Abstract
Aims/hypothesis
Many studies have examined the relationship between plasma metabolites and type 2 diabetes progression, but few have explored saliva and multi-fluid metabolites.
Methods
We used LC/MS to measure plasma (n=1051) and saliva (n=635) metabolites among Puerto Rican adults from the San Juan Overweight Adults Longitudinal Study. We used elastic net regression to identify plasma, saliva and multi-fluid plasma–saliva metabolomic scores predicting baseline HOMA-IR in a training set (n=509) and validated these scores in a testing set (n=340). We used multivariable Cox proportional hazards models to estimate HRs for the association of baseline metabolomic scores predicting insulin resistance with incident type 2 diabetes (n=54) and prediabetes (characterised by impaired glucose tolerance, impaired fasting glucose and/or high HbA1c) (n=130) at 3 years, along with regression from prediabetes to normoglycaemia (n=122), adjusting for traditional diabetes-related risk factors.
Results
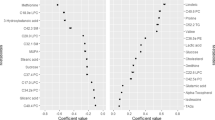
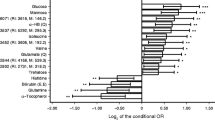
Plasma, saliva and multi-fluid plasma–saliva metabolomic scores predicting insulin resistance included highly weighted metabolites from fructose, tyrosine, lipid and amino acid metabolism. Each SD increase in the plasma (HR 1.99 [95% CI 1.18, 3.38]; p=0.01) and multi-fluid (1.80 [1.06, 3.07]; p=0.03) metabolomic scores was associated with higher risk of type 2 diabetes. The saliva metabolomic score was associated with incident prediabetes (1.48 [1.17, 1.86]; p=0.001). All three metabolomic scores were significantly associated with lower likelihood of regressing from prediabetes to normoglycaemia in models adjusting for adiposity (HRs 0.72 for plasma, 0.78 for saliva and 0.72 for multi-fluid), but associations were attenuated when adjusting for lipid and glycaemic measures.
Conclusions/interpretation
The plasma metabolomic score predicting insulin resistance was more strongly associated with incident type 2 diabetes than the saliva metabolomic score. Only the saliva metabolomic score was associated with incident prediabetes.
Graphical Abstract




Similar content being viewed by others
Abbreviations
- CRP:
-
C-reactive protein
- FDR:
-
False discovery rate
- FPG:
-
Fasting plasma glucose
- HDL-C:
-
HDL-cholesterol
- LDL-C:
-
LDL-cholesterol
- MET-h/week:
-
Metabolic equivalent hours per week
- SOALS:
-
San Juan Overweight Adults Longitudinal Study
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- WC:
-
Waist circumference
References
Razzaghi H, Martin DN, Quesnel-Crooks S et al (2019) 10-year trends in noncommunicable disease mortality in the Caribbean region. Rev Panam Salud Publica 43:e37. https://doi.org/10.26633/RPSP.2019.37
International Diabetes Federation (2021) IDF Diabetes Atlas, 10th edn. International Diabetes Federation, Brussels
Pérez CM, Soto-Salgado M, Suárez E, Guzmán M, Ortiz AP (2015) High prevalence of diabetes and prediabetes and their coexistence with cardiovascular risk factors in a hispanic community. J Immigr Minor Health 17(4):1002–1009. https://doi.org/10.1007/s10903-014-0025-8
Sallar A, Dagogo-Jack S (2020) Regression from prediabetes to normal glucose regulation: State of the science. Exp Biol Med (Maywood) 245(10):889–896. https://doi.org/10.1177/1535370220915644
Rooney MR, Fang M, Ogurtsova K et al (2023) Global prevalence of prediabetes. Diabetes Care 46(7):1388–1394. https://doi.org/10.2337/dc22-2376
Johnson JA, Cavanagh S, Jacelon CS, Chasan-Taber L (2017) The diabetes disparity and Puerto Rican identified individuals: a systematic literature review. Diabetes Educ 43(2):153–162. https://doi.org/10.1177/0145721716687662
Rodriguez F, Lee UJ, Barone N et al (2021) Risk factor control across the spectrum of cardiovascular risk: Findings from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Am J Prev Cardiol 5:100147. https://doi.org/10.1016/j.ajpc.2021.100147
Lipton R, Losey L, Giachello AL, Corral M, Girotti MH, Mendez JJ (1996) Factors affecting diabetes treatment and patient education among Latinos: results of a preliminary study in Chicago. J Med Syst 20(5):267–276. https://doi.org/10.1007/BF02257040
Morze J, Wittenbecher C, Schwingshackl L et al (2022) Metabolomics and type 2 diabetes risk: an updated systematic review and meta-analysis of prospective cohort studies. Diabetes Care 45(4):1013–1024. https://doi.org/10.2337/dc21-1705
Long J, Yang Z, Wang L et al (2020) Metabolite biomarkers of type 2 diabetes mellitus and pre-diabetes: a systematic review and meta-analysis. BMC Endocr Disord 20:174. https://doi.org/10.1186/s12902-020-00653-x
Gar C, Rottenkolber M, Prehn C, Adamski J, Seissler J, Lechner A (2018) Serum and plasma amino acids as markers of prediabetes, insulin resistance, and incident diabetes. Critical Reviews in Clinical Laboratory Sciences 55(1):21–32. https://doi.org/10.1080/10408363.2017.1414143
Chai JC, Chen G-C, Yu B et al (2022) Serum metabolomics of incident diabetes and glycemic changes in a population with high diabetes burden: the hispanic community health study/study of latinos. Diabetes 71(6):1338–1349. https://doi.org/10.2337/db21-1056
Rivas-Tumanyan S, Pacheco LS, Haslam DE et al (2022) Novel plasma metabolomic markers associated with diabetes progression in Older Puerto Ricans. Metabolites 12(6):513. https://doi.org/10.3390/metabo12060513
Chen G-C, Chai JC, Yu B et al (2020) Serum sphingolipids and incident diabetes in a US population with high diabetes burden: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Am J Clin Nutr 112(1):57–65. https://doi.org/10.1093/ajcn/nqaa114
Mujalli A, Farrash WF, Alghamdi KS, Obaid AA (2023) Metabolite alterations in autoimmune diseases: a systematic review of metabolomics studies. Metabolites 13(9):987. https://doi.org/10.3390/metabo13090987
Chuchueva N, Carta F, Nguyen HN et al (2023) Metabolomics of head and neck cancer in biofluids: an integrative systematic review. Metabolomics 19(9):77. https://doi.org/10.1007/s11306-023-02038-2
Li C-X, Wheelock CE, Sköld CM, Wheelock ÅM (2018) Integration of multi-omics datasets enables molecular classification of COPD. Eur Respir J 51(5):1701930. https://doi.org/10.1183/13993003.01930-2017
González-Moles MÁ, Ramos-García P (2021) State of evidence on oral health problems in diabetic patients: a critical review of the literature. J Clin Med 10(22):5383. https://doi.org/10.3390/jcm10225383
Favale N, Farina R, Carrieri A et al (2024) Functional profile of oral plaque microbiome: Further insight into the bidirectional relationship between type 2 diabetes and periodontitis. Mol Oral Microbiol 39(2):62–79. https://doi.org/10.1111/omi.12418
Gupta S, Nayak MT, Sunitha J, Dawar G, Sinha N, Rallan NS (2017) Correlation of salivary glucose level with blood glucose level in diabetes mellitus. J Oral Maxillofac Pathol 21(3):334–339. https://doi.org/10.4103/jomfp.JOMFP_222_15
Kadashetti V, Baad R, Malik N et al (2015) Glucose level estimation in diabetes mellitus by Saliva: a bloodless revolution. Roman J Int Med 53(3):248–252. https://doi.org/10.1515/rjim-2015-0032
Kumar S, Padmashree S, Jayalekshmi R (2014) Correlation of salivary glucose, blood glucose and oral candidal carriage in the saliva of type 2 diabetics: a case-control study. Contemp Clin Dent 5(3):312–317. https://doi.org/10.4103/0976-237X.137925
Carramolino-Cuéllar E, Lauritano D, Carinci F et al (2017) Salivary glucose as a metabolic control marker in patients with type 2 diabetes. J Biol Regul Homeost Agents 31(2 Suppl 1):181–187
Barnes VM, Kennedy AD, Panagakos F et al (2014) Global metabolomic analysis of human saliva and plasma from healthy and diabetic subjects, with and without periodontal disease. PLoS One 9(8):e105181. https://doi.org/10.1371/journal.pone.0105181
Mook-Kanamori DO, Selim MME-D, Takiddin AH et al (2014) 1,5-Anhydroglucitol in saliva is a noninvasive marker of short-term glycemic control. J Clin Endocrinol Metab. 99(3):E479–E483. https://doi.org/10.1210/jc.2013-3596
Halama A, Kulinski M, Kader SA et al (2016) Measurement of 1,5-anhydroglucitol in blood and saliva: from non-targeted metabolomics to biochemical assay. J Transl Med 14(1):140. https://doi.org/10.1186/s12967-016-0897-6
Yousri NA, Mook-Kanamori DO, Selim MME-D et al (2015) A systems view of type 2 diabetes-associated metabolic perturbations in saliva, blood and urine at different timescales of glycaemic control. Diabetologia 58(8):1855–1867. https://doi.org/10.1007/s00125-015-3636-2
Sakanaka A, Kuboniwa M, Katakami N et al (2021) Saliva and plasma reflect metabolism altered by diabetes and periodontitis. Front Mol Biosci 8:742002. https://doi.org/10.3389/fmolb.2021.742002
Andriankaja OM, Jiménez JJ, Muñoz-Torres FJ, Pérez CM, Vergara JL, Joshipura K (2015) Lipid lowering agents use and systemic and oral inflammation in overweight or obese adult Puerto Ricans: the San Juan Overweight Adults Longitudinal Study (SOALS). J Clin Periodontol 42(12):1090–1096. https://doi.org/10.1111/jcpe.12461
Landale NS, Oropesa RS (2002) White, Black, or Puerto Rican? Racial self-identification among mainland and island Puerto Ricans. Social Forces 81(1):231–254. https://doi.org/10.1353/sof.2002.0052
Paffenbarger RS, Wing AL, Hyde RT (1995) Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol 142(9):889–903. https://doi.org/10.1093/oxfordjournals.aje.a117736
Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24(4):385–396. https://doi.org/10.2307/2136404
ElSayed NA, Aleppo G, Aroda VR et al (2023) 2. Classification and diagnosis of diabetes: standards of care in diabetes-2023. Diabetes Care 46(Suppl 1):S19–S40. https://doi.org/10.2337/dc23-S002
Henson BS, Wong DT (2010) Collection, storage, and processing of saliva samples for downstream molecular applications. Methods Mol Biol 666:21–30. https://doi.org/10.1007/978-1-60761-820-1_2
Evans AM, DeHaven CD, Barrett T, Mitchell M, Milgram E (2009) Integrated, nontargeted ultrahigh performance liquid chromatography/electrospray ionization tandem mass spectrometry platform for the identification and relative quantification of the small-molecule complement of biological systems. Anal Chem 81(16):6656–6667. https://doi.org/10.1021/ac901536h
Friedman J, Hastie T, Tibshirani R (2010) Regularization paths for generalized linear models via coordinate descent. J Stat Softw 33(1):1–22
Li J, Guasch-Ferré M, Chung W et al (2020) The Mediterranean diet, plasma metabolome, and cardiovascular disease risk. Eur Heart J 41(28):2645–2656. https://doi.org/10.1093/eurheartj/ehaa209
Wang F, Baden MY, Guasch-Ferré M et al (2022) Plasma metabolite profiles related to plant-based diets and the risk of type 2 diabetes. Diabetologia 65(7):1119–1132. https://doi.org/10.1007/s00125-022-05692-8
Vangipurapu J, Fernandes Silva L, Kuulasmaa T, Smith U, Laakso M (2020) Microbiota-related metabolites and the risk of type 2 diabetes. Diabetes Care 43(6):1319–1325. https://doi.org/10.2337/dc19-2533
Lee S, Zhang C, Kilicarslan M et al (2016) Integrated network analysis reveals an association between plasma mannose levels and insulin resistance. Cell Metabolism 24(1):172–184. https://doi.org/10.1016/j.cmet.2016.05.026
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Acknowledgements
The authors thank all SOALS participants and staff for their contribution to this study. Part of this study was presented as an abstract at the virtual Metabolomics Society 2021 conference, 22–24 June 2021.
Data availability
Data are available upon reasonable request. Information on requesting data from SOALS can be found on their website: http://soals.rcm.upr.edu/.
Funding
This work was supported by the National Institutes of Health: T32CA009001 (DEH), 1K01DK136968 (DEH) and R01DK120560-01 (DEH, LL, C-HL, DTWW, FBH, MJS, KJ and SNB) and the National Institute of General Medical Sciences [U54GM133807 (KG, CMP, EM-B, KJ)].
Authors’ relationships and activities
DTWW is a consultant to AIONCO and has equity in Liquid Diagnostics LLC. The authors declare that there are no other relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
DEH performed the statistical analyses. DEH and SNB drafted the manuscript. DEH, LL, KG, MM-L, CMP, C-HL, EM-B, CC, DTWW, JEM, FBH, MJS, KJ and SNB contributed to interpretation of the data and revised the article critically for important intellectual content. All authors approved the final version of the manuscript. DEH and SNB are guarantors of the work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Haslam, D.E., Liang, L., Guo, K. et al. Discovery and validation of plasma, saliva and multi-fluid plasma–saliva metabolomic scores predicting insulin resistance and diabetes progression or regression among Puerto Rican adults. Diabetologia (2024). https://doi.org/10.1007/s00125-024-06169-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00125-024-06169-6