Abstract
Aims/hypothesis
We previously showed that intrauterine exposure to gestational diabetes mellitus (GDM) increases selected markers of adiposity in pre-pubertal adolescents. In the present study, we examined these associations in adolescence, and explored whether they are strengthened as the participants transition through puberty.
Methods
Data from 597 individuals (505 unexposed, 92 exposed) participating in the longitudinal Exploring Perinatal Outcomes among Children (EPOCH) study in Colorado were collected at two research visits when the participants were, on average, 10.4 and 16.7 years old. Adiposity measures included BMI, waist/height ratio, and visceral and subcutaneous adipose tissue (as determined by MRI). Separate general linear mixed models were used to assess the longitudinal relationships between exposure to maternal GDM and each adiposity outcome. We tested whether the effect changed over time by including an interaction term between exposure and age in our models, and whether the associations were explained by postnatal behaviours.
Results
Compared with unexposed participants, those exposed to maternal GDM had higher BMI (β = 1.28; 95% CI 0.35, 2.21; p < 0.007), waist/height ratio (β = 0.03; 95% CI 0.01, 0.04; p = 0.0004), visceral adipose tissue (β = 4.81; 95% CI 1.08, 8.54; p = 0.01) and subcutaneous adipose tissue (β = 35.15; 95% CI 12.43, 57.87; p < 0.003). The magnitude of these differences did not change over time and the associations did not appear to be explained by postnatal behaviours.
Conclusions/interpretation
Our data provide further evidence that intrauterine exposure to maternal GDM is associated with increased offspring adiposity, an effect that appears early in life and tracks throughout adolescence. Efforts to prevent childhood obesity following intrauterine exposure to maternal GDM should target the prenatal or early life periods.
Similar content being viewed by others

Introduction
Over the last 50 years, the prevalence of overweight and obesity in youth has increased, with both conditions appearing at increasingly younger ages [1]. Obesity in childhood and adolescence is associated with long-term consequences, including more obesity [2], type 2 diabetes [3], and cardiovascular morbidity and mortality later in life [4]. Over the last two decades, the SEARCH for Diabetes in Youth study showed a rise in youth-onset type 2 diabetes [5], a condition that often occurs following obesity in childhood, suggesting that the early health risks associated with obesity can lead to long-lasting conditions in early adolescence.
Exposure to maternal gestational diabetes mellitus (GDM) during the intrauterine life leads to increased fetal growth, and fuel-mediated teratogenesis has been one of the suggested mechanisms responsible for fetal overnutrition [6] and its long-term consequences [7]. Positive associations have been observed between fetal exposure to maternal GDM and increased offspring BMI during childhood and adolescence [8,9,10,11,12,13,14,15,16]; however, less is known about the impact on fat patterning and distribution. The Exploring Perinatal Outcomes among Children (EPOCH) study is one of only a few studies that have incorporated more specific measures of adiposity and fat distribution. In 2011, Crume et al reported that exposure to maternal GDM is associated with more subcutaneous fat in mostly pre-pubertal children (mean age 10.5 years) [11]. In addition, few published studies have explored the association between exposure to maternal GDM and offspring adiposity longitudinally [13, 14] and none have explored whether the association strengthens as the participants transition through puberty. Puberty is a sensitive postnatal period of development that is characterised by many social and biological transitions. It is possible that this postnatal sensitive period may interact with fetal exposures, such as exposure to maternal GDM, and thereby either enhance or mitigate the risk of chronic diseases or their precursors.
This manuscript builds on previous work of the EPOCH study and explores the associations between exposure to maternal GDM and offspring adiposity throughout childhood and adolescence, using precise adiposity measures and longitudinally collected data. We also explored whether the magnitude of the associations changed over time as participants aged and transitioned through puberty. As secondary analyses, we examined whether the effect of intrauterine exposure to maternal GDM on offspring adiposity was partially explained by offspring behaviours or confounded by maternal pre-pregnancy BMI.
Methods
Study population
The EPOCH study is a historical, prospective, multiethnic cohort study that recruited 604 mother/child dyads in Colorado, selected based on their intrauterine exposure to maternal GDM status. Participants were offspring of singleton pregnancies, exposed or not exposed to maternal GDM in utero, born at a single hospital in Denver between 1992 and 2002, whose biological mothers were members of the Kaiser Permanente of Colorado (KPCO) Health Plan. More detailed information on the study population and methodology has been previously published [11]. Participants and their mothers were invited to participate in two research visits at mean ages of 10.4 (SD = 1.5) and 16.7 (SD = 1.2) years, at which time demographic, anthropometric and adiposity measures were collected and pubertal staging was assessed. The study was approved by the appropriate institutional review boards. Mothers provided written, informed consent and the children provided written assent.
Exposure definition
Exposure to maternal GDM was defined as a physician diagnosis of gestational diabetes during the index pregnancy. Diabetes status was ascertained from the KPCO perinatal database, an electronic database that links prenatal and neonatal medical records. All pregnant women at KPCO were routinely screened for GDM at 24–28 weeks using the two-step standard protocol [17]. GDM was diagnosed when two or more glucose values during the diagnostic 3 h 100 g OGTT met or exceeded the criteria for a positive test, as recommended by the National Diabetes Data Group [18]. Ninety-two mothers were diagnosed with GDM.
Adiposity outcomes
Offspring adiposity outcomes were evaluated during in-person research visits conducted by trained research staff at the University of Colorado Anschutz Medical Campus. The height and weight of the child were measured in light clothing and without shoes at each visit. Waist circumference was measured according to the National Health and Nutrition Examination Survey protocol [19]. BMI was calculated as weight (kg) divided by height (m) squared. Waist/height ratio (WHR) was calculated for each research visit as waist circumference divided by height, both measured in the same unit (cm). Visceral adipose tissue (VAT) and subcutaneous adipose tissue (SAT) were quantified by taking an MRI of the abdominal region with a 3 T HDx Imager (General Electric, Waukashau, WI, USA). The MRI was performed by a trained technician. Each study participant was in a supine position. A series of T1-weighted coronal images were taken to locate the L4/L5 plane. One axial, 10 mm, T1-weighted image, at the umbilicus or L4/L5 vertebrae, was analysed to determine SAT and VAT contents. MRI images were analysed by a single reader, blinded to exposure status.
Other measurements
Offspring age was calculated using the date of research visit minus the date of birth. The sex of the child was based on report from the mother, or self-report from the child. Race/ethnicity was self-reported at each research visit using the 2000 US Census base questions and categorised as Hispanic (any race), non-Hispanic white, non-Hispanic black or non-Hispanic other. For this analysis, we collapsed race/ethnicity into two race categories, non-Hispanic white and other, due to small sample sizes in the non-Hispanic black and non-Hispanic other categories. Pubertal development was self-reported by the offspring at each visit using diagrammatic representations of Tanner staging adapted from Marshall and Tanner [20]. Tanner stage (TS) 1–5 was classified on the basis of the appearance of pubic hair for males and the stage of breast development for females. We further categorised puberty into pre-pubertal (TS 1) and pubertal (TS 2–5). The participant’s diet at each visit was assessed using a modified version of the Block Kid’s Food Questionnaire, a semi-quantitative usual intake food frequency questionnaire developed specifically for participants aged 8 years and older [21]. In this analysis, we used energy from fat as a percentage of total daily energy intake as the variable of interest. Physical activity was obtained by self-report using a 3 day physical activity recall questionnaire, where questions based on key activities performed during the previous 3 days were queried. Results were reported as the mean number of 30 min blocks of vigorous activity per day. Maternal pre-pregnancy BMI was calculated from the KPCO-measured weight before the last menstrual cycle preceding pregnancy and height collected at the in-person research visit.
Statistical analysis
All individuals were eligible for the primary analysis, whereas only individuals who had diet and physical activity data or maternal pre-pregnancy BMI data were included in the secondary analyses. We computed descriptive statistics for exposed and unexposed, and used t tests and χ2 tests to compare the two groups. To test the effect of intrauterine exposure to maternal GDM on the offspring adiposity outcomes across the two research visits that span puberty, we fit separate general linear mixed models for the continuous outcomes of BMI, WHR, VAT and SAT. The models assumed an unstructured covariance matrix and included a random intercept. Use of mixed models for the purposes of our research questions is ideal as they appropriately account for correlations between the repeated adiposity measurements within the same participant, and they are more efficient than modelling change in the adiposity outcomes over time as they do not require that every participant has exactly the same number of repeated measurements and, thus, are suited to handling missing data [22]. We used Kenward–Roger df and the Wald F test to assess significance [23]. To test whether the effect of intrauterine exposure to maternal GDM on offspring adiposity changed over time, we used an interaction term between exposure and age. Due to possible differences in biological mechanisms, we additionally tested for effect modification of exposure status by sex, race/ethnicity and pubertal stage, by including appropriate interaction terms in each model. If interaction terms were not significant based on a p value <0.05, they were removed and models adjusted for the individual covariate terms. To examine modelling assumptions, variance inflation factors were calculated across model covariates, and Cook’s distance was used to pinpoint influential outliers. Jack-knifed studentised residuals were used to assess homoscedasticity and linearity. Adjusted β coefficients and corresponding 95% CIs were reported. Base models were adjusted for child’s age, sex, race/ethnicity and pubertal status, which were chosen a priori and were included in the model regardless of significance. For the secondary analyses, we added repeated measures of offspring behavioural covariates (daily 30 min blocks of vigorous physical activity and daily percentage of energy from fat) to the base model. We also explored the effect of maternal pre-pregnancy BMI on the association between exposure to maternal GDM and adiposity outcomes by adding maternal pre-pregnancy BMI to the base model.
Results
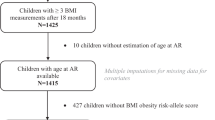
A total of 604 participants completed the first research visit and 418 participants completed the second research visit. We excluded seven child/mother dyads from the primary analysis due to exposure to type 1 diabetes; therefore, an analytic sample of 597 participants was used in the primary analysis. Mean ± SD ages of exposed and unexposed participants were 9.5 ± 1.7 and 10.6 ± 1.4 years for the first research visit, respectively (p < 0.001), and 15.9 ± 1.0 and 16.8 ± 1.5 years for the second research visit, respectively (p < 0.001). Compared with participants who only attended the first research visit (n = 597), those who attended both the first and second research visits (n = 411) were not significantly different in terms of race/ethnicity, sex or intrauterine exposure to diabetes (race/ethnicity: 48.1% vs 51.3%, p = 0.32; sex: 50.3% vs 50.1%, p = 0.95; exposure status: 15.4% vs 17.3%, p = 0.42, respectively). Of those who completed the first research visit, 15.4% of participants were exposed to maternal GDM compared with 17.3% in the second research visit. The distribution of sociodemographic characteristics was not significantly different between the primary and secondary analyses (diet and physical activity, n = 591; maternal pre-pregnancy BMI, n = 437; electronic supplementary material Table 1). Maternal and offspring characteristics by exposure status are summarised in Table 1.
On average, participants exposed to maternal GDM had significantly higher BMI (21.99 vs 20.71 kg/m2; β = 1.28; 95% CI 0.35, 2.21; p < 0.007), WHR (0.49 vs 0.46; β = 0.03; 95% CI 0.01, 0.04; p = 0.0004), VAT (31.00 vs 26.19 mm2; β = 4.81; 95% CI 1.08, 8.54; p = 0.01) and SAT (186.93 vs 151.78 mm2; β = 35.15; 95% CI 12.43, 57.87; p < 0.003) compared with unexposed participants (Table 2). The effect of exposure to maternal GDM did not change over time (exposure × age interaction: BMI, p = 0.94; WHR, p = 0.19; VAT, p = 0.34; SAT, p = 0.90). Child sex, race/ethnicity or pubertal status did not modify the association between exposure to maternal GDM and offspring adiposity (all interactions p > 0.05).
In our secondary analyses, we separately adjusted for postnatal behaviours (child’s physical activity and diet, assessed longitudinally) and additional confounders (maternal pre-pregnancy BMI). The magnitude of the association between exposure to maternal GDM and adiposity remained similar for all adiposity outcomes after adjusting for the offspring’s physical activity and diet (Table 3). When adjusting for maternal pre-pregnancy BMI, the associations between exposure to maternal GDM and adiposity were attenuated to non-significance, except for VAT (β = 6.36, p = 0.0008 vs β = 4.27, p = 0.02; Table 4).
Discussion
We aimed to explore the longitudinal association between intrauterine exposure to maternal GDM and levels of adiposity in a contemporary cohort of participants transitioning through puberty. We observed that participants exposed to maternal GDM had on average higher levels of BMI, WHR, VAT and SAT compared with those unexposed, and that these differences did not change over time as youth transitioned through puberty. The relationship between exposure to maternal GDM and increased offspring adiposity did not seem to be explained by postnatal behaviours, such as the offspring’s physical activity and diet. Adjustment for maternal pre-pregnancy BMI attenuated most of these associations, though the association with VAT remained statistically significant.
Most published studies exploring the association of exposure to maternal diabetes with offspring adiposity assess adiposity at a single time point [8,9,10,11,12,13, 15]. Two of the seven studies [11, 12] assessed adiposity once during childhood, prior to puberty, while the others [8,9,10, 13, 15] assessed adiposity at a single time point during or after puberty. We previously showed in this cohort that exposure to maternal GDM was associated with increased waist circumference and both VAT and SAT as early as 6 years of age [11]. This is around the same time that adrenarche typically begins, marking the start of the hormonal changes that occur later with puberty [24]. To our knowledge, no contemporary studies have examined the longitudinal effects of exposure to maternal diabetes on adiposity as offspring transition through puberty. Puberty is a complex physiological process defined by a period of intense hormonal changes and rapid physical growth, leading to psychological and physical maturation. Our current data also suggest that the effect of exposure on markers of adiposity does not change as youth transition through puberty.
Previous studies exploring the associations between intrauterine exposure to diabetes and offspring adiposity showed inconsistencies. Some have reported positive associations [8, 9, 11,12,13,14,15,16], while others reported some null associations [10, 25, 26]. The disagreement between studies may be due to the use of BMI as the sole marker of adiposity. BMI tends to be an imprecise measure of adiposity in growing youth [27,28,29]. In the present study, we observed an association between exposure to maternal GDM and several measures of adiposity, including BMI. However, we observed larger percentage differences between exposed and unexposed participants for more precise measures of adiposity related to abdominal fat deposition (VAT: 18% and SAT: 23%), compared with measures of overall adiposity (BMI: 6%). While the natural evolution of fat formation and deposition in children requires further study, it has been hypothesised that abdominal fat in pre-pubertal youth is mainly subcutaneous, whereas visceral fat increases with age and puberty and is influenced by sex [30]. In our study, exposure to maternal GDM was associated with a higher percentage difference between exposed and unexposed in SAT compared with VAT. Whether this difference continues into adulthood is unknown. Further research is needed to better understand the potential effects of exposure to maternal GDM on abdominal fat deposition throughout the life course. Nonetheless, these findings suggest that exposure to maternal GDM affects not only overall adiposity of the offspring, but also both central and peripheral fat disposition.
The magnitude of the association between exposure to maternal GDM and offspring adiposity outcomes remained similar when accounting for markers of offspring postnatal physical activity and diet, suggesting that the effect of maternal GDM operates independently of these behavioural choices. Recently, using the same cohort, Sauder et al showed that postnatal behaviours are important, but mostly act as effect modifiers in the relationship between exposure to maternal GDM and offspring markers of adiposity [31]. However, offspring physical activity and diet were self-reported, which may have introduced non-differential measurement error. Thus, future studies are needed to investigate the role of postnatal behaviours in the relationship between intrauterine exposure to GDM and offspring adiposity in childhood and adolescence using more objective measures of diet and physical activity.
We also explored the effect of additional adjustment for maternal pre-pregnancy BMI on the relationship between exposure to maternal GDM and offspring adiposity, albeit only in a subset with available data. Consistent with other studies [10, 15, 16, 32], adjustment for maternal pre-pregnancy BMI attenuated all associations, from 74.6% when the outcome was child BMI, to 32.9% when the outcome was VAT. Similar changes in the strength of associations between maternal GDM and child adiposity outcomes were observed in the much larger Hyperglycemia and Adverse Pregnancy Outcome Follow-up Study (HAPO FUS) study, where, after adjustment for maternal pre-pregnant BMI, the relationships remained statistically significant [32]. In addition, we argue that maternal pre-pregnancy BMI should not be conceptualised simply as a confounder [33]. Adjustment for maternal pre-pregnancy BMI may partly control for a competing mechanism, genetic predisposition to obesity shared by mother and offspring, which may be why the largest attenuation effect of adjustment was seen on the relationship between exposure and offspring BMI. However, maternal pre-pregnancy BMI is also a marker of the fetal overnutrition pathway explored here (i.e., elevated fuels, such as glucose and likely others) in the offspring of women with both obesity and diabetes during pregnancy [15, 34]. Thus, simply adjusting for maternal pre-pregnancy BMI may obscure, rather than isolate, the associations of interest. Prior studies have attempted to isolate the contribution of maternal genetic predisposition passed from mothers to offspring, either by using sib-pair designs with offspring born before and after GDM diagnosis in the mothers [35] or by directly controlling for offspring genetic risk score for obesity [36]. Both have concluded that the effect of exposure to GDM in utero on offspring adiposity does represent a specific intrauterine effect, above and beyond transmission of genetic susceptibility.
There are strengths and limitations in the present study. An important limitation is the fact that offspring adiposity markers were only obtained at two time points during a period of approximately 6 years, the period when our participants transitioned through puberty. This may have prevented us from detecting a statistically significant change in the strength of association between exposure and offspring adiposity markers over this period. Studies with a larger number of repeated adiposity measures during this developmental period are needed to definitively address this question. Another limitation is the difference in the proportion of Hispanics by exposure status. We addressed this by adjusting for several common co-occurring risk factors such as maternal health characteristics and socioeconomic factors that are more intrinsic to risk of developing GDM than race alone. Moreover, since Hispanic ethnicity is associated with higher GDM risk [37] and higher child BMI [1], and our exposed group had fewer Hispanic participants, any potential residual confounding in our analysis would serve to underestimate the associations between GDM exposure and child adiposity outcomes. Other limitations include the self-reported assessment of childhood diet, physical activity and TS. Important strengths are the prospective assessment of offspring adiposity markers, the inclusion of more specific measures of adiposity than child BMI alone and the objective assessment of intrauterine exposures from medical records.
In conclusion, our study suggests that the effects of fetal overnutrition (resulting from exposure to maternal GDM and obesity) on offspring adiposity are established early in life, likely before puberty, and track throughout adolescence. Future efforts to prevent childhood obesity should focus on the pre-conception and prenatal periods, and/or very early in the postnatal life.
Data availability
The data that support the findings of this study are available on request from the Principal Investigator (DD).
Abbreviations
- EPOCH:
-
Exploring Perinatal Outcomes among Children
- GDM:
-
Gestational diabetes mellitus
- KPCO:
-
Kaiser Permanente of Colorado
- SAT:
-
Subcutaneous adipose tissue
- TS:
-
Tanner stage
- VAT:
-
Visceral adipose tissue
- WHR:
-
Waist/height ratio
References
Ogden CL, Carroll MD, Lawman HG et al (2016) Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA 315(21):2292–2299. https://doi.org/10.1001/jama.2016.6361
Cunningham SA, Kramer MR, Narayan KMV (2014) Incidence of childhood obesity in the United States. N Engl J Med 370(5):403–411. https://doi.org/10.1056/NEJMoa1309753
Weiss R, Dziura J, Burgert TS et al (2004) Obesity and the metabolic syndrome in children and adolescents. N Engl J Med 350(23):2362–2374. https://doi.org/10.1056/NEJMoa031049
Sinha R, Fisch G, Teague B et al (2002) Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N Engl J Med 346(11):802–810. https://doi.org/10.1056/NEJMoa012578
Mayer-Davis EJ, Dabelea D, Lawrence JM (2017) Incidence trends of type 1 and type 2 diabetes among youths, 2002–2012. N Engl J Med 376(3):1419–1429. https://doi.org/10.1056/NEJMoa1610187
Freinkel N (1980) Banting lecture 1980. Of pregnancy and progeny. Diabetes 29(12):1023–1035. https://doi.org/10.2337/diab.29.12.1023
Clausen TD, Mathiesen ER, Hansen T et al (2009) Overweight and the metabolic syndrome in adult offspring of women with diet-treated gestational diabetes mellitus or type 1 diabetes. J Clin Endocrinol Metab 94(7):2464–2470. https://doi.org/10.1210/jc.2009-0305
Dabelea D, Hanson RL, Lindsay RS et al (2000) Intrauterine exposure to diabetes conveys risks for type 2 diabetes and obesity: a study of discordant sibships. Diabetes 49(12):2208–2211. https://doi.org/10.2337/diabetes.49.12.2208
Pettitt DJ, Baird HR, Aleck KA, Bennett PH, Knowler WC (1983) Excessive obesity in offspring of Pima Indian women with diabetes during pregnancy. N Engl J Med 308(5):242–245. https://doi.org/10.1056/NEJM198302033080502
Lowe WL, Scholtens DM, Lowe LP et al (2018) Association of gestational diabetes with maternal disorders of glucose metabolism and childhood adiposity. JAMA 320(10):1005–1016. https://doi.org/10.1001/jama.2018.11628
Crume TL, Ogden L, West NA et al (2011) Association of exposure to diabetes in utero with adiposity and fat distribution in a multiethnic population of youth: the Exploring Perinatal Outcomes among Children (EPOCH) study. Diabetologia 54(1):87–92. https://doi.org/10.1007/s00125-010-1925-3
Page KA, Romero A, Buchanan TA, Xiang AH (2014) Gestational diabetes mellitus, maternal obesity, and adiposity in offspring. J Pediatr 164(4):807–810. https://doi.org/10.1016/j.jpeds.2013.11.063
Lawlor DA, Lichtenstein P, Långström N (2011) Association of maternal diabetes mellitus in pregnancy with offspring adiposity into early adulthood: sibling study in a prospective cohort of 280,866 men from 248,293 families. Circulation 123(3):258–265. https://doi.org/10.1161/CIRCULATIONAHA.110.980169
Pitchika A, Vehik K, Hummel S et al (2018) Associations of maternal diabetes during pregnancy with overweight in offspring: results from the prospective TEDDY study. Obes Silver Spring Md 26(9):1457–1466. https://doi.org/10.1002/oby.22264
Gillman MW, Rifas-Shiman S, Berkey CS, Field AE, Colditz GA (2003) Maternal gestational diabetes, birth weight, and adolescent obesity. Pediatrics 111(3):e221–e226. https://doi.org/10.1542/peds.111.3.e221
Lawlor DA, Fraser A, Lindsay RS et al (2010) Association of existing diabetes, gestational diabetes and glycosuria in pregnancy with macrosomia and offspring body mass index, waist and fat mass in later childhood: findings from a prospective pregnancy cohort. Diabetologia 53(1):89–97. https://doi.org/10.1007/s00125-009-1560-z
American Diabetes Association (2015) 2. Classification and diagnosis of diabetes. Diabetes Care 38(Suppl1):S8–S16. https://doi.org/10.2337/dc15-S005
National Diabetes Data Group (1979) Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. Diabetes 28(12):1039–1057. https://doi.org/10.2337/diab.28.12.1039
Centers for Disease Control and Prevention (2007) Anthropometry procedures manual. In: National Health and Nutrition Examination Survey (NHANES) 2007–2008 Procedure Manuals. Available from httpwwwn.cdc.gov/nchs/data/nhanes/2007-2008/manuals/manual_an.pdf. Accessed 15 April 2019
Marshall WA, Tanner JM (1968) Growth and physiological development during adolescence. Annu Rev Med 19(1):283–300. https://doi.org/10.1146/annurev.me.19.020168.001435
Cullen KW, Watson K, Zakeri I (2008) Relative reliability and validity of the Block Kids Questionnaire among youth aged 10 to 17 years. J Am Diet Assoc 108(5):862–866. https://doi.org/10.1016/j.jada.2008.02.015
Demidenko E (2004) Mixed models: theory and applications, 1st edn. Wiley-Interscience, Hoboken. https://doi.org/10.1002/0471728438
Kenward MG, Roger JH (1997) Small sample inference for fixed effects from restricted maximum likelihood. Biometrics 53(3):983–997. https://doi.org/10.2307/2533558
Sperling MA (2014) Pediatric endocrinology. Elsevier Health Sciences, Philadelphia
Whitaker RC, Pepe MS, Seidel KD, Wright JA, Knopp RH (1998) Gestational diabetes and the risk of offspring obesity. Pediatrics 101(2):E9. https://doi.org/10.1542/peds.101.2.e9
Wright CS, Rifas-Shiman SL, Rich-Edwards JW, Taveras EM, Gillman MW, Oken E (2009) Intrauterine exposure to gestational diabetes, child adiposity, and blood pressure. Am J Hypertens 22(2):215–220. https://doi.org/10.1038/ajh.2008.326
Rothman KJ (2008) BMI-related errors in the measurement of obesity. Int J Obes 32(S3):S56–S59. https://doi.org/10.1038/ijo.2008.87
Brambilla P, Bedogni G, Moreno LA et al (2006) Crossvalidation of anthropometry against magnetic resonance imaging for the assessment of visceral and subcutaneous adipose tissue in children. Int J Obes 30(1):23–30. https://doi.org/10.1038/sj.ijo.0803163
Brambilla P, Bedogni G, Heo M, Pietrobelli A (2005) Waist circumference-to-height ratio predicts adiposity better than body mass index in children and adolescents. Int J Obes 37(7):943–946. https://doi.org/10.1038/ijo.2013.32
Fox KR, Peters DM, Sharpe P, Bell M (2000) Assessment of abdominal fat development in young adolescents using magnetic resonance imaging. Int J Obes Relat Metab Disord 24(12):1653–1659. https://doi.org/10.1038/sj.ijo.0801464
Sauder K, Bekelman T, Harrall K, Glueck D, Dabelea D (2019) Gestational diabetes exposure and adiposity outcomes in childhood and adolescence: an analysis of effect modification by breastfeeding, diet quality, and physical activity in the EPOCH study. Pediatr Obes. https://doi.org/10.1111/ijpo.12562
Lowe WL, Lowe LP, Kuang A et al (2019) Maternal glucose levels during pregnancy and childhood adiposity in the Hyperglycemia and Adverse Pregnancy Outcome Follow-up Study. Diabetologia 62(4):598–610. https://doi.org/10.1007/s00125-018-4809-6
Perng W, Okin E, Dabelea D (2019) Developmental overnutrition and offspring obesity and type 2 diabetes. Diabetologia. https://doi.org/10.1007/s00125-019-4914-1
Shapiro ALB, Schmiege SJ, Brinton JT et al (2015) Testing the fuel-mediated hypothesis: maternal insulin resistance and glucose mediate the association between maternal and neonatal adiposity, the Healthy Start study. Diabetologia 58(5):937–941. https://doi.org/10.1007/s00125-015-3505-z
Dabelea D (2007) The predisposition to obesity and diabetes in offspring of diabetic mothers. Diabetes Care 30(Suppl2):S169–S174. https://doi.org/10.2337/dc07-s211
Raghavan S, Zhang W, Yang IV et al (2017) Association between gestational diabetes mellitus exposure and childhood adiposity is not substantially explained by offspring genetic risk of obesity. Diabet Med 34(12):1696–1700. https://doi.org/10.1111/dme.13529
Hedderson MM, Darbinian JA, Ferrara A (2010) Disparities in the risk of gestational diabetes by race-ethnicity and country of birth. Paediatr Perinat Epidemiol 24(5):441–448. https://doi.org/10.1111/j.1365-3016.2010.01140.x
Acknowledgements
The authors thank the EPOCH participants, their families and the study staff for their dedicated contribution to this work.
Funding
This work was supported by the NIH National Institute of Diabetes, Digestive, and Kidney Diseases (R01 DK068001), and DHG was supported by the NIH National Institute of General Medical Sciences (R01GM121081, R25GM111901 and R25GM111901-S1). The contents are the authors’ sole responsibility and do not necessarily represent official NIH views. The funders had no role in the design, conduct or reporting of this work.
Author information
Authors and Affiliations
Contributions
DD conceptualised and designed the study. CWH and DD conceptualised the research questions, while CWH, DD, KKH, BMR, DHG designed the analyses and KH and CWH conducted the analyses. CWH wrote the first draft of the manuscript. KKH, BFM, APS, AB, KAS, WP, AS, KG, BMR, DHG and DD contributed to the interpretation of the paper and critically reviewed the manuscript for important intellectual content. All authors read and approved the final manuscript. DD is the guarantor of this work.
Corresponding author
Ethics declarations
The authors declare that there is no duality of interest associated with this manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 58 kb)
Rights and permissions
About this article
Cite this article
Hockett, C.W., Harrall, K.K., Moore, B.F. et al. Persistent effects of in utero overnutrition on offspring adiposity: the Exploring Perinatal Outcomes among Children (EPOCH) study. Diabetologia 62, 2017–2024 (2019). https://doi.org/10.1007/s00125-019-04981-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-019-04981-z