Abstract
Aims/hypothesis
The aim of this study was to assess whether the addition of intermittently scanned continuous glucose monitoring (isCGM) to standard care (self-monitoring of blood glucose [SMBG] alone) improves glycaemic control and pregnancy outcomes in women with type 1 diabetes and multiple daily injections.
Methods
This was a multicentre observational cohort study of 300 pregnant women with type 1 diabetes in Spain, including 168 women using SMBG (standard care) and 132 women using isCGM in addition to standard care. In addition to HbA1c, the time in range (TIR), time below range (TBR) and time above range (TAR) with regard to the pregnancy glucose target range (3.5–7.8 mmol/l) were also evaluated in women using isCGM. Logistic regression models were performed for adverse pregnancy outcomes adjusted for baseline maternal characteristics and centre.
Results
The isCGM group had a lower median HbA1c in the second trimester than the SMBG group (41.0 [IQR 35.5–46.4] vs 43.2 [IQR 37.7–47.5] mmol/mol, 5.9% [IQR 5.4–6.4%] vs 6.1% [IQR 5.6–6.5%]; p=0.034), with no differences between the groups in the other trimesters (SMBG vs isCGM: first trimester 47.5 [IQR 42.1–54.1] vs 45.9 [IQR 39.9–51.9] mmol/mol, 6.5% [IQR 6.0–7.1%] vs 6.4% [IQR 5.8–6.9%]; third trimester 43.2 [IQR 39.9–47.5] vs 43.2 [IQR 39.9–47.5] mmol/mol, 6.1% [IQR 5.8–6.5%] vs 6.1% [IQR 5.7–6.5%]). The whole cohort showed a slight increase in HbA1c from the second to the third trimester, with a significantly higher rise in the isCGM group than in the SMBG group (median difference 2.2 vs 1.1 mmol/mol [0.2% vs 0.1%]; p=0.033). Regarding neonatal outcomes, newborns of women using isCGM were more likely to have neonatal hypoglycaemia than newborns of non-sensor users (27.4% vs 19.1%; ORadjusted 2.20 [95% CI 1.14, 4.30]), whereas there were no differences between the groups in large-for-gestational-age (LGA) infants (40.6% vs 45.1%; ORadjusted 0.73 [95% CI 0.42, 1.25]), Caesarean section (57.6% vs 48.8%; ORadjusted 1.33 [95% CI 0.78, 2.27]) or prematurity (27.3% vs 24.8%; ORadjusted 1.05 [95% CI 0.55, 1.99]) in the adjusted models. A sensitivity analysis in pregnancies without LGA infants or prematurity also showed that the use of isCGM was associated with a higher risk of neonatal hypoglycaemia (non-LGA: ORadjusted 2.63 [95% CI 1.01, 6.91]; non-prematurity: ORadjusted 2.52 [95% CI 1.12, 5.67]). For isCGM users, the risk of delivering an LGA infant was associated with TIR, TAR and TBR in the second trimester in the logistic regression analysis.
Conclusions/interpretation
isCGM use provided an initial improvement in glycaemic control that was not sustained. Furthermore, offspring of isCGM users were more likely to have neonatal hypoglycaemia, with similar rates of macrosomia and prematurity to those of women receiving standard care.
Graphical abstract

Similar content being viewed by others

Introduction
Despite improvements in glycaemic control during pregnancy, women with type 1 diabetes have a three- to fivefold greater risk of adverse perinatal and obstetric outcomes than the general obstetric population [1, 2]. In this context, the implementation of new technologies such as continuous glucose monitoring (CGM) could have a positive impact on maternal and neonatal morbidity, as shown in non-pregnant populations [3, 4].
Based on the results of the continuous glucose monitoring in pregnant women with type 1 diabetes (CONCEPTT) trial, CGM has been widely recommended for all pregnant women with type 1 diabetes in international guidelines [5, 6]. The CONCEPTT trial was the first RCT to demonstrate that the continued use of real-time continuous glucose monitoring (rtCGM) in pregnant women with type 1 diabetes led to a significant reduction in large-for-gestational-age (LGA) infants, neonatal hypoglycaemia and neonatal intensive care unit admissions [7]. However, in contrast to rtCGM, data from RCTs evaluating the effectiveness of the intermittent use of CGM for maternal and neonatal outcomes have yielded conflicting results [8,9,10]. While the study by Murphy et al found a decreased mean birthweight and a reduced risk of macrosomia in women randomised to intermittent use of retrospective CGM [9], the continuous glucose monitoring during diabetic pregnancy (GlucoMOMS) study failed to replicate these benefits years later [10]. Moreover, when rtCGM was used intermittently throughout pregnancy, outcomes were not improved either [8]. In 2018, intermittently scanned continuous glucose monitoring (isCGM, FreeStyle Libre system; Abbott, Alameda, CA, USA) was approved for use during pregnancy [11]. However, to date, the impact of isCGM on pregnancy outcomes has been rarely studied [12, 13]. In an observational cohort study including pregnant women using CGM, the rates of neonatal outcomes did not differ between isCGM and rtCGM users [12]. In addition, recent data from a small RCT (n = 34 women with type 1 diabetes) comparing isCGM with self-monitoring of blood glucose (SMBG) showed that isCGM did not improve neonatal outcomes [13].
Only the continued use of rtCGM has been demonstrated to have benefits for neonatal outcomes such as neonatal hypoglycaemia and neonatal intensive care unit admissions [7]; however, the economic burden of rtCGM systems on national health systems has limited their implementation. Indeed, in Spain, isCGM is the main government-funded CGM system for pregnant women with type 1 diabetes managed by multiple daily injection (MDI) therapy. Therefore, the aim of this study was to assess whether the addition of isCGM to standard care (monitoring by SMBG only) improves maternal glycaemic control and pregnancy outcomes in a cohort of women with type 1 diabetes managed by MDI therapy.
Methods
Study population
We performed an observational multicentre cohort study in women with type 1 diabetes attending seven tertiary university hospitals in Spain between 2012 and 2021. The inclusion criteria were (1) age >18 years; (2) type 1 diabetes; (3) MDI therapy; and (4) singleton pregnancy. Women with pregnancy loss before 20 weeks of gestation or women treated with an insulin pump were excluded from the analysis. There were no additional exclusion criteria. Information was obtained from a web-based Spanish national registry designed by the Spanish Diabetes and Pregnancy Study Group. A data manager supervised data entry to avoid errors and enable potential technical issues to be solved. All study members were encouraged to consecutively introduce data from all pregnant women with pregestational diabetes attending their centres. A chart review was conducted when missing data were detected. The study was approved by the ethics committee at each participating centre and all participants provided written informed consent.
Routine care
All women received routine clinical care, with antenatal visits every 2–4 weeks. In accordance with current national guidelines [14, 15], women were advised to perform SMBG both before and 1 or 2 h after meals, at bedtime and occasionally during the night. The goals were to achieve preprandial capillary glucose levels <5.3 mmol/l, 1 h postprandial capillary glucose levels <7.8 mmol/l or 2 h postprandial capillary glucose levels <6.7 mmol/l, and HbA1c levels <48 mmol/mol (<6.5%). HbA1c was measured every 4–8 weeks during pregnancy. One HbA1c measurement per trimester was selected as follows: at 10–14 weeks of gestation (first trimester), 24–28 weeks of gestation (second trimester) and 32–36 weeks of gestation (third trimester). If more than one HbA1c measurement was registered within these periods, the HbA1c value closest to the upper limit was selected. HbA1c analysis was performed in local laboratories according to standard procedures and values were standardised against the National Glycohemoglobin Standardization Program levels. ADA and National Institute for Health and Care Excellence (NICE) guidelines were used as a reference for the statistical analysis. ADA recommends an HbA1c value <48 mmol/mol (<6.5%) as the pre-pregnancy and first trimester target and a value <42 mmol/mol (<6.0%) in the second and third trimesters [5], while NICE recommends an HbA1c value <48 mmol/mol (<6.5%) in all trimesters [6].
Intervention with CGM
In addition to routine care, in Spain the use of isCGM has been reimbursed for all pregnant women with type 1 diabetes since 2018 [16, 17]. Thus, pregnant women with type 1 diabetes who were not already using a CGM device before pregnancy were offered an isCGM device at the first antenatal visit. The isCGM device used was the FreeStyle Libre system (Abbott), which measures subcutaneous interstitial glucose concentrations every 60 s and generates a glucose value every 15 min (with 96 recordings per day). The device requires no calibration by the user. The FreeStyle Libre 2 was implemented in June 2020, which, in contrast to the previous version, has optional alarms that warn the user in the case of hypoglycaemia or hyperglycaemia. National guidelines recommend setting the hypoglycaemia alarm at between 3.6 and 3.9 mmol/l in the first trimester and between 3.3 and 3.6 mmol/l in the second and third trimesters, and setting the hyperglycaemia alarm at between 8.9 and 10 mmol/l throughout pregnancy [15]. SMBG measurements were recommended prior to insulin dose adjustment or correction of hypoglycaemia to verify the accuracy of isCGM. Women were advised to achieve the same SMBG goals as the routine care group and, in addition, it was recommended that the percentage of time in range (TIR), time below range (TBR) and time above range (TAR) with regard to the pregnancy glucose target (3.5–7.8 mmol/l) were >70%, <4% and<25%, respectively [15]. The isGCM-related data for each pregnancy were obtained using the LibreView software (Abbott Diabetes Care, Alameda, USA; ambulatory glucose profile [AGP] report for 14 consecutive days) [18]. The isCGM data obtained included mean glucose level, percentage of time the sensor was active, and the percentage of TIR, TBR and TAR for each trimester of gestation. One AGP report was registered per trimester.
Maternal and neonatal data
We obtained baseline maternal data such as demographic characteristics, diabetes-related characteristics (severe hypoglycaemia episodes were defined as those requiring assistance from a third party), current smoking status, attendance at a pre-pregnancy care programme and folic acid supplementation at the first antenatal visit.
The primary outcome of interest was delivery of an LGA infant, which was defined as a birthweight above the 90th centile according to Spanish fetal growth charts that take into account sex and gestational age [19]. Gestational age at delivery was defined as the number of completed weeks based on the last menstrual period or on the earliest ultrasound assessment if discordant. The secondary outcomes evaluated were severe maternal hypoglycaemia during pregnancy (events requiring third-party assistance), pre-eclampsia (blood pressure 140/90 mmHg plus proteinuria >300 mg/day [20]), Caesarean section, preterm and early preterm delivery (delivery before 37 weeks and before 34 weeks, respectively), small-for-gestational-age (SGA) infant (birthweight <10th centile), macrosomia (birthweight ≥4000 g), neonatal hypoglycaemia (blood glucose level <2.2 mmol/l requiring treatment in the first 24 h after delivery [21]), respiratory distress (any distress requiring treatment), congenital anomalies, classified according to the European network of population-based registries for the epidemiological surveillance of congenital anomalies (EUROCAT) [22], and perinatal mortality (fetal and infant death from 20 weeks of gestation to 4 weeks after birth [23]).
Statistical analysis
Data are presented as means±SD, medians (IQR) or n values (percentage) unless indicated otherwise. The normal distribution of continuous variables was assessed using the Shapiro–Wilk test. Continuous data were compared using unpaired Student’s t tests and the Mann–Whitney test, according to data distribution, and categorical data were compared using the χ2 test. Wilcoxon and McNemar tests were used to evaluate changes throughout pregnancy for HbA1c and percentage achievement of HbA1c goals, respectively. Because of the observational design of this study, logistic regression analysis was fitted to characterise the strength of association between adverse pregnancy outcomes and the glucose monitoring system, including maternal age, pregestational BMI, current smoking status, centre, HbA1c level in the first trimester and gestational age at the first antenatal visit as independent variables. Thus, only adverse pregnancy outcomes with more than 60 events were selected for the logistic regression model. First trimester HbA1c level could be a reflection of baseline status rather than an effect of isCGM itself because of the high proportion of women who are naive to isCGM at the first antenatal visit; hence, this variable was included in the adjusted model. The regression models were not adjusted for intermediate variables such as HbA1c levels in the second and third trimesters, gestational age at delivery and maternal gestational weight gain at delivery [24]. However, it is known that LGA and preterm infants are more prone to neonatal hypoglycaemia [25, 26]; thus, a sensitivity analysis was performed in groups without preterm and LGA infants. Moreover, as the study period ranged from 2011 to 2021, and routine practice may have changed over time, a sensitivity analysis was performed to assess the rates of adverse pregnancy outcomes according to year of delivery.
Finally, a subanalysis was performed among isCGM users. The Spearman correlation was performed to estimate the association between isCGM metrics (TIR, TAR and TBR) and HbA1c. Logistic regression models were used to estimate ORs (95% CIs) for adverse pregnancy outcomes (LGA, prematurity, neonatal hypoglycaemia and Caesarean section). Variables included in the model were isCGM metrics, pregestational BMI and current smoking status. HbA1c was not included in the model because it was correlated with is CGM metrics.
Detailed information on missing data is provided in electronic supplementary material (ESM) Table 1. In the models, listwise deletion was applied (i.e. complete case analysis). All analyses were performed using Stata version 14.0 (Stata, College Station, TX, USA). A two-sided p value <0.05 was considered statistically significant. Based on the size of the cohort, our analyses had 80% power at the 5% level to detect a 16% difference in LGA rates between participants with or without isCGM use during pregnancy.
Results
Participant characteristics
A total of 300 pregnant women were included in the study, of whom 132 (44%) were isCGM users. The mean age of participants was 34.1±5.3 years and the median duration of diabetes was 16.0 (IQR 9.5–23.0) years, with no differences between the groups (Table 1). Among the isCGM group, 60.6% of users were CGM naive at the first antenatal visit and 10.6% of women were using the FreeStyle Libre 2 device. The median gestational age at which isCGM was initiated was 14.0 (IQR 8.9–20.0) weeks (data available for 51/80 women) and no woman discontinued isCGM use during pregnancy. As shown in Table 1, no differences were observed between groups in current smoking status, pregestational BMI, parity, rates of diabetes complications, folic acid use, pre-pregnancy care or rates of severe maternal hypoglycaemia. As expected, the number of isCGM users was highest in the last period considered (2020–2021).
Glycaemic control
The whole cohort showed a significant decrease in HbA1c levels from the pregestational period to the second trimester (median difference 8.7 [IQR 4.4–16.4] mmol/mol, 0.8% [IQR 0.4–1.5%]; p<0.001), with a slight increase from the second to the third trimester (median difference 1.1 [IQR −1.1–4.4] mmol/mol, 0.1% [IQR –0.1–0.4%]; p<0.001). The same pattern was observed in both groups throughout pregnancy, but HbA1c increased significantly more in the isCGM group than in the SMBG group from the second to the third trimester (median difference 2.2 [IQR −1.1–5.5] mmol/mol, 0.2% [IQR –0.1–0.5%], vs 1.1 [IQR −1.1–4.4] mmol/mol, 0.1% [IQR –0.1–0.4%]; p=0.033) (Fig. 1). When cross-sectional comparisons were made in each trimester, the isCGM group had a lower median HbA1c in the second trimester than the SMBG group (41.0 [IQR 35.5–46.4] mmol/mol vs 43.2 [IQR 37.7–47.5] mmol/mol; p=0.034). No differences were seen in the other periods (Table 1, Fig. 1).
HbA1c levels according to glucose monitoring system used and gestational age. First trimester: 10–14 weeks’ gestation; second trimester: 24–28 weeks’ gestation; third trimester: 32–36 weeks’ gestation. Data are median (IQR). *p<0.05 (SMBG vs isCGM); †p<0.05 for change in HbA1c levels between the second and third trimesters (SMBG vs isCGM)
Figure 2 shows the percentages of women meeting HbA1c targets according to international guidelines. When the NICE goals were applied, there were no trimester-specific differences in the percentages of women meeting HbA1c targets. However, when ADA goals were evaluated, significant differences were observed between groups in the second trimester (isCGM vs SMBG: 56.0% vs 42.6%; p=0.024), with a greater reduction from the second to the third trimester in the percentage of women meeting the target in the isCGM group than in the SMBG group (mean difference 19.6% vs 5.9%; p=0.034).
Percentage of women fulfilling HbA1c targets according to (a) NICE and (b) ADA criteria. The ADA recommends an HbA1c value <48 mmol/mol (<6.5%) as the pre-pregnancy and first trimester target and a value <42 mmol/mol (<6.0%) in the second and third trimesters. NICE recommends an HbA1c value <48 mmol/mol (<6.5%) in all trimesters. First trimester: 10–14 weeks’ gestation; second trimester: 24–28 weeks’ gestation; third trimester: 32–36 weeks’ gestation. *p=0.024 (SMBG vs isCGM); †p<0.05 for change over time (SMBG vs isCGM)
Pregnancy outcomes
The median gestational age at the first antenatal visit was 8.4 (IQR 6.9–10) weeks. There was no difference in this variable between the two glucose monitoring groups (Table 2). As shown in Table 2 (unadjusted analysis), there was also no significant difference in adverse pregnancy outcomes between groups. Nevertheless, when logistic regression was adjusted for well-known confounders (such as maternal age, centre, smoking status, pregestational BMI, HbA1c in the first trimester and gestational age at first antenatal visit), isCGM users had a higher risk of neonatal hypoglycaemia than those in the SMBG group (ORadjusted 2.20 [95% CI 1.14, 4.30]) (Fig. 3). The glucose monitoring system was not associated with LGA infants, prematurity or Caesarean section. In addition, a sensitivity analysis was performed for pregnancies without LGA or prematurity outcomes in the isCGM group; this gave the same results with regard to the frequency of neonatal hypoglycaemia (Table 3). Finally, the rates of adverse pregnancy outcomes were not significantly different throughout the study period (ESM Tables 2, 3).
Binary logistic regression models for the most prevalent adverse pregnancy outcomes including the SMBG group as the reference group. All models were adjusted for the same variables: maternal age, pregestational BMI, smoking status, centre, HbA1c in the first trimester and gestational age at the first antenatal visit
CGM-derived metrics among women with isCGM
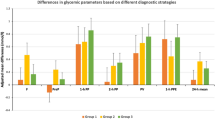
Figure 4 shows correlations between HbA1c and TAR, TIR and TBR with regard to the pregnancy glucose target range by trimester. HbA1c was directly correlated with TAR and inversely correlated with TIR and TBR throughout pregnancy.
Table 4 shows the changes in TIR, TAR and TBR throughout pregnancy. The percentage of TIR increased during pregnancy as the percentage of TAR decreased. However, TBR decreased from the first to the second trimester, with no significant changes in the third trimester. Finally, an exploratory analysis was performed to evaluate the relationship between TIR, TAR and TBR and the following adverse pregnancy outcomes: prematurity, Caesarean section, LGA infant and neonatal hypoglycaemia. After adjustment for confounders, metrics from the second trimester were associated with LGA birthweight (per 1% increase in TIR: ORadjusted 0.97 [95% CI 0.94, 0.99]; TAR: ORadjusted 1.05 [95% CI 1.02, 1.08]; and TBR: ORadjusted 0.76 [95% CI 0.65, 0.89]), and TBR in the first trimester was associated with prematurity (per 1% increase: ORadjusted 0.79 [95% CI 0.68, 0.93]) (ESM Table 4).
Discussion
In this multicentre cohort study, the addition of isCGM to SMBG in pregnancies complicated by type 1 diabetes was associated with lower HbA1c values in the second trimester, although this improvement was not sustained over time. We also found that offspring of pregnant women using isCGM were more likely to have neonatal hypoglycaemia, with no significant differences in other neonatal outcomes. To the best of our knowledge, this is the largest cohort study evaluating the effect on pregnancy of isCGM compared with current clinical practice (using SMBG alone) in women with type 1 diabetes treated with MDI therapy.
CGM systems extrapolate blood glucose concentrations from measurements of interstitial subcutaneous glucose and, thus, the accuracy and reliability of these systems are key factors. The accuracy and safety of isCGM (FreeStyle Libre 1) and user acceptability by pregnant women with diabetes have been demonstrated [11]. Nonetheless, although acceptable accuracy has been shown for estimates of interstitial glucose compared with reference blood glucose measurements (mean absolute relative difference of 11.8%), the discrepancy is more pronounced at the extremes of glucose ranges, in both pregnant and non-pregnant populations [27,28,29]. Indeed, despite similar mean sensor glucose values obtained with isCGM and rtCGM, more glucose readings were classified as TBR by isCGM in 20 pregnant women with type 1 diabetes in early pregnancy [28]. Overestimation of hypoglycaemia during pregnancy when tight glycaemic control is recommended could have clinical consequences. In fact, this could explain, in part, the greater increase in HbA1c from the second to the third trimester in isCGM users in our cohort. Insulin requirements are higher between weeks 24 and 34 of gestation [30]. However, women using isCGM who spend a large proportion of time (3–10%) below the target blood glucose range may be conflicted whether to prevent or treat hypoglycaemia (e.g. by snacking) and to change insulin doses. Furthermore, the international consensus on the use of CGM recommends that all pregnant women with type 1 diabetes spend <4% of their time below the target range, regardless of the CGM system used [18]. Thus, overestimation of the TBR by the isCGM system could lead to more conservative decision-making, not only by pregnant women themselves, but also by their physicians.
Surprisingly, unlike previous studies, our results show that isCGM use during pregnancy is associated with an increased risk of neonatal hypoglycaemia compared with SMBG alone. Only one previous RCT has compared isCGM with SMBG and no advantages were found for isCGM regarding HbA1c or TIR; however, the study was underpowered for neonatal outcomes because of the low number of participants included (n = 34 women with type 1 diabetes) [13]. In a larger cohort study from Sweden (n = 187), isCGM users were compared only with rtCGM users and no differences were found in pregnancy outcomes [12]. Interestingly, the rtCGM group had higher rates of insulin pump therapy. A prespecified analysis of the CONCEPTT study revealed that pump users were less likely to achieve HbA1c at a gestational age of 34 weeks and were also more likely to experience adverse neonatal outcomes (including neonatal hypoglycaemia) than MDI users [31]. Thus, the higher rates of insulin pump therapy among the rtCGM group in the Swedish study could have influenced the results, as the isCGM group was directly compared with a high-risk group. On the other hand, it has been found that high glucose levels during the peripartum period also play a role in neonatal hypoglycaemia [25, 26]. In our cohort, no between-group difference in HbA1c values in the third trimester was observed, but isCGM users started with significantly lower HbA1c levels in the second trimester, which leads to the hypothesis that further increases in glucose levels in the isCGM group could be present weeks/days before delivery, consequently leading to an increased risk of neonatal hypoglycaemia. Moreover, sensor use during intrapartum among isCGM users cannot be ruled out, with the subsequent risk of overestimation of hypoglycaemia in this period. In contrast, the lower HbA1c in the second trimester in the isCGM group could have prevented deleterious repercussions on fetal growth, for which glycaemic control is important not only at the end of pregnancy, but also throughout gestation [32]. Overall, these results highlight the need for tight glycaemic control until delivery.
Focusing on the isCGM cohort, CGM metrics improved throughout pregnancy (the percentages of women who achieved the target TIR >70% and target TAR <25% significantly increased from the first to the third trimester), unlike HbA1c, which showed higher levels in the third trimester than in the second trimester. This discrepancy between HbA1c and TIR has been described previously [33]. In the study by Kristensen et al, maternal HbA1c levels remained unchanged from the second to the third trimester, despite a 5% percentage point increase in TIR [12]. Similar discrepancies between third trimester HbA1c and improving TIR and TAR were observed in the CONCEPTT study [7]. In addition, a recent observational study showed an increase in HbA1c levels from the second to the third trimester (+1 mmol/mol), despite a 2% increase in TIR in this period [34]. Indeed, the authors suggested that pregnant women with type 1 diabetes should strive for a TIR >78% to achieve an HbA1c <42 mmol/mol, or a TIR >74% to achieve an HbA1c <48 mmol/mol. On the other hand, in the present study, CGM-derived metrics showed a strong correlation with HbA1c, especially with TAR and TIR, in all trimesters. Our results showed a slightly higher correlation than previous studies in this field (r=0.5–0.7 in the present study vs r=0.4–0.5 in the previous studies) [34, 35]. As well as with HbA1c, our data suggest an association of all three CGM metrics in the second trimester (TIR, TBR and TAR) with the risk of LGA infants. The relationship between metrics related to hyperglycaemia and LGA infants has previously been observed in both isCGM and rtCGM users and was confirmed by our results [12, 34, 36, 37]. Moreover, we found an inverse association of TBR with the risk of LGA and prematurity. Although previous studies failed to replicate the results [36, 37], Sibiak et al described a relationship between the glycaemic risk assessment diabetes equation score attributed to hypoglycaemia and LGA [36]. Nonetheless, TBR-related findings should be interpreted with caution because of overestimation of hypoglycaemia by the isCGM [28]. Taken together, these data support the role of maternal hyperglycaemia triggering excessive insulin production by the fetal pancreas.
Our study has some strengths and limitations. Among its strengths is its multicentre nature and size, including 300 pregnant women with type 1 diabetes treated with MDI therapy. To date, this is the largest cohort study evaluating the effect of isCGM during a critical period such as pregnancy in a real clinical setting. Most of the previous studies evaluating CGM in type 1 diabetes included not only women receiving MDI therapy but also those receiving pump therapy [10, 12, 36]. To increase sample homogeneity, we carefully selected only women treated with MDI therapy. Furthermore, these data were collected from university hospitals with expertise in both CGM systems and obstetric management of pregnant women with diabetes. In addition to well-known maternal risk factors, the adjusted logistic regression models included the centre of selection, because of the possible variation in clinical practices between centres.
Nonetheless, limitations should also be acknowledged. First, this was an observational study, which precludes making causal inferences. However, this study highlights the limitations observed in real clinical practice (such as higher HbA1c levels in the third trimester of gestation). On the other hand, the wide availability of the isCGM system for facilitating the self-management of glucose control in all pregnant women with type 1 diabetes means that it is practically and ethically difficult to perform a RCT comparing isCGM with standard care (SMBG alone). Second, the differences in year of delivery between the isCGM group and the control group may have had an impact on adverse pregnancy outcomes. However, national guidelines on the screening and diagnosis of neonatal hypoglycaemia in newborns of women with type 1 diabetes have not been modified in the last 15 years, suggesting that there were no major changes over the study period. Moreover, a sensitivity analysis was performed and ruled out a time effect. Third, the definition of neonatal hypoglycaemia is not uniform in published studies. In the present study neonatal hypoglycaemia was defined as glycaemia <2.2 mmol/l requiring treatment in the first 24 h after delivery, while in the CONCEPTT study it was defined as glycaemia requiring treatment with intravenous dextrose [7] and in the study by Kristensen et al it was defined as glycaemia <2.6 mmol/l >3 h after birth [12]. These differences make comparisons difficult and highlight the need for additional evidence in other populations to confirm the results observed. Fourth, evaluation of metabolic control between groups was performed using a single HbA1c measure per trimester. Using only one measure per trimester may not provide an accurate reflection of metabolic control in each trimester and, in addition, HbA1c measurements have limitations in pregnancy [38]. Nonetheless, HbA1c was correlated with the number of daily glucose scans [39] and is considered to be a robust predictor of adverse pregnancy outcomes [40]. In fact, for neonatal hypoglycaemia, HbA1c at 34 weeks of gestation was a better predictor than CGM metrics (AUC 0.68 for HbA1c vs 0.64 for TIR and TAR at 34 weeks of gestation) [40]. Finally, the frequency of SMBG is missing in both groups. Although this information may have helped to elucidate the percentage of decisions initiated only by the glucose sensor, this information is usually difficult to obtain except in RCTs [41, 42].
In conclusion, the addition of isCGM to standard care in pregnancies complicated by type 1 diabetes and MDI therapy provided an initial improvement in glycaemic control that was not sustained. This deterioration late in pregnancy could explain the higher risk of neonatal hypoglycaemia. Further studies are needed to confirm our results, including with the new version of isCGM (FreeStyle Libre 2) that is currently available. Nevertheless, for the time being, rtCGM should be the gold standard of CGM therapy in pregnant women with type 1 diabetes receiving MDI therapy.
Data availability
Data are available from the authors on request.
Abbreviations
- CGM:
-
Continuous glucose monitoring
- CONCEPTT:
-
Continuous glucose monitoring in pregnant women with type 1 diabetes trial
- isCGM:
-
Intermittently scanned continuous glucose monitoring
- LGA:
-
Large-for-gestational-age
- MDI:
-
Multiple daily injection
- NICE:
-
National Institute for Health and Care Excellence
- rtCGM:
-
Real-time continuous glucose monitoring
- SGA:
-
Small-for-gestational-age
- SMBG:
-
Self-monitoring of blood glucose
- TAR:
-
Time above range
- TBR:
-
Time below range
- TIR:
-
Time in range
References
Murphy HR, Bell R, Cartwright C et al (2017) Improved pregnancy outcomes in women with type 1 and type 2 diabetes but substantial clinic-to-clinic variations: a prospective nationwide study. Diabetologia 60(9):1668–1677. https://doi.org/10.1007/s00125-017-4314-3
Persson M, Norman M, Hanson U (2009) Obstetric and perinatal outcomes in type 1 diabetic pregnancies: a large, population-based study. Diabetes Care 32(11):2005–2009. https://doi.org/10.2337/dc09-0656
Bolinder J, Antuna R, Geelhoed-Duijvestijn P, Kröger J, Weitgasser R (2016) Novel glucose-sensing technology and hypoglycaemia in type 1 diabetes: a multicentre, non-masked, randomised controlled trial. Lancet 388(10057):2254–2263. https://doi.org/10.1016/S0140-6736(16)31535-5
Beck RW, Riddlesworth T, Ruedy K et al (2017) Effect of continuous glucose monitoring on glycemic control in adults with type 1 diabetes using insulin injections the diamond randomized clinical trial. JAMA J Am Med Assoc 317(4):371–378. https://doi.org/10.1001/jama.2016.19975
American Diabetes Association (2021) 14. Management of diabetes in pregnancy: standards of medical care in diabetes—2021. Diabetes Care 44(Supplement 1):S200–S210. https://doi.org/10.2337/DC21-S014
NICE (2020) Diabetes in pregnancy: management from preconception to the postnatal period. Overview. Available from www.nice.org.uk/guidance/ng3. Accessed 30 Nov 2021
Feig DS, Donovan LE, Corcoy R et al (2017) Continuous glucose monitoring in pregnant women with type 1 diabetes (CONCEPTT): a multicentre international randomised controlled trial. Lancet 390(10110):2347–2359. https://doi.org/10.1016/S0140-6736(17)32400-5
Secher AL, Ringholm L, Andersen HU, Damm P, Mathiesen ER (2013) The effect of real-time continuous glucose monitoring in pregnant women with diabetes a randomized controlled trial. Diabetes Care 36(7):1877–1883. https://doi.org/10.2337/dc12-2360
Murphy HR, Rayman G, Lewis K et al (2008) Effectiveness of continuous glucose monitoring in pregnant women with diabetes: randomised clinical trial. BMJ 337(7675):907–910. https://doi.org/10.1136/bmj.a1680
Voormolen DN, DeVries JH, Sanson RME et al (2018) Continuous glucose monitoring during diabetic pregnancy (GlucoMOMS): a multicentre randomized controlled trial. Diabetes Obes Metab 20(8):1894–1902. https://doi.org/10.1111/dom.13310
Scott EM, Bilous RW, Kautzky-Willer A (2018) Accuracy, user acceptability, and safety evaluation for the FreeStyle libre flash glucose monitoring system when used by pregnant women with diabetes. Diabetes Technol Ther 20(3):180–188. https://doi.org/10.1089/DIA.2017.0386/ASSET/IMAGES/LARGE/FIGURE2.JPEG
Kristensen K, Ögge LE, Sengpiel V et al (2019) Continuous glucose monitoring in pregnant women with type 1 diabetes: an observational cohort study of 186 pregnancies. Diabetologia 62(7):1143–1153. https://doi.org/10.1007/S00125-019-4850-0
Tumminia A, Milluzzo A, Festa C et al (2021) Efficacy of flash glucose monitoring in pregnant women with poorly controlled pregestational diabetes (FlashMom): a randomized pilot study. Nutr Metab Cardiovasc Dis 31(6):1851–1859. https://doi.org/10.1016/j.numecd.2021.03.013
Acosta D, Balsells M, Ballesteros M et al (2015) Asistencia a la gestante con diabetes. Guía de práctica clínica actualizada en 2014 [article in Spanish]. Avances en Diabetologia 31(2):45–59. https://doi.org/10.1016/j.avdiab.2014.12.001
Grupo Español de Diabetes y Embarazo (2021) Diabetes mellitus y embarazo. Guia de práctica clínica actualizada 2021 [article in Spanish]. Prog Obstet Ginecol 2022 65:35–41
Resolución del 26 abril de 2019, de la Dirección General de Cartera Básica de Servicios del Sistema Nacional de Salud y Farmacia del acuerdo de la Comisión de prestaciones, aseguramiento y financiación sobre el sistema de monitorización de glucosa mediante sensores (tipo flash) en adultos [web page in Spanish]. Available from www.sanidad.gob.es/gl/profesionales/prestacionesSanitarias/CarteraDeServicios/ContenidoCS/docs/Resolucionglucosadultos.pdf. Accessed 12 December 2021.
Servicio Canario de Salud (2018) Instrucción n.o 9/18 del Director del Servicio Canario de la Salud sobre procedimentos y requisites para la prescripción, administración, seguimiento y control de las bombas de infusión contínua de insulina y sistemas de monitorización continua de glucose [web page in Spanish]. Available from https://www3.gobiernodecanarias.org/sanidad/scs/content/197eacf7-a6ba-11e8-a347-637f0280f239/Instruccion_9_18.pdf. Accessed 7 January 2022
Battelino T, Danne T, Bergenstal RM et al (2019) Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care 42(8):1593–1603. https://doi.org/10.2337/DCI19-0028
Carrascosa Lezcano A, Ferrández Longás A, Yeste Fernández D et al (2008) Estudio transversal español de crecimiento 2008. Parte I: Valores de peso y longitud en recién nacidos de 26-42 semanas de edad gestacional [article in Spanish]. Anales de Pediatria 68(6):544–551. https://doi.org/10.1157/13123286
Brown MA, Lindheimer MD, de Swiet M, van Assche A, Moutquin J-M (2001) The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the international society for the study of hypertension in pregnancy (ISSHP). Hypertens Pregnancy 20(1):ix–xiv. https://doi.org/10.1081/PRG-100104165
Metzger BE, Persson B, Lowe LP et al (2010) Hyperglycemia and adverse pregnancy outcome study: neonatal glycemia. Pediatrics 126(6):e1545–e1552. https://doi.org/10.1542/PEDS.2009-2257
European Commission. EUROCAT. Available from https://eu-rd-platform.jrc.ec.europa.eu/eurocat_en. Accessed 30 Nov 2021
Chico A, Herranz L, Corcoy R et al (2016) Glycemic control and maternal and fetal outcomes in pregnant women with type 1 diabetes according to the type of basal insulin. Eur J Obstetr Gynecol Reprod Biol 206:84–91. https://doi.org/10.1016/j.ejogrb.2016.07.490
Ananth CV, Schisterman EF (2017) Confounding, causality, and confusion: the role of intermediate variables in interpreting observational studies in obstetrics. Am J Obstetr Gynecol 217(2):167–175. https://doi.org/10.1016/J.AJOG.2017.04.016
Yamamoto JM, Corcoy R, Donovan LE et al (2019) Maternal glycaemic control and risk of neonatal hypoglycaemia in type 1 diabetes pregnancy: a secondary analysis of the CONCEPTT trial. Diabet Med 36(8):1046–1053. https://doi.org/10.1111/dme.13988
Dashora U, Levy N, Dhatariya K, Willer N, Castro E, Murphy HR (2021) Managing hyperglycaemia during antenatal steroid administration, labour and birth in pregnant women with diabetes – an updated guideline from the Joint British Diabetes Society for Inpatient Care. Diabetic Medicine e14744. https://doi.org/10.1111/DME.14744
Sola-Gazagnes A, Faucher P, Jacqueminet S et al (2020) Disagreement between capillary blood glucose and flash glucose monitoring sensor can lead to inadequate treatment adjustments during pregnancy. Diabetes Metab 46(2):158–163. https://doi.org/10.1016/J.DIABET.2019.08.001
Nørgaard SK, Mathiesen ER, Nørgaard K, Ringholm L (2021) Comparison of glycemic metrics measured simultaneously by intermittently scanned continuous glucose monitoring and real-time continuous glucose monitoring in pregnant women with type 1 diabetes. Diabetes Technol Ther 23(10):665–672. https://doi.org/10.1089/DIA.2021.0109
Jafri RZ, Balliro CA, El-Khatib F et al (2020) A three-way accuracy comparison of the Dexcom G5, Abbott Freestyle libre pro, and senseonics eversense continuous glucose monitoring devices in a home-use study of subjects with type 1 diabetes. Diabetes Technol Ther 22(11):846–852. https://doi.org/10.1089/DIA.2019.0449
García-Patterson A, Gich I, Amini SB, Catalano PM, de Leiva A, Corcoy R (2010) Insulin requirements throughout pregnancy in women with type 1 diabetes mellitus: three changes of direction. Diabetologia 53(3):446–451. https://doi.org/10.1007/s00125-009-1633-z
Feig DS, Corcoy R, Donovan LE et al (2018) Pumps or multiple daily injections in pregnancy involving type 1 diabetes: a prespecified analysis of the CONCEPTT randomized trial. Diabetes Care 41(12):2471–2479. https://doi.org/10.2337/dc18-1437
Scott EM, Feig DS, Murphy HR, Law GR (2020) Continuous glucose monitoring in pregnancy: importance of analyzing temporal profiles to understand clinical outcomes. Diabetes Care 43(6):1178–1184. https://doi.org/10.2337/DC19-2527
Murphy HR (2019) Continuous glucose monitoring targets in type 1 diabetes pregnancy: every 5% time in range matters. Diabetologia 62(7):1123–1128. https://doi.org/10.1007/S00125-019-4904-3
Ling P, Yang D, Gu N et al (2021) Achieving the HbA1c target requires longer time in range in pregnant women with type 1 diabetes. J Clin Endocrinol Metab 106(11):e4309–e4317. https://doi.org/10.1210/CLINEM/DGAB502
Shah VN, Snell-Bergeon JK, Demmitt J et al (2021) Relationship between time-in-range, HbA1c and the glucose management indicator in pregnancies complicated by type 1 diabetes. Diabetes Technol Ther 23(12):783–790. https://doi.org/10.1089/DIA.2021.0093
Sibiak R, Gutaj P, Mrzewka-Rogacz B, Mantaj U, Wender-Ozegowska E (2022) Novel continuous glucose monitoring metrics and LGA risk; an exploratory retrospective cohort study in pregnancies with type 1 diabetes. Diabetes Technol Ther 24(1):42–53. https://doi.org/10.1089/dia.2021.0194
Law GR, Ellison GTH, Secher AL et al (2015) Analysis of continuous glucose monitoring in pregnant women with diabetes: distinct temporal patterns of glucose associated with large-for-gestational-age infants. Diabetes Care 38(7):1319–1325. https://doi.org/10.2337/dc15-0070
Nielsen LR, Ekbom P, Damm P et al (2004) HbA1c levels are significantly lower in early and late pregnancy. Diabetes Care 27(5):1200–1201. https://doi.org/10.2337/diacare.27.5.1200
Gomez-Peralta F, Dunn T, Landuyt K, Xu Y, Merino-Torres JF (2020) Flash glucose monitoring reduces glycemic variability and hypoglycemia: real-world data from Spain. BMJ Open Diabetes Res Care 8(1):e001052. https://doi.org/10.1136/BMJDRC-2019-001052
Meek CL, Tundidor D, Feig DS et al (2021) Novel biochemical markers of glycemia to predict pregnancy outcomes in women with type 1 diabetes. Diabetes Care 44(3):681–689. https://doi.org/10.2337/DC20-2360
Hásková A, Radovnická L, Petruželková L et al (2020) Real-time CGM is superior to flash glucose monitoring for glucose control in type 1 diabetes: the CORRIDA randomized controlled trial. Diabetes Care 43(11):2744–2750. https://doi.org/10.2337/DC20-0112
Nathanson D, Svensson AM, Miftaraj M, Franzén S, Bolinder J, Eeg-Olofsson K (2021) Effect of flash glucose monitoring in adults with type 1 diabetes: a nationwide, longitudinal observational study of 14,372 flash users compared with 7691 glucose sensor naive controls. Diabetologia 64(7):1595–1603. https://doi.org/10.1007/S00125-021-05437-Z/FIGURES/3
Acknowledgements
We are grateful to D. Pringle for her help in writing and editing of the manuscript.
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
VP, MJP, AM, MG, AMW, BV, NS, MDM and IV made substantial contributions to the conception or design of the work and the acquisition, analysis and interpretation of data. All authors participated in drafting the manuscript or revising it critically for important intellectual content. The final version of the manuscript was approved by all authors, who agree to be accountable for all aspects of the work. VP and IV are the guarantors of this work. They had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding
This research received no specific grants from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(PDF 147 kb)
Rights and permissions
About this article
Cite this article
Perea, V., Picón, M.J., Megia, A. et al. Addition of intermittently scanned continuous glucose monitoring to standard care in a cohort of pregnant women with type 1 diabetes: effect on glycaemic control and pregnancy outcomes. Diabetologia 65, 1302–1314 (2022). https://doi.org/10.1007/s00125-022-05717-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-022-05717-2