Abstract
This article offers an historical approach to exploring precision medicine’s potential for reducing health disparities in diabetes. It examines case studies from the twentieth-century USA, from early twentieth-century beliefs that Jews were most at risk of developing diabetes to claims in the 1980s that Native Americans, African Americans, Hispanic Americans and Asian Americans had the greatest likelihood of developing the disease. These case studies reveal that attempts to understand perceived health disparities have long tended to focus on the biology and behaviours of the unwell, while paying less attention to food security, workplace hazards, access to quality healthcare and other social determinants of health. The precision medicine initiative, I argue, has an opportunity to right this imbalance by leveraging the tools of big data to learn more not only about biomarkers but also about the social and physical environments in which people live and work.
Similar content being viewed by others
Introduction
No one questions that health disparities exist. Diabetes rates, for example, are clearly higher in certain populations than in others. Where disagreements abound is in how to explain the disparities: do answers rest primarily in the biology and behaviours of different populations we label ‘races’ or do social determinants of health (food security, affordable housing, financial stability, access to quality healthcare, clean water and air, workplace hazards) matter most [1]?
Precision medicine sits uncomfortably in this space. On the one hand, the promise of ‘the right therapy for the right person at the right time’ suggests a way to avoid generalisations about different racial groups, since the goal is to replace ethnic and racial categories with clinical subphenotypes and, ultimately, to move closer to the possibility of treating each person as an individual. Added to that, the use of big data to amass information about biology, lifestyle and environment has the potential to disrupt the divisions that have so often been erected between genes and environments, finally putting to rest remnants of the age-old battle over whether nature or nurture matters most. However, at least two problems stand in the way of precision medicine making a major contribution to the elimination of health disparities. The first is cost. Wherever one stands on whether precision medicine can ever be achieved, it is widely agreed that it will take a long time before this approach benefits those with limited resources, whether they live in the Global South or are struggling with underinsurance or lack of insurance in the USA. Precision medicine may thus exacerbate health disparities before it ever has the possibility of eliminating them [2,3,4,5].
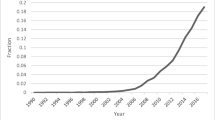
The second problem, which is the focus of this essay, is the outsized emphasis on the omic sciences that currently characterises precision medicine. Indeed, a PubMed search using ‘precision medicine’ and ‘social determinants of health’ turned up only 43 articles, although precision medicine alone had 43,004 hits. To be sure, nowhere does precision medicine deny the importance of non-biological factors. The first consensus report from the ADA and the EASD on precision medicine states explicitly its goal of ‘coupling’ what is learned about the ‘genetic and metabolic state’ of the disease with ‘detailed information about lifestyle and environment’ [6]. Even the 2011 National Research Council report, which explored the possibilities of precision medicine 4 years before President Obama announced the initiative, made a strong case for including information about ‘occupational hazards, exposure to industrial and household pollutants, water quality, climate, altitude, air pollution, and living conditions,’ as well as ‘social factors, such as socioeconomic status, quality of housing, neighbourhood, social relationships, access to services and experience of discrimination that can contribute to psychological stress, poor health, and health inequities’ [7]. Yet, this acknowledgement has not yet generated anywhere near the same level of interest and funding as is currently the case with the omic sciences. Surely, if the goal of precision medicine is to jettison the ‘one-size-fits-all’ approach to medicine, then far more needs to be known about the radically different material and social environments in which people live, work and face life’s many obstacles.
Historical perspective on health disparities: biomedical vs social approach
Precision medicine has the potential to reduce health disparities by enhancing our understanding of how biological, psychological, social and structural factors together impact health. The challenge is to ensure efforts expended to collect data about biomarkers are matched by efforts to collect data from the long list of factors identified in the National Research Council report. If precision medicine could strike this balance, it would be in a better position to provide insight into the complex constellation of factors driving health disparities and thus provide guidance on the best steps to eliminate them [8,9,10].
Charting this path will not be easy. For over a century there has been a preference in the USA and other western industrialised countries for biomedical approaches to improving health outcomes. This preference dates back to the successes of the bacteriological revolution, which led to the identification of bacterial causes of infectious diseases and the eventual development of vaccines and chemotherapeutic treatments. In the USA, this biomedical approach was enshrined in medical education and medical research in the 1910 Flexner Report, which signalled the beginning of substantial financial investments in the laboratory sciences, first by private entities like the Rockefeller and Carnegie Foundations, then, after World War II, by the US government and, increasingly, pharmaceutical and biotechnology industries [11,12].
The irony is that the rapid decline in mortality rates from infectious diseases during the early decades of the twentieth century, accompanied by a marked increase in life expectancy, was not the result of biomedical advances. Historians and demographers agree that improved nutrition and public health measures, such as the construction of sewer systems, filtered water supplies and indoor plumbing (i.e. measures that addressed social determinants of health), contributed most to the improved health outcomes [13]. It is also telling that such improvements were not experienced equally by all populations. Because of ongoing federal injustices and dispossessions, Native Americans and African Americans struggled disproportionately with food security and were rarely the beneficiaries of public health measures; they thus continued to die at comparatively young ages and to suffer disproportionately from infectious diseases well after White Americans lived long enough to develop chronic diseases such as cancer, cardiovascular disease, stroke and diabetes [14]. Much like today, the combination of limited access to biomedical advances and inequitable funding for measures that could improve people’s living and working conditions meant that Black and Native people continued to die at higher rates and at younger ages than people who were White [15].
Rather than ascribe high mortality rates from infectious diseases to impoverishment, food insecurity and the failure to extend public health improvements to all regions of the country, medical researchers and writers sought answers in biological differences between the races. That tendency persisted throughout the twentieth century, and it applied to chronic diseases as well. As the following case studies show, early twentieth-century claims that Jews were most at risk of developing diabetes and later claims that Native Americans, African Americans, Hispanic Americans and Asian Americans were the most susceptible attributed differential disease rates to the bodies and behaviours of the unwell. Arguments that social determinants of health also played a role surfaced from time to time but those voices struggled to be heard [16].
Diabetes as a Jewish disease in early twentieth-century USA
In the late nineteenth century, when US medical and public health experts first began to notice rapidly increasing diabetes rates, they also recognised that the disease did not afflict all populations equally. The renowned clinician, William Osler, commented in 1892 that ‘Hebrews seem especially prone to it’ [17]. Elliott P. Joslin agreed: an internationally renowned diabetes specialist in the first half of the twentieth century, he stated bluntly that ‘the frequency with which diabetes occurs in the Jewish is proverbial’ [18]. Even Jewish physicians concurred. In an article on diabetes mellitus in the Jewish Encyclopedia, the physician Maurice Fishberg and the anthropologist Joseph Jacobs wrote: ‘Statistics prove conclusively that the disease occurs among Jews from two to six times as frequently as it does among non-Jews’ [19].
Widespread acceptance of this health disparity did not, however, translate into a consensus about why Jews suffered disproportionately from diabetes. To some, answers were found in Jews’ racial makeup, the Jews at the time being widely regarded as a separate race. Embracing anti-Semitic sentiments, they blamed high rates on ‘some hereditary defect’, on Jews’ ‘racial tendency to corpulence’, and on ‘their neurotic temperament,’ which drew on a widespread belief at the time that diabetes was, fundamentally, a disease of the nervous system. Indeed, the alleged ‘primitivity’ of the nervous system of Black and Native peoples was presented as the reason rates of diabetes in these two populations seemed to be so low [17, 20,21,22].
Other physicians attributed high rates of diabetes to Jews’ lifestyle choices, rather than their biology. They wrote of Jews’ love for ‘high living’ and ‘parties’, ignoring the fact that the vast majority of Jews in the USA at the turn of the twentieth century could not yet afford luxury items, having only recently fled poverty and pogroms. Joslin was squarely in this camp, stating succinctly that Jews were not prone to develop diabetes because they were Jews but because they were fat. His advice to other physicians whose diabetes patients were fat, whether Jewish or not, was to use shame to get them to change their habits [23,24,25].
There was some resistance to these claims from Jewish physicians, who challenged the idea that either their hereditary makeup or their behaviours were primarily responsible for high rates of diabetes in their midst. Although their explanations never gained traction, they blamed the prevalence of diabetes in their community on the ‘oppression, privation, and every possible mental distress’ that Jews had faced ‘for many generations, year in and year out, from the cradle to the grave’ [26, 27]. Anti-Semitism, they argued, had made their nervous systems labile and had rendered them prone to develop nervous diseases. It followed that the way to reduce diabetes rates would be by eliminating anti-Semitism, not by pointing to hereditary defects or shaming people into losing weight.
My point is not that Jewish physicians were correct and others were wrong. After all, it remains unclear whether Jews did in fact suffer disproportionately from diabetes. The statistics available to the early twentieth-century medical community were too unreliable, a problem that was acknowledged at the time [26]. My point, rather, is that from the moment that rapidly increasing rates of diabetes were noticed, many assumed that perceived racial disparities in those rates could best be explained by biological and behavioural traits. Other explanations went largely unexplored.
Diabetes, ‘thrifty genes’ and Native Americans in post-war USA
A similar indifference to the social determinants of health was evident in the decades after World War II, when some of the highest rates of diabetes in the world were discovered among Native American tribes. To be sure, there were researchers, including the epidemiologist Kelly West, who placed importance on studying both genetic and environmental causes of high rates but genetics ended up dominating research efforts. An early and influential example of the privileging of genetic causes can be seen in the work of the Canadian human geneticist, David L. Rimoin, who began in the 1960s to think of diabetes mellitus as a genetically heterogeneous group of disorders. Rimoin had become curious about the reasons for the clinical variability he observed in the presentation of diabetes in different ethnic groups. Based on a comparative study he conducted of Amish people and the Dineh (Navajo), he concluded that diet could not account for differences in either vascular complications or the ability to tolerate high blood glucose concentrations and that diabetes in these two populations most likely differed genetically [28,29,30].
Two points need to be made. First, although Rimoin set out to compare genetics and the environment, he, like other researchers at the time, equated the environment with diet alone. The only data he collected, therefore, were on the foods that his study groups consumed. When diet failed to account for the clinical differences he observed, he concluded that the answer had to rest in genetics. Second, although Rimoin studied two distinct populations, he considered the Amish to be representative of Europeans and the Dineh to be representative of Native Americans. Other scholars interpreted his work in the same way. Thus, to Max Miller, Peter Bennett and Thomas Burch, three leading figures in the study of diabetes among the Akimel O’odham (Pima) people, Rimoin’s publications supported the possibility that the genetic mechanisms underlying diabetes differed ‘in the American Indian from those observed in the Caucasian’ [31].
Rimoin’s work, however, had suggested no such thing. All he had really shown was that diet could not explain the observed clinical differences in how diabetes presented itself in the Dineh and the Amish. Still, it did not take long before the idea took hold that Native Americans were at high risk of developing diabetes because of their genetic makeup. This not only downplayed the importance of studying non-genetic contributions but it also ignored the wide variation in diabetes rates (and genetic traits) among individuals of Native American ancestry.
Eventually, it became common to read of Native Americans’ possession of a ‘thrifty genotype’. This phrase referred to the work of the geneticist James Neel who had sought to explain how a deleterious trait (a diabetic genotype) could have attained such a high frequency in the human gene pool. His answer, which he published in 1962, built on what he knew about the evolutionary advantages that sickle cell provided populations that lived in regions where malaria thrived [32]. Neel thus hypothesised that a ‘thrifty genotype’ might have helped early humans as they lived through cycles of feast and famine by increasing the efficiency with which they stored fat when food was abundant. Such ‘efficient’ fat storers would be better able to survive periods of famine, thus making it more likely that they would reproduce. Only when food became consistently available did this efficiency become a liability. Neel said nothing, however, about Native Americans. He was not thinking of specific populations but, rather, of the entire human race.
As with Jews, there were challenges to the claim that genetics best explained high rates of diabetes among Native peoples. As the Indian rights movement gained strength in the 1970s, Native activists blamed high diabetes rates on White settler colonialism and the demise of traditional foodways. They were not so much denying the possibility of a genetic predisposition but were shifting attention to the actions of ‘so-called civilised’ White people, who had stolen Native lands [33, 34]. The Akimel O’odham (Pima) people, who have some of the highest rates of diabetes in the world, drew particular attention. This once prosperous tribe had grown much of their own food, relying on the Gila River to irrigate its lands until, in the words of one activist, ‘White settlers dammed and diverted the flow of the Gila River, making an agricultural existence impossible’ [35]. The result was mass starvation and dependence on government rations, which consisted primarily of flour, lard, coffee, sugar, salt, tobacco, beef and salt pork. For Native activists, then, high rates of diabetes were not best explained by thrifty genes or poor lifestyle choices but by ‘new diets, economic disaster, and social stress’ [36].
The Native American example, like the Jewish example, brings home how easily assumptions can drive decisions about what data to collect, which then shapes possible conclusions. Why should environment be defined solely by diet and why, when diet did not explain clinical variability, did Rimoin not consider social determinants of health, insisting instead that the answer had to rest in genetics? The notion that the destruction of Native lands had radically altered the lived experiences of Native peoples never even occurred to him, being too far removed from the biomedical framework in which he had been trained and at which he excelled.
That different populations vary in their genetic predispositions to certain diseases is not in question. However, as Rimoin’s work shows, assumptions about racial belonging can influence how those populations are defined. Whatever genetic differences might have separated the Dineh and the Amish, Rimoin made a leap by extrapolating from his study of these two populations a claim about genetic differences between Native Americans and Europeans. What thus began as an open exploration into the relative importance of genes and the environment in explaining differential diabetes rates slowly became ‘evidence’ of what was already believed: that the genetics of Native Americans and Europeans differed in fundamental ways.
The US government addresses health disparities, 1985
Biomedical research into the bodies of people who are unwell, rather than on social determinants of health, was securely in place by 1985, when the US government commissioned its first substantive study of the nation’s health disparities. The study was the brainchild of Margaret Heckler (US Secretary of Health and Human Services) and Thomas Malone (Deputy Director of the National Institutes of Health). These government officials had noticed that the health of Americans overall was improving but that not all populations were benefitting equally. They thus established a taskforce and charged it with determining the extent of health disparities in the nation, identifying the main reasons these disparities persisted, and proposing actions to eliminate them [37, 38].
To make the project manageable, the 19-member committee focused its attention on six conditions with the greatest health disparities among four racial groups (Black Americans, Native Americans, Hispanic Americans and Asian Americans). According to the nephrologist, Sandra L. Gadson, the resulting report, which ran to ten volumes, sent shockwaves through the nation [39]. What most disturbed readers was not that health disparities existed but that they were so severe long after the Civil Rights Movement had fought to extend the same rights and privileges to all Americans that most White Americans took for granted. One lasting result of this report was the establishment of the US government’s Office of Minority Health, which had the goal of eliminating health disparities [38].
The Heckler Report, as it came to be called, confined its discussion of social determinants of health to just a few pages in the first volume. Therein, the authors touched upon the effects that nutrition and diet, exposure to environmental hazards at home and work, and patterns of coping with stress had on an individual’s health. They also mentioned higher levels of unemployment and poverty among minority-ancestry families as compared with White families. Yet few of these insights were included in the more substantive volumes in which the taskforce explored the six health conditions in detail. Instead, the taskforce kept its focus largely on bodies and behaviours. In the volume on diabetes, moreover, different risk factors were highlighted for each of the different minority populations under study: genetics was mentioned only in the sections on Native Americans and Hispanic Americans; diet appeared only in the sections on Native Americans and Asian Americans; and psychosocial factors received mention only in the section on Asian Americans.
Since the taskforce’s report was formatted as a literature review, it was dependent on prior research. However, by merely synthesising past research instead of applying a critical eye, the review reinforced the legitimacy of racial groupings and ignored the great diversity within these populations. It also failed to acknowledge topics that had remained unexplored in the past. Others, however, were not so blind. Edith Irby Jones, the president of the National Medical Association, resented the report’s suggestion that Black people simply had to make better choices in order to solve their health problems. She wanted recognition that ‘poverty, neglect, underlying prejudices and the resulting stress’ produce ill health. If the government was truly interested in eliminating health disparities, Jones argued, it needed to invest in ‘better nutrition in early life, better housing, and more and better jobs’ [40]. However, that was not the focus of the report. Instead, the government’s first concerted effort to declare health disparities a national priority was centred on biomedical and behavioural research, not neighbourhood health centres, public health campaigns or anti-poverty and anti-racist measures.
Conclusion
Those funding the precision medicine initiative stand at a crossroad. They can continue to invest most heavily in the omic sciences, lured by the promise that advances in molecular biology and data science can together make it possible to develop targeted therapies. The results are sure to be impressive, and may very well open new markets, which explains the great interest of pharmaceutical and biotechnology industries. But for the reasons put forth in this essay, this research alone is unlikely to benefit people whose health problems are constantly aggravated by the social and physical environments in which they live and work. If, therefore, the goal is to reduce health disparities, then funding must be extended to research that studies the lived experiences of those who are sick.
There needs to be more interest in leveraging the tools of big data to learn more about home environments, neighbourhoods and workplaces. Information about food security and financial stability needs to be considered as important as information about biomarkers. The rejection of the ‘one-size-fits-all’ approach to medical treatment needs to be extended to the recognition that people differ not only biologically but also with respect to where and how they spend their days. Not everyone has access to the same resources. People face different obstacles when they try to make healthy choices. Furthermore, poverty and racism pose some of the greatest challenges to good health [1].
History provides an opportunity to place these tensions in context. Precision medicine sits at the end of over a century of biomedical advances that have improved the lives of some but not all. This foregrounding of biomedical research has taken place alongside inadequate funding for measures that would tackle social determinants of health. Throughout history, there have been people who have tried to direct attention away from an emphasis on the bodies and behaviours of the sick and toward policies that would improve the conditions in which people live and work. Such a balance is necessary if we are to be serious about eliminating health disparities.
References
Hill-Briggs F, Adler NE, Berkowitz SA et al (2020) Social determinants of health and diabetes: a scientific review. Diabetes Care 44(1):258–279 https://doi-org.proxy.library.vanderbilt.edu/10.2337/dci20-0053
Burke W, Trinidad SB, Schenck D (2019) Can precision medicine reduce the burden of diabetes? Ethn Dis 29(Suppl 3):669–674. https://doi.org/10.18865/ed.29.S3.669
Khoury MJ, Galea S (2016) Will precision medicine improve population health? JAMA 316(13):1357–1358. https://doi.org/10.1001/jama.2016.12260
Matthew DB (2019) Two threats to precision medicine equity. Ethn Dis 29(Suppl 3):629–640. https://doi.org/10.18865/ed.29.S3.629
Konkel L (2020) Who Will Benefit from Precision Medicine? UCSF Magazine Winter: 1–19
Chung WK, Erion K, Florez JC et al (2020) Precision medicine in diabetes: a consensus report from the American Diabetes Association (ADA) and the European Association for the Study of diabetes (EASD). Diabetes Care 43(7):1617–1635. https://doi.org/10.2337/dci20-0022
National Research Council (US) Committee on A Framework for Developing a New Taxonomy of Disease. Toward Precision Medicine: Building a Knowledge Network for Biomedical Research and a New Taxonomy of Disease. Washington (DC): National Academies Press (US); 2011. PMID: 22536618, Box 3–1, p 44
Burris HH, Wright CJ, Kirpalani H et al (2019) The promise and pitfalls of precision medicine to resolve black-white racial disparities in preterm birth. Pediatr Res 87(2):221–226. https://doi.org/10.1038/s41390-019-0528-z
Parikh RB, Jain SH, Navathe AS (2019) The sociobehavioral phenotype: applying a precision medicine framework to social determinants of health. Am J Manag Care 25(9):421–423
Kwon IG, Kim SH, Martin D (2021) Integrating social determinants of health to precision medicine through digital transformation: an exploratory roadmap. Int J Environ Res Public Health 18(9):5018. https://doi.org/10.3390/ijerph18095018
Starr P (1982) The social transformation of American medicine. Basic Books, New York
Porter R (1997) The greatest benefit to mankind. W. W. Norton & Company, New York
Colgrove J (2002) The McKeown thesis: a historical controversy and its enduring influence. Am J Public Health 92(5):725–729. https://doi.org/10.2105/ajph.92.5.725
Byrd W, Michael CL (2000–2002) An American Health Dilemma: Race, Medicine, and Health Care in the United States, 2 vols. New York, Routledge
Hammonds EM, Reverby SM (2019) Toward a historically informed analysis of racial health disparities since 1619. Am J Public Health 109(10):1348–1349. https://doi.org/10.2105/AJPH.2019.305262
Tuchman AM (2020) Diabetes: a history of race and disease. Yale University Press, New Haven
Osler W (1892) The principles and practice of medicine, 1st edn. D. Appleton, New York, p 275
Joslin EP (1917) The treatment of diabetes mellitus, 1st edn. Lea & Febiger, Philadelphia, p 46
Jacobs J, Fishberg M (1901–1906) Diabetes Mellitus. JewishEncyclopedia.com, https://www.jewishencyclopedia.com/articles/5161-diabetes-mellitus, accessed October 11, 2021
Wilson JG (1912) Increase in the death rate from diabetes—a possible explanation. Med Rec 82:662–663
Lees H (1936) Two million tightrope walkers. Collier’s May 16:34
Kleen E (1900) On diabetes mellitus and glycosuria. P. Blakiston’s Son & Co, Philadelphia, pp 15–19
Fitz RH, Joslin EP (1898) Diabetes mellitus at the Massachusetts General Hospital from 1824 to 1898. A study of the medical records. JAMA 31:165–171
Joslin EP (1924) The diabetic problem of today. JAMA 83:727–729. https://doi.org/10.1001/jama.1924.02660100001001
Joslin EP (1921) The prevention of diabetes mellitus. JAMA 76:79–84
Epstein AA (1919) Diabetes among Jews—its cause and prevention. Mod Med 1:269–275
(1925) Adiposity and other Etiological Factors in Diabetes Mellitus. JAMA 84: 1775–76
Rimoin DL (1967) Genetics of diabetes mellitus. Diabetes 16:346–351. https://doi.org/10.2337/diab.16.5.346
Rimoin DL (1969) Ethnic variability in glucose tolerance and insulin secretion. Arch Intern Med 124:695–700. https://doi.org/10.1001/archinte.1969.00300220047008
Rimoin DL, Saiki JH (1968) Diabetes mellitus among the Navajo. II. Plasma glucose and insulin responses. Arch Intern Med 122:6–9. https://doi.org/10.1001/archinte.1968.00300060008002
Miller M, Bennett PH, Burch TA (1968) Hyperglycemia in Pima Indians: A Preliminary Appraisal of Its Significance. In: Biomedical Challenges Presented by the American Indian. Washington, DC, Pan American Health Organization, 89–103
Neel JV (1962) Diabetes mellitus: a ‘thrifty’ gene rendered detrimental by ‘Progress’? Am J Hum Genet 14:363–362
(1980) Mike Myers—Excerpts from an Interview. Akwesasne Notes Sept;12: 23
(1982) Native People, Colonialism, and Food. Akwesasne Notes Mar;13: 24–25
(1974) New Hope in Health Care for Native Americans. Akwesasne Notes April;6 (April): 28
Smith-Morris C (2006) Diabetes among the Pima: stories of survival. University of Arizona Press, Tucson
U.S. Department of Health and Human Services. Report of the Secretary’s Task Force on Black & Minority Health (2006) (Heckler Report) Washington, DC, U.S. Government Printing Office
Gamble VN, Stone D (2006) U.S. policy on health inequities: the interplay of politics and research. J Health Polit Policy Law 31:93–126. https://doi.org/10.1215/03616878-31-1-93
Gadson SL (2006) Health equality: the new civil rights frontier. J Natl Med Assoc 98(3):324–329
Jones EI (1976) President’s column: closing the health status gap for blacks and other minorities. J Natl Med Assoc 78:485–488
Acknowledgements
I am grateful to L. Stark (Center for Medicine, Health, and Society, Vanderbilt University, USA) for her astute comments on an earlier draft of this manuscript.
Author’s relationships and activities
The author declares that there are no relationships or activities that might bias, or be perceived to bias, their work.
Funding
This research was funded by the American Council of Learned Societies, the National Institutes of Health (G13LM012252-01), and Vanderbilt University’s Office of the Provost (Research Scholars Grant Program).
Author information
Authors and Affiliations
Contributions
The author was the sole contributor to this paper.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tuchman, A.M. One size does not fit all: an historian’s perspective on precision diabetes medicine. Diabetologia 65, 1907–1912 (2022). https://doi.org/10.1007/s00125-022-05660-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-022-05660-2