively. However, the effects vanished as the intervention intensity waned. The effects we observed at intermediate time points were larger than those reported in a meta-analysis of plant-based diets, which reported 3 and 2 mmHg improvements in SBP and DBP, respectively [45]. The PB+Ex intervention also decreased heart rate by 4 and 5 beats/min at weeks 6 and 12, respectively, compared with the SMC, although the effect lost significance by week 24 (p=0.10). These intermediate improvements in triglycerides, blood pressure and heart rate may partially explain why plant-based diets are associated with lower cardiovascular disease incidence and mortality risk [46]. Finally, the PB+Ex intervention reduced hsCRP at all timepoints, indicating the intervention decreased inflammation. Notably, biological sex was not a statistically significant covariate for any cardiometabolic outcome, suggesting no differences between males and females.
The strengths of this study include the innovative diet approach, large sample size, long duration, high male representation (50%), high-priority population, the cultural adaptation and using a lifestyle intervention that progressively decreased in intensity. The latter factor provided us with a unique opportunity to test different ‘doses’ of the PB+Ex intervention. Interestingly, during the most intensive phase, participants experienced robust improvements in nearly every cardiometabolic endpoint, although the effects for fasting glucose, insulin, triglycerides, heart rate and blood pressure waned as intervention intensity decreased. This suggests that a WFPB diet with moderate exercise can improve most cardiometabolic risk factors, but the effects depend on the intervention intensity and/or level of adherence. Limitations of this study include that no adherence data or diet records were collected; participants were randomised 3–5 days prior to baseline testing; some SMC participants adopted elements of the PB+Ex lifestyle intervention (which likely diluted estimates of the true treatment effects); no Marshallese citizens assisted with study design, data interpretation or manuscript writing; and there were minor differences in the intervention intensity in cohorts 1–2 vs 3–5 (although there were no statistically significant differences between cohorts in virtually all outcomes).
In conclusion, a WFPB lifestyle intervention with moderate exercise was more effective than SMC at improving glycaemic control, body weight, waist circumference and inflammation. It also lessened the need for glucose-lowering and cardiovascular medications and induced type 2 diabetes remission in some participants. Overall, our findings support the ‘food as medicine’ concept and suggest that WFPB interventions with moderate exercise may dramatically reduce the risk of comorbidities. A WFPB diet with moderate exercise can be offered as a highly effective, evidence-based lifestyle intervention for individuals with type 2 diabetes.
Abbreviations
- DBP:
-
Diastolic blood pressure
- DiRECT:
-
Diabetes Remission Clinical Trial
- hsCRP:
-
High-sensitivity C-reactive protein
- MES:
-
Medication effect score
- PB+Ex:
-
Whole-food, plant-based intervention with moderate exercise
- RMI:
-
Republic of the Marshall Islands
- SBP:
-
Systolic blood pressure
- SMC:
-
Standard medical care
- VLCD:
-
Very-low-calorie diet
- WFPB:
-
Whole-food, plant-based
References
Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J (2020) Epidemiology of type 2 diabetes - global burden of disease and forecasted trends. J Epidemiol Glob Health 10(1):107–111. https://doi.org/10.2991/jegh.k.191028.001
Ong KL, Stafford LK, McLaughlin SA et al (2023) Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 402(10397):203–234. https://doi.org/10.1016/s0140-6736(23)01301-6
Lean ME, Leslie WS, Barnes AC et al (2018) Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet 391(10120):541–551. https://doi.org/10.1016/s0140-6736(17)33102-1
Steven S, Hollingsworth KG, Al-Mrabeh A et al (2016) Very low-calorie diet and 6 months of weight stability in type 2 diabetes: pathophysiological changes in responders and nonresponders. Diabetes Care 39(5):808–815. https://doi.org/10.2337/dc15-1942
Paisey RB, Frost J, Harvey P et al (2002) Five year results of a prospective very low calorie diet or conventional weight loss programme in type 2 diabetes. J Hum Nutr Diet 15(2):121–127. https://doi.org/10.1046/j.1365-277x.2002.00342.x
Rafiullah M, Musambil M, David SK (2022) Effect of a very low-carbohydrate ketogenic diet vs recommended diets in patients with type 2 diabetes: a meta-analysis. Nutr Rev 80(3):488–502. https://doi.org/10.1093/nutrit/nuab040
Goldenberg JZ, Day A, Brinkworth GD et al (2021) Efficacy and safety of low and very low carbohydrate diets for type 2 diabetes remission: systematic review and meta-analysis of published and unpublished randomized trial data. BMJ 372:m4743. https://doi.org/10.1136/bmj.m4743
Noto H, Goto A, Tsujimoto T, Noda M (2013) Low-carbohydrate diets and all-cause mortality: a systematic review and meta-analysis of observational studies. PLoS One 8(1):e55030. https://doi.org/10.1371/journal.pone.0055030
Rosenbaum M, Hall KD, Guo J et al (2019) Glucose and lipid homeostasis and inflammation in humans following an isocaloric ketogenic diet. Obesity (Silver Spring) 27(6):971–981. https://doi.org/10.1002/oby.22468
Hall KD, Guo J, Courville AB et al (2021) Effect of a plant-based, low-fat diet versus an animal-based, ketogenic diet on ad libitum energy intake. Nat Med 27(2):344–353. https://doi.org/10.1038/s41591-020-01209-1
Webster CC, van Boom KM, Armino N et al (2020) Reduced glucose tolerance and skeletal muscle GLUT4 and IRS1 content in cyclists habituated to a long-term low-carbohydrate, high-fat diet. Int J Sport Nutr Exerc Metab 30(3):210–217. https://doi.org/10.1123/ijsnem.2019-0359
Chawla S, Tessarolo Silva F, Amaral Medeiros S, Mekary RA, Radenkovic D (2020) The effect of low-fat and low-carbohydrate diets on weight loss and lipid levels: a systematic review and meta-analysis. Nutrients 12(12):3774. https://doi.org/10.3390/nu12123774
Toumpanakis A, Turnbull T, Alba-Barba I (2018) Effectiveness of plant-based diets in promoting well-being in the management of type 2 diabetes: a systematic review. BMJ Open Diabetes Res Care 6(1):e000534. https://doi.org/10.1136/bmjdrc-2018-000534
de Carvalho GB, Dias-Vasconcelos NL, Santos RKF, Brandão-Lima PN, da Silva DG, Pires LV (2020) Effect of different dietary patterns on glycemic control in individuals with type 2 diabetes mellitus: a systematic review. Crit Rev Food Sci Nutr 60(12):1999–2010. https://doi.org/10.1080/10408398.2019.1624498
Jenkins DJ, Jones PJ, Abdullah MM et al (2022) Low-carbohydrate vegan diets in diabetes for weight loss and sustainability: a randomized controlled trial. Am J Clin Nutr 116(5):1240–1250. https://doi.org/10.1093/ajcn/nqac203
Dunaief DM, Fuhrman J, Dunaief JL, Ying G (2012) Glycemic and cardiovascular parameters improved in type 2 diabetes with the high nutrient density (HND) diet. Open J Prev Med 2(3):364–371. https://doi.org/10.4236/ojpm.2012.23053
Kahleova H, Matoulek M, Malinska H et al (2011) Vegetarian diet improves insulin resistance and oxidative stress markers more than conventional diet in subjects with Type 2 diabetes. Diabet Med 28(5):549–559. https://doi.org/10.1111/j.1464-5491.2010.03209.x
Karlsen M, Panigraphi G, Kelly J (2021) 503-P: intensive lifestyle interventions for treatment towards remission of type 2 diabetes: a case series. Diabetes 70(Suppl 1):503-P. https://doi.org/10.2337/db21-503-P
Anderson JW, Ward K (1979) High-carbohydrate, high-fiber diets for insulin-treated men with diabetes mellitus. Am J Clin Nutr 32(11):2312–2321. https://doi.org/10.1093/ajcn/32.11.2312
Campbell TM, Campbell EK, Attia J et al (2023) The acute effects of a DASH diet and whole food, plant-based diet on insulin requirements and related cardiometabolic markers in individuals with insulin-treated type 2 diabetes. Diabetes Res Clin Pract 202:110814. https://doi.org/10.1016/j.diabres.2023.110814
Austin G, Ferguson JJA, Garg ML (2021) Effects of plant-based diets on weight status in type 2 diabetes: a systematic review and meta-analysis of randomised controlled trials. Nutrients 13(11):4099. https://doi.org/10.3390/nu13114099
Tran E, Dale HF, Jensen C, Lied GA (2020) Effects of plant-based diets on weight status: a systematic review. Diabetes Metab Syndr Obes 13:3433–3448. https://doi.org/10.2147/dmso.S272802
Melina V, Craig W, Levin S (2016) Position of the academy of nutrition and dietetics: vegetarian diets. J Acad Nutr Diet 116(12):1970–1980. https://doi.org/10.1016/j.jand.2016.09.025
Moore WJ, McGrievy ME, Turner-McGrievy GM (2015) Dietary adherence and acceptability of five different diets, including vegan and vegetarian diets, for weight loss: the New DIETs study. Eat Behav 19:33–38. https://doi.org/10.1016/j.eatbeh.2015.06.011
Sun H, Saeedi P, Karuranga S et al (2022) IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract 183:109119. https://doi.org/10.1016/j.diabres.2021.109119
Ahlgren I, Yamada S, Wong A (2014) Rising oceans, climate change, food aid, and human rights in the Marshall Islands. Health Hum Rights 16(1):69–80
Hankosky ER, Schapiro D, Gunn KB, Lubelczyk EB, Mitroi J, Nelson DR (2023) Gaps remain for achieving HbA1c targets for people with type 1 or type 2 diabetes using insulin: results from NHANES 2009–2020. Diabetes Ther 14(6):967–975. https://doi.org/10.1007/s13300-023-01399-0
Kodish SR, Matean M, Grey K et al (2022) Conceptualizing multi-level determinants of infant and young child nutrition in the Republic of Marshall Islands-a socio-ecological perspective. PLOS Glob Public Health 2(12):e0001343. https://doi.org/10.1371/journal.pgph.0001343
McElfish PA, Smith L, Sparks K et al (2019) A community-based participatory approach to promote healthy eating among Marshallese. Hawaii J Health Soc Welf 78(11):332–337
Gittelsohn J, Dyckman W, Tan ML et al (2006) Development and implementation of a food store-based intervention to improve diet in the Republic of the Marshall Islands. Health Promot Pract 7(4):396–405. https://doi.org/10.1177/1524839905278620
Dela Cruz R, Novotny R, Wilkens LR et al (2023) Diet quality of young children in the US-Affiliated Pacific’s Children’s Healthy Living (CHL) program. J Acad Nutr Diet 123(12):1781–1792. https://doi.org/10.1016/j.jand.2023.08.003
Davis BC, Jamshed H, Peterson CM et al (2019) An intensive lifestyle intervention to treat type 2 diabetes in the republic of the Marshall islands: protocol for a randomized controlled trial. Front Nutr 6:79. https://doi.org/10.3389/fnut.2019.00079
Davis B, Barnard T (2003) Defeating diabetes: a no-nonsense approach to type 2 diabetes and the diabesity epidemic. Healthy Living Publications, Summertown, TN, USA
Alexopoulos AS, Yancy WS, Edelman D et al (2021) Clinical associations of an updated medication effect score for measuring diabetes treatment intensity. Chronic Illn 17(4):451–462. https://doi.org/10.1177/1742395319884096
Lee YM, Kim SA, Lee IK et al (2016) Effect of a brown rice based vegan diet and conventional diabetic diet on glycemic control of patients with type 2 diabetes: a 12-week randomized clinical trial. PLoS One 11(6):e0155918. https://doi.org/10.1371/journal.pone.0155918
Barnard ND, Cohen J, Jenkins DJ et al (2009) A low-fat vegan diet and a conventional diabetes diet in the treatment of type 2 diabetes: a randomized, controlled, 74-wk clinical trial. Am J Clin Nutr 89(5):1588s–1596s. https://doi.org/10.3945/ajcn.2009.26736H
Viguiliouk E, Kendall CW, Kahleová H et al (2019) Effect of vegetarian dietary patterns on cardiometabolic risk factors in diabetes: a systematic review and meta-analysis of randomized controlled trials. Clin Nutr 38(3):1133–1145. https://doi.org/10.1016/j.clnu.2018.05.032
Barnard ND, Levin SM, Gloede L, Flores R (2018) Turning the waiting room into a classroom: weekly classes using a vegan or a portion-controlled eating plan improve diabetes control in a randomized translational study. J Acad Nutr Diet 118(6):1072–1079. https://doi.org/10.1016/j.jand.2017.11.017
Bunner AE, Wells CL, Gonzales J, Agarwal U, Bayat E, Barnard ND (2015) A dietary intervention for chronic diabetic neuropathy pain: a randomized controlled pilot study. Nutr Diabetes 5(5):e158. https://doi.org/10.1038/nutd.2015.8
Gittelsohn J, Haberle H, Vastine AE, Dyckman W, Palafox NA (2003) Macro- and microlevel processes affect food choice and nutritional status in the republic of the marshall islands. J Nutr 133(1):310s–313s. https://doi.org/10.1093/jn/133.1.310S
Hingle M, Short E, Aflague T et al (2023) Food security is associated with higher diet quality among children of the US-Affiliated Pacific Region. J Nutr 153(3):848–856. https://doi.org/10.1016/j.tjnut.2023.01.015
Yamada S, Palafox N (2001) On the biopsychosocial model: the example of political economic causes of diabetes in the Marshall Islands. Fam Med 33(9):702–704
Nicholson AS, Sklar M, Barnard ND, Gore S, Sullivan R, Browning S (1999) Toward improved management of NIDDM: a randomized, controlled, pilot intervention using a lowfat, vegetarian diet. Prev Med 29(2):87–91. https://doi.org/10.1006/pmed.1999.0529
Koch CA, Kjeldsen EW, Frikke-Schmidt R (2023) Vegetarian or vegan diets and blood lipids: a meta-analysis of randomized trials. Eur Heart J 44(28):2609–2622. https://doi.org/10.1093/eurheartj/ehad211
Lee KW, Loh HC, Ching SM, Devaraj NK, Hoo FK (2020) Effects of vegetarian diets on blood pressure lowering: a systematic review with meta-analysis and trial sequential analysis. Nutrients 12(6):1604. https://doi.org/10.3390/nu12061604
Quek J, Lim G, Lim WH et al (2021) The association of plant-based diet with cardiovascular disease and mortality: a meta-analysis and systematic review of prospect cohort studies. Front Cardiovasc Med 8:756810. https://doi.org/10.3389/fcvm.2021.756810
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Acknowledgements
The authors are extremely grateful to the government of the Republic of the Marshall Islands, especially the Ministry of Health for providing Marshallese staff and medical professionals, sample processing and the building to set up the Diabetes Wellness Center; the RMI Diabetes Wellness Clinic for providing aid in recruitment and medical care for SMC participants; and the Canvasback Missions staff, who were invaluable in working with the Ministry of Health and conducting this trial. The authors also thank R. D. Harris (former physician at The Meridian Senior Retirement Center) and J. D. Spence (President and co-founder of Canvasback Missions, Inc.) for their help in conducting the trial and coordinating logistics. An abstract and a research poster were presented virtually at the American Diabetes Association’s 82nd Scientific Sessions on 3 June 2022.
Data availability
The datasets generated during and/or analysed in the current study are available from the corresponding author upon reasonable request.
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium. This research was funded by the Department of the Army (W81XWH-05-1-0547). The sponsor had no role in the design and conduct of the trial or in the analysis, interpretation, and publication of data. CJH received support through a National Institutes of Health Predoctoral T32 Obesity Fellowship (T32 HL105349). The content is solely the responsibility of the authors and does not necessarily reflect the views of the National Institutes of Health.
Authors’ relationships and activities
BCD is the author of the books Defeating Diabetes and The Kick Diabetes Cookbook: An Action Plan and Recipes for Defeating Diabetes. The authors declare that there are no other relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
JHK designed the study, with input from JS. BCD and JHK conducted the study, including designing the menus, administering the intervention and acquiring data. CJH and CMP performed the statistical analyses and drafted the manuscript. All authors interpreted study data and revised and approved the final version of the manuscript. JHK is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hanick, C.J., Peterson, C.M., Davis, B.C. et al. A whole-food, plant-based intensive lifestyle intervention improves glycaemic control and reduces medications in individuals with type 2 diabetes: a randomised controlled trial. Diabetologia (2024). https://doi.org/10.1007/s00125-024-06272-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00125-024-06272-8