Abstract
In recent decades, large increases in diabetes prevalence have been demonstrated in virtually all regions of the world. The increase in the number of people with diabetes or with a longer duration of diabetes is likely to alter the disease profile in many populations around the globe, particularly due to a higher incidence of diabetes-specific complications, such as kidney failure and peripheral arterial disease. The epidemiology of other conditions frequently associated with diabetes, including infections and cardiovascular disease, may also change, with direct effects on quality of life, demands on health services and economic costs. The current understanding of the international burden of and variation in diabetes-related complications is poor. The available data suggest that rates of myocardial infarction, stroke and amputation are decreasing among people with diabetes, in parallel with declining mortality. However, these data predominantly come from studies in only a few high-income countries. Trends in other complications of diabetes, such as end-stage renal disease, retinopathy and cancer, are less well explored. In this review, we synthesise data from population-based studies on trends in diabetes complications, with the objectives of: (1) characterising recent and long-term trends in diabetes-related complications; (2) describing regional variation in the excess risk of complications, where possible; and (3) identifying and prioritising gaps for future surveillance and study.
Similar content being viewed by others
Background
In recent decades, large increases in diabetes prevalence have been demonstrated in virtually all regions of the world, with 415 million people worldwide now living with diabetes [1]. This is most concerning because an increase in diabetes prevalence will increase the number of chronic and acute diseases in the general population, with profound effects on quality of life, demand on health services and economic costs. Macrovascular complications of diabetes, including coronary heart disease, stroke and peripheral vascular disease, and microvascular complications, such as end-stage renal disease (ESRD), retinopathy and neuropathy, along with lower-extremity amputations (LEA), are responsible for much of the burden associated with diabetes. There is also growing recognition of a diversifying set of causally-linked conditions, including cancers, ageing-related outcomes (e.g. dementia), infections and liver disease. Since current data suggests that rates of all-cause and cardiovascular disease (CVD) mortality are decreasing in individuals with diabetes [2], trends in other complications of diabetes may become proportionately more prominent in the future.
Despite widespread international assessment of the growth of diabetes prevalence, quantification of the international burden and variation in the incidence of diabetes-related complications is notably lacking. This stems largely from the fact that data systems and population-based studies assessing diabetes complications are concentrated in Europe, North America and other high-income countries, with little to no availability in low- and middle-income countries, where the absolute increase in diabetes prevalence is largest. The lack of both uniform diagnosis of diabetes and of standardised measurement of diabetes-related complications has caused additional barriers in comparing trends worldwide. In this review, we synthesise data from adult population-based studies on trends in diabetes complications based on original articles, review articles and meta-analyses, with the objectives of: (1) characterising recent and long-term trends in diabetes-related complications; (2) describing regional variation in the excess risk of complications, where possible; and (3) identifying and prioritising gaps for future surveillance and study.
To this end, we conducted an extensive review of the literature in order to identify the majority of relevant publications. However, we did not adopt the formalities of a systematic literature review. Relevant publications were identified through a PubMed and Medline search using the following medical subject heading (MesH) terms: Diabetes Mellitus AND Diabetes Complications OR Mortality; End-Stage Renal Disease; Hyperglycaemia; Amputations; Cardiovascular Disease; Retinopathy; Nephropathy; Infections; Cancer; Dementia AND Epidemiology AND Trend. We also hand-searched reference lists of identified publications to determine additional eligible articles. The search was limited to papers in the English language. Throughout this Review, unless otherwise stated, data are reported among populations of people with diabetes, not general populations. All studies included were population-based, not clinic-based. Where more than one study per country (per outcome) existed, we chose the study reporting the most recent trends.
Macrovascular complications
CVD
CVD is a major cause of death and disability among people with diabetes. As the number of people with diabetes is predicted to increase, it is expected that the number of people with CVD will also increase [2]. However, data from several studies suggest that risk of CVD in people with diabetes has been declining since the 1990s (Table 1). Despite these improvements, people with diabetes continue to have a two- to fourfold higher risk of hospitalisation for major CVD events and CVD-associated clinical procedures compared with those without diabetes [2].
CVD mortality
Among the general population, mortality rates owing to CVD have declined in most high-income countries [12]. However, worldwide, CVD remains a leading cause of death in both people with and without diabetes [2, 13], and individuals with diabetes still have a two- to fourfold increased rate of CVD mortality compared with those without [14]. Data from several studies suggest a decline in CVD-associated mortality among people with diabetes.
In the USA, a 53% relative decline in CVD mortality was observed between 1988 and 1994, and 2010 and 2015, as well as a reduction in the excess risk between populations with and without diabetes [15]. In Australia, a 50% decline in CVD-mortality rates was observed between 2000 and 2011 [16] and, in Iceland, a 46% decline was observed between 1993 and 2004 [17]. In Canada, in-hospital mortality for acute myocardial infarction (AMI) and stroke fell by 44.1% and 17.1%, respectively, between 1992 and 1999, but individuals with diabetes were still 1.6 times more likely to die from these events than those without diabetes [3]. Similar declines for CVD mortality in individuals with type 1 diabetes have also been shown in Australia [16] and Switzerland [18].
Microvascular complications
LEAs
LEAs are a major complication for adults with diabetes because of their physical, economical and psychosocial burden. Since several aetiological pathways are associated with conditions leading to LEAs, LEAs are also an important indicator of the success of preventive care, such as that targeting glycaemic control, CVD risk factor management, and screening and treatment of people at high risk of foot complications. Population-based studies indicate that, in general, there have been reductions in the rates of LEAs between 1982 and 2011 (by ~3% to 85%) across diverse populations [9, 19,20,21,22,23] (Fig. 1 and Table 2). Only two studies have specifically examined trends among people with type 1 diabetes; significant declines were observed in Spain [24] and non-significant declines were seen in Australia [21].
Trends in LEAs among people with diabetes, by country, between 1988 and 2011. Data in the figure were derived from population-based studies of countries or major regions of countries in which rates of LEAs were examined using the same methods within populations over time. Differences in absolute rates between countries may be affected by variation in age and differences in criteria for diagnosis of both LEA and diabetes. Data are intended to be interpreted as trends over time and should not be used for comparison of absolute rates between countries at any one time point. aUnadjusted rate; brate per 100,000 person-years. This figure is available as part of a downloadable slideset
Among the 13 countries and major regions of countries with available data, the decline in total LEA incidence appears to be driven by declines in major LEAs (Fig. 2a, Table 2). Smaller relative declines have been reported for minor LEAs, with some countries even reporting increases (Fig. 2b, Table 2). This suggests that there may be a relative increase in the number of minor LEAs being performed in the clinical setting to prevent major LEAs. There also remain important disparities in rates of LEA between subgroups within populations. For example, in the USA, decreases in LEA rates are mainly attributable to greater reductions in LEAs in the elderly, with reductions in rates in young and middle-age people being modest [22]. In addition, the number of LEAs remain higher in non-whites and the male population in the USA [25], and large geographical differences exist [26].
Trends in (a) major and (b) minor LEAs among people with diabetes, by country, between 1982 and 2010. Data in the figure were derived from population-based studies of countries or major regions of countries in which rates of LEAs were examined using the same methods within populations over time. Differences in absolute rates between countries may be affected by variation in age and differences in criteria for diagnosis of both LEA and diabetes. Data are intended to be interpreted as trends over time and should not be used for comparison of absolute rates between countries at any one time point. aUnadjusted rate. This figure is available as part of a downloadable slideset
ESRD
Worldwide, it is estimated that 80% of ESRD cases are caused by diabetes or hypertension [28]. Between 2002 and 2015, steep increases (approximately 40–700%) in the incidence of diabetes-associated ESRD were reported for Russia, the Philippines, Malaysia, the Republic of Korea, the Jalisco region of Mexico and Singapore, as well as Australia, Taiwan, Bosnia and Herzegovina and Scotland. In the USA, the increase was 11% for the same period [28] (Fig. 3). By contrast, diabetes-associated ESRD incidence declined over the same period in Austria (by 26%), Belgium (16%), Finland (11%), Denmark (2%), and Sweden (1%). All of these rates are reported for overall country-specific populations, not for diabetes populations, and increases likely reflect the increasing prevalence of both type 1 and type 2 diabetes in these populations [28].
Trends in the incidence rate (per million people in the general population/year) of diabetes-related ESRD, by country, between 2002 and 2015. The graph was generated based on data from the United States Renal Data System (USRDS) annual data report 2017 [28]. This figure is available as part of a downloadable slideset
Among adults with type 2 diabetes, the incidence of ESRD declined by approximately 6% per year between 2000 and 2012 in a nationwide study of Chinese participants [29]. In the USA, incidence of ESRD in those with diabetes declined by 28% between 1990 and 2010, with a statistically significant decrease across all age groups after the year 2000 [19]. This decline was smaller than for other reported complications of diabetes, such as AMI, stroke, LEAs and death from hypoglycaemia, possibly owing to more inclusive criteria for initiating renal replacement therapy in the earlier years and large reductions in cardiovascular complications, both improving morbidity and mortality rates among people with diabetes.
Trends in the incidence of treated ESRD (i.e. dialysis initiation) among people with diabetes are also known to differ by race/ethnicity. In the USA, the incidence rate of treated ESRD declined between 2000 and 2013, by 28%, 22%, 14%, and 13% in American Indian/Alaska Native, Hispanic, non-Hispanic white and non-Hispanic black people with diabetes, respectively. Within the same timeframe, ESRD incidence remained relatively stable in Asian individuals with diabetes [30].
According to the United States Renal Data System (USRDS) reports, of all new cases of diabetes-associated ESRD, an estimated 91% were attributable to type 2 diabetes. Epidemiological data on trends in the incidence of treated ESRD in type 1 diabetes are less clear, partly because type 1 diabetes is less frequent than type 2 diabetes and also because of uncertainties related to the diagnosis of type 1 diabetes; young people with diabetes or those treated with insulin are often misclassified as having type 1 diabetes. Nonetheless, a review of ESRD in eight countries or regions of Europe, and in non-indigenous Canadians and Australians, found that incidence of type 1 diabetes-related ESRD declined between 1998 and 2002 [31]. Unlike type 2 diabetes, there are no studies among national cohorts with type 1 diabetes populations as the denominator; however, several cohort studies indicate that for a given duration of type 1 diabetes, people diagnosed in more recent decades have a lower incidence of ESRD than those diagnosed in the 1960s and 1970s [32]. Declines in type 1 diabetes-related ESRD may be attributed to the widespread use of renin–angiotensin system inhibitors and statin therapy at younger ages in this population, and recent improvements in insulin delivery technologies. On the other hand, in Taiwan, the incidence of type 1 diabetes-related ESRD increased substantially between 1999 and 2010 (from 0.13 to 3.52 per 1000 people; p < 0.001) [33].
Retinopathy
Retinopathy affects approximately one third of adults with diabetes and represents the leading cause of blindness in these individuals [34]. Despite how common diabetic retinopathy is, there are few population-based data on incidence trends. Of the few studies that do report objectively measured annual incidence of retinopathy over time, findings are mixed (Table 3).
Generally, population-based studies conducted from the 1990s onwards report a 50–67% lower incidence of diabetic retinopathy compared with earlier studies [34]. A meta-analysis of 28 studies and 27,120 participants with type 1 and type 2 diabetes showed that the pooled incidence of proliferative diabetic retinopathy was lower in 1986–2008 (2.6%) compared with 1975–1985 (19.5%) [35]. Likewise, in the Pittsburgh Epidemiology of Diabetes Complications Study, incidence of proliferative diabetic retinopathy reduced from 38% in 1965–1969 to 26.5% in 1975–1980 [36]. These trends are likely to be owing to earlier identification and treatment of both diabetes and diabetic retinopathy and reductions in smoking rates. Moreover, lessons learned from the UK Prospective Diabetes Study (UKPDS) and DCCT trial, leading to better glycaemic and blood pressure control in diabetes, may have also contributed to the reduced incidence of diabetic retinopathy over recent years.
Neuropathy
Information on trends in the prevalence or incidence of neuropathy are virtually non-existent due to the lack of data from repeated population surveys. Surveillance data from the US Diabetes Surveillance System (USDSS) show that the rate of hospitalisations for neuropathy (both first admission and any readmissions) increased by 42.1% (from 29.7 to 42.2 per 1000 people with diabetes) between 2000 and 2014; although these data are likely influenced by changes in coding of neuropathy and increased awareness of neuropathy among individuals with diabetes [37]. Historical data from the Pittsburgh Epidemiology of Diabetes Complications Study indicate a decline in the incidence of distal symmetrical polyneuropathy in participants with a 25-year duration of type 1 diabetes who were diagnosed between 1970 and 1974 compared with those diagnosed between 1965 and 1969 [36].
Acute complications
Acute complications of diabetes, such as diabetic ketoacidosis (DKA), the hyperglycaemic hyperosmolar state (HHS), lactic acidosis and hypoglycaemia are largely preventable, yet they still account for high morbidity and mortality among people with diabetes and contribute significantly to the high costs of diabetes care [43]. In the USA, the SEARCH for Diabetes in Youth study reported that 29% of individuals aged <20 years with type 1 diabetes, and 10% with type 2 diabetes presented with DKA at diagnosis [44]. The incidence of DKA in children and adolescents with type 1 diabetes also remains high, with approximately 1–12 episodes per 100 patient-years [43]. Comparable population-based data for adults are not currently available.
Overall, data suggest that DKA-related mortality and hospitalisation rates for acute complications are decreasing among people with diabetes (Table 4). However, in the USA, since 2010, significant increases in hospitalisations for hyperglycaemia and death from hyperglycaemic crisis have been reported by the USDSS, although continued declines in hospitalisations for hypoglycaemia were observed [37].
Decreasing temporal trends in hospitalisations and deaths from acute diabetes complications suggest improvements in in-hospital management of DKA and HHS and outpatient care, and better patient education in disease management. Reasons for increases in acute complications, as observed in the USA, are, at this stage, unclear.
Mortality
Non-cardiovascular mortality
Diabetes is associated with a diverse set of specific, non-cardiovascular causes of death. An international meta-analysis of 97 prospective studies representing 820,900 individuals with diabetes and 123,205 deaths throughout North America and Europe found that diabetes was associated with an increased risk for mortality from several cancers (17–116% increased risk, depending on the cancer site), renal disease, infections, liver disease, digestive system disorders, falls, pneumonia, mental health issues, intentional self-harm, external causes, nervous system disorders, chronic obstructive pulmonary disease (COPD) and related conditions, and other non-cancer, non-vascular causes [48].
Observations of trends in non-cardiovascular mortality are restricted to a few studies. In the USA, the rate of cancer-related deaths declined by 16% every 10 years between 1988–1994 and 2010–2015, while the rate of non-vascular, non-cancer-related deaths declined by a smaller magnitude (8% every 10 years) [15]. In Australia, age-standardised mortality rates (ASMRs) for all-cause, CVD and diabetes decreased significantly between 2000 and 2011, while cancer-related ASMRs remained unchanged in people with type 1 and type 2 diabetes [16]. Data from the same national registry in Australia demonstrated that cancer is now the second leading cause of death among people with diabetes, increasing from 25% of all deaths to 35% between 1997 and 2010 [49]. Similar findings have been reported in the USA [50] and Taiwan [51]. This is important in light of the increasing prevalence of diabetes that is coinciding with an ageing population, the latter being an inherent risk factor for both diabetes and cancer.
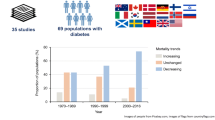
All-cause mortality
Mortality rates due to diabetes are often estimated from vital statistics systems (based on death certificate data), the efficacy of which may be affected by diabetes prevalence, coding practices and country-level awareness of diabetes. Therefore, to adequately monitor mortality rates among populations with diabetes, rates should ideally be estimated among defined cohorts with diagnosed diabetes. However, data on all-cause and cause-specific mortality among people with diabetes are difficult to compare and come from a relatively small number of high-income countries within North America, Europe, Australia and Asia. Population-based data on all-cause mortality from several of these countries are shown in Fig. 4 and Table 5. These data are intended to be interpreted as trends over time, rather than as a comparison of absolute rates between countries, as methodologies differ between the studies. Nonetheless, a consistent reduction in mortality among people with diabetes (either type 2 diabetes or all [type 1 and type 2] diabetes) has been observed since the late 1980s, ranging from a 4% relative decline in mortality among Taiwanese women with diabetes (27% in Taiwanese men) between 2000 and 2009 [51], to a 37% decline in Canadians between 1996 and 2009 [52].
Trends in all-cause mortality among people with diabetes, by country, between 1988 and 2015. Data in the figure were derived from population-based studies of countries or major regions of countries in which all-cause mortality rates were examined using the same methods within populations over time. Differences in absolute rates between countries may be affected by variation in age, differences in diabetes diagnosis, country-level awareness of diabetes and collection of vital statistics. Data are intended to be interpreted as trends over time and should not be used for comparison of absolute rates between countries at any one time point. aRate per 100,000 person-years. This figure is available as part of a downloadable slideset
Studies that compare populations with and without diabetes show that the relative difference between the two populations is decreasing over time, but excess risk remains among people with diabetes, even at more recent time points [53]. For example, in Ontario, Canada, the mortality rate ratio decreased from 1.90 (95% CI 1.86, 1.94) in 1996 to 1.51 (95% CI 1.48, 1.54) in 2009 [52], and similar declines have been noted in the UK [52], USA [15] and Australia [49].
For type 1 diabetes, there is a 3–18-fold excess risk for death compared with individuals without diabetes [54]. However, continued improvements in mortality rates have been noted by a few studies. For example, in the USA, between 1950 and 2009, marked declines in the number of deaths attributed to type 1 diabetes were observed across all age groups (by 45–90%) [54]. An analysis by the Centers for Disease Control and Prevention also showed a 61% decrease in diabetes-related mortality prior to age 20 years between 1968–1969 and 2008–2009 [55]. Outside of the USA, Japan and Finland reported declines in mortality rates of 69% and 8%, respectively, when comparing mortality among those diagnosed with childhood-onset type 1 diabetes in 1965–1969 with those diagnosed in 1975–1979 [56]. The smaller declines in Finland are most likely explained by the lower absolute mortality in this country as compared with Japan [56]. In Norway, mortality rates among individuals diagnosed with type 1 diabetes between 1973 and 1982, before 15 years of age, was reduced by 81% (from 286 to 53 per 100,000 person-years) compared with those diagnosed in 1999–2012 [57]. In Australia, mortality rates among individuals with type 1 diabetes who were diagnosed before 45 years of age declined by 33% between 2000 and 2011 [16].
Emerging complications of diabetes
The increase in diabetes incidence since the 1980s, combined with declining mortality among people with diabetes, has increased the total years of life spent with diabetes. Longer life expectancy among those with diabetes has also driven the emergence of newly recognised complications, including cancer, infections and physical and cognitive disability. Observations of trends in ‘emerging’ diabetes complications are restricted to a few select studies.
Individuals with diabetes have an increased risk for tuberculosis, severe gram-positive infections, hospital-acquired postoperative infections, urinary tract infections (UTIs) and tropical diseases compared with people without diabetes [63]. Whether the rate of infections among populations with diabetes has changed over time is not clear. In the USA, data from the National Vital Statistics System show that the per cent of deaths with infections listed anywhere on the death certificate decreased from 3.1% in 1999 to 2.7% in 2010 in people with diabetes and from 4.5% to 4.1% in people without, with respiratory tract infections accounting for the highest percentage of deaths in both groups [63]. An analysis of data from the National Nursing Home Surveys between 1999 and 2004 showed that the age-standardised proportion of nursing home residents with infections among people with diabetes increased from 6.1% to 10.3% between 1999 and 2004, while in people without diabetes this increased from 6.0% to 8.5% [63]. In Spain, a 61.3% increase in hospitalisation rates for sepsis was observed between 2008 and 2012 [64], though changes in ICD-9-clinical modification (ICD-9-CM; www.cdc.gov/nchs/icd/icd9cm.htm) codes make it difficult to assess the change in sepsis over time.
A growing body of research suggests that people with diabetes are at increased risk for major depressive disorder [65], anxiety [66], eating disorders (particularly in female adolescents with type 1 diabetes) [67], serious mental illness (e.g. schizophrenia) [68], dementia [69], and several domains of disability, including mobility loss, reduced instrumental activities of daily living (IADL) or basic activities of daily living, and work disability [70]. Again, whether risk has changed over time remains unknown as for many of these complications, prospective data with adequate follow-up is not available. For depression, two studies have explored trends over time. In Spain, the prevalence of depression among hospitalised individuals with type 2 diabetes increased significantly from 3.5% to 5.8% between 2001 and 2011, with increases being much higher in women [71]. In Finland, the use of antidepressants was more common in people with diabetes compared with those without and use of these drugs increased more rapidly between 1997 and 2007 in people with diabetes, particularly younger individuals with type 2 diabetes [72]. For physical disability, data from the USA show that the prevalence of both impaired mobility and IADLs have not changed in recent decades, while work disability declined from 23.8% in 1997 to 17.9% in 2006; however, this then increased to 19.7% in 2011 [70]. In relative terms, similar trends in rates of disability were reported among the non-diabetic population, but, in absolute terms, rates over time were smaller (from 9.8% in 1997 to 5.8% in 2010).

Discussion
This review of international trends in diabetes-related complications reveals several key conclusions (see Text box); first, rates of LEAs, acute complications, CVD and all-cause and CVD-related mortality among populations of people with diabetes are declining. Data on trends in ESRD, diabetic retinopathy and neuropathy, non-CVD-related causes of death and ‘emerging’ complications in these populations are scarce, however, and, as such, conclusions are limited. Second, in spite of notable declines in several diabetes complications, people with diabetes remain at significantly higher risk for these complications compared with people without diabetes. Third, declines in all-cause and CVD-related mortality are leading to proportional increases in other forms of morbidity, including renal disease, infections, cancers, and physical and cognitive disability, with important implications for the clinical and public health burden of diabetes. Last, there is a genuine lack of comparable data on trends in rates of diabetes complications, specifically from low- and middle-income countries. Therefore, conclusions drawn from this work are limited to about a dozen high-income countries in North America, Europe and East Asia and, as such, this leaves the status of global trends in diabetes complications unclear.
The explanation for the decline in rates of diabetes complications among selected countries around the world is likely multifactorial, involving trends in the underlying risk factors of the population and changes in preventive care and medical treatment. Reductions in macrovascular complications in high-income countries are likely influenced by improved pharmacotherapy, CVD treatment procedures and better prevention strategies [73]. For example, large reductions in smoking rates occurred in the 1970s and 1980s, followed by gradual reductions thereafter [74, 75]. Blood pressure control also improved in the 1980s and 1990s, driven by new evidence for treatment efficacy from clinical trials and better awareness of blood pressure as a key risk factor for CVD [74, 75]. In addition, lipid levels have declined over time, likely due to increased use of lipid-lowering medications as well as reductions in trans-fat intake [73, 76]. These improvements in risk factor management in high-income countries have likely had additional benefits in terms of microvascular complications, which have been further buoyed by improvements in glycaemic control since 2000 [73, 76, 77]. In the USA, the improvements in risk factors are also likely driven by improvements in the organisation of care and initiatives to improve quality of diabetes care. Whether improvements in risk factors, treatment options and medical care also occurs in the majority of other countries in the world is unclear due to the lack of continuous monitoring systems.
Trends in rates of diabetes complications are also influenced by background trends in mortality. For example, the large reductions in CVD-related mortality in populations with diabetes that have been observed in the USA, Australia and several other countries in Northern Europe have increased survival rates, resulting in proportional increases in other causes of death, including those due to cancer, renal disease and infections.
The interpretation of trends in rates of diabetes complications also depends on which denominator population (diabetes or whole population) is used. This review has focused primarily on the average risk for the average person with diagnosed diabetes, independent of changes in prevalence of diabetes in the underlying population. When rates are calculated as the frequency of diabetes-related complications in the general population, many countries reveal flat or even increasing trends because the increases in diabetes prevalence offset reductions in risk of complications within the diabetic population [19]. For example, while the average adult with diabetes in the USA has a lower risk of CVD than in previous decades, the average adult in the general population has an increased risk of diabetes-related CVD than in previous decades because of the large increase in diabetes prevalence. The fact that trends differ depending on the choice of general population denominator is a reminder that the burden of the wide spectrum of complications in those with diabetes will ultimately be influenced by efforts to prevent diabetes.
Conclusion
In this review, we have highlighted the scarcity of data outside North America, Europe and high-income Asia-Pacific countries, leaving the global status of diabetes complications rates unclear, especially in low and middle-income countries. This gap in data stems largely from the lack of population-based systems quantifying healthcare utilisation because surveys and cohort studies are generally inadequate for the assessment of diabetic complications. The comparison of trends in complications has also been hampered by varied reporting methods, definitions of complications and methods to identify people with diabetes. Future monitoring of global trends in diabetes complications could be enhanced by implementing standardised reporting methods and establishing practical registries that suit the dual needs of population monitoring and providing feedback and decision support for clinical systems.
Abbreviations
- AMI:
-
Acute myocardial infarction
- ASMR:
-
Age-standardised mortality rates
- CVD:
-
Cardiovascular disease
- DKA:
-
Diabetic ketoacidosis
- ESRD:
-
End-stage renal disease
- HHS:
-
Hyperglycaemic hyperosmolar state
- IADL:
-
Instrumental activities of daily living
- LEA:
-
Lower-extremity amputation
- USDSS:
-
United States Diabetes Surveillance System
References
Ogurtsova K, da Rocha Fernandes JD, Huang Y et al (2017) IDF Diabetes Atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract 128:40–50
International Diabetes Federation (2016) Diabetes and cardiovascular disease. Brussels, Belgium: International Diabetes Federation 2016. Available from www.idf.org/our-activities/care-prevention/cardiovascular-disease/cvd-report. Accessed 24 July 2018
Booth GL, Kapral MK, Fung K, Tu JV (2006) Recent trends in cardiovascular complications among men and women with and without diabetes. Diabetes Care 29:32–37
Burrows NR, Li Y, Gregg EW, Geiss LS (2018) Declining rates of hospitalization for selected cardiovascular disease conditions among adults aged ≥35 years with diagnosed diabetes, U.S., 1998–2014. Diabetes Care 41:293–302
Jung CH, Chung JO, Han K et al (2017) Improved trends in cardiovascular complications among subjects with type 2 diabetes in Korea: a nationwide study (2006–2013). Cardiovasc Diabetol 16:1
Lopez-de-Andres A, Jimenez-Garcia R, Hernandez-Barrera V et al (2014) National trends over one decade in hospitalization for acute myocardial infarction among Spanish adults with type 2 diabetes: cumulative incidence, outcomes and use of percutaneous coronary intervention. PLoS One 9:e85697
Lopez-de-Andres A, Jimenez-Trujillo I, Jimenez-Garcia R et al (2015) National trends in incidence and outcomes of abdominal aortic aneurysm among elderly type 2 diabetic and non-diabetic patients in Spain (2003-2012). Cardiovasc Diabetol 14:48
Munoz-Rivas N, Mendez-Bailon M, Hernandez-Barrera V et al (2015) Time trends in ischemic stroke among type 2 diabetic and non-diabetic patients: analysis of the Spanish National Hospital Discharge Data (2003-2012). PLoS One 10:e0145535
Ringborg A, Lindgren P, Martinell M, Yin DD, Schon S, Stalhammar J (2008) Prevalence and incidence of type 2 diabetes and its complications 1996–2003—estimates from a Swedish population-based study. Diabet Med 25:1178–1186
Vamos EP, Millett C, Parsons C, Aylin P, Majeed A, Bottle A (2012) Nationwide study on trends in hospital admissions for major cardiovascular events and procedures among people with and without diabetes in England, 2004–2009. Diabetes Care 35:265–272
Yashkin AP, Picone G, Sloan F (2015) Causes of the change in the rates of mortality and severe complications of diabetes mellitus: 1992-2012. Med Care 53:268–275
Levi F, Lucchini F, Negri E, La Vecchia C (2002) Trends in mortality from cardiovascular and cerebrovascular diseases in Europe and other areas of the world. Heart 88:119–124
Abi Khalil C, Roussel R, Mohammedi K, Danchin N, Marre M (2012) Cause-specific mortality in diabetes: recent changes in trend mortality. Eur J Prev Cardiol 19:374–381
Taylor KS, Heneghan CJ, Farmer AJ et al (2013) All-cause and cardiovascular mortality in middle-aged people with type 2 diabetes compared with people without diabetes in a large U.K. primary care database. Diabetes Care 36:2366–2371
Gregg EW, Cheng YJ, Srinivasan M et al (2018) Trends in cause-specific mortality among adults with and without diagnosed diabetes in the USA: an epidemiological analysis of linked national survey and vital statistics data. Lancet 391:2430–2440
Harding JL, Shaw JE, Peeters A, Davidson S, Magliano DJ (2016) Age-specific trends from 2000–2011 in all-cause and cause-specific mortality in type 1 and type 2 diabetes: a cohort study of more than one million people. Diabetes Care 39:1018–1026
Olafsdottir E, Aspelund T, Sigurdsson G et al (2013) Similar decline in mortality rate of older persons with and without type 2 diabetes between 1993 and 2004 the Icelandic population-based Reykjavik and AGES-Reykjavik cohort studies. BMC Public Health 13:36
Allemann S, Saner C, Zwahlen M, Christ ER, Diem P, Stettler C (2009) Long-term cardiovascular and non-cardiovascular mortality in women and men with type 1 and type 2 diabetes mellitus: a 30-year follow-up in Switzerland. Swiss Med Wkly 139:576–583
Gregg EW, Li Y, Wang J et al (2014) Changes in diabetes-related complications in the United States, 1990–2010. N Engl J Med 370:1514–1523
Kennon B, Leese GP, Cochrane L et al (2012) Reduced incidence of lower-extremity amputations in people with diabetes in Scotland: a nationwide study. Diabetes Care 35:2588–2590
Kurowski JR, Nedkoff L, Schoen DE, Knuiman M, Norman PE, Briffa TG (2015) Temporal trends in initial and recurrent lower-extremity amputations in people with and without diabetes in Western Australia from 2000 to 2010. Diabetes Res Clin Pract 108:280–287
Moxey PW, Gogalniceanu P, Hinchliffe RJ et al (2011) Lower-extremity amputations — a review of global variability in incidence. Diabet Med 28:1144–1153
Narres M, Kvitkina T, Claessen H et al (2017) Incidence of lower-extremity amputations in the diabetic compared with the non-diabetic population: a systematic review. PLoS One 12:e0182081
Carinci F, Massi Benedetti M, Klazinga NS, Uccioli L (2016) Lower extremity amputation rates in people with diabetes as an indicator of health systems performance. A critical appraisal of the data collection 2000–2011 by the Organization for Economic Cooperation and Development (OECD). Acta Diabetol 53:825–832
Li Y, Burrows NR, Gregg EW, Albright A, Geiss LS (2012) Declining rates of hospitalization for nontraumatic lower-extremity amputation in the diabetic population aged 40 years or older: U.S., 1988-2008. Diabetes Care 35:273–277
Margolis DJ, Hoffstad O, Nafash J et al (2011) Location, location, location: geographic clustering of lower-extremity amputation among Medicare beneficiaries with diabetes. Diabetes Care 34:2363–2367
Lopez-de-Andres A, Martinez-Huedo MA, Carrasco-Garrido P, Hernandez-Barrera V, Gil-de-Miguel A, Jimenez-Garcia R (2011) Trends in lower-extremity amputations in people with and without diabetes in Spain, 2001–2008. Diabetes Care 34:1570–1576
United States Renal Data System. 2017 USRDS annual data report: epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2017. Available from www.usrds.org/adr.aspx. Accessed 26 July 2018
Luk AOY, Hui EMT, Sin MC et al (2017) Declining trends of cardiovascular-renal complications and mortality in type 2 diabetes: The Hong Kong Diabetes Database. Diabetes Care 40:928–935
Bullock A, Burrows NR, Narva AS et al (2017) Vital signs: decrease in incidence of diabetes-related end-stage renal disease among American Indians/Alaska Natives — United States, 1996–2013. MMWR Morb Mortal Wkly Rep 66:26–32
Group EIS, Stewart JH, McCredie MR, Williams SM (2006) Divergent trends in the incidence of end-stage renal disease due to type 1 and type 2 diabetes in Europe, Canada and Australia during 1998–2002. Diabet Med 23:1364–1369
Helve J, Sund R, Arffman M et al (2018) Incidence of end-stage renal disease in patients with type 1 diabetes. Diabetes Care 41:434–439
Lin WH, Li CY, Wang WM, Yang DC, Kuo TH, Wang MC (2014) Incidence of end stage renal disease among type 1 diabetes: a nationwide cohort study in Taiwan. Medicine 93:e274
Liew G, Wong VW, Ho IV (2017) Mini Review: changes in the incidence of and progression to proliferative and sight-threatening diabetic retinopathy over the last 30 years. Ophthalmic Epidemiol 24:73–80
Wong TY, Mwamburi M, Klein R et al (2009) Rates of progression in diabetic retinopathy during different time periods: a systematic review and meta-analysis. Diabetes Care 32:2307–2313
Pambianco G, Costacou T, Ellis D, Becker DJ, Klein R, Orchard TJ (2006) The 30-year natural history of type 1 diabetes complications: the Pittsburgh Epidemiology of Diabetes Complications Study experience. Diabetes 55:1463–1469
Centers for Disease Control and Prevention. Diabetes Atlas, United States Diabetes Surveillance System 2018. Available from: https://gis.cdc.gov/grasp/diabetes/DiabetesAtlas.html. Accessed 24 July 2018
Mathur R, Bhaskaran K, Edwards E et al (2017) Population trends in the 10-year incidence and prevalence of diabetic retinopathy in the UK: a cohort study in the Clinical Practice Research Datalink 2004–2014. BMJ Open 7:e014444
Klein R, Lee KE, Gangnon RE, Klein BE (2010) The 25-year incidence of visual impairment in type 1 diabetes mellitus: the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Ophthalmology 117:63–70
Song SJ, Han K, Choi KS et al (2018) Trends in diabetic retinopathy and related medical practices among type 2 diabetes patients: results from the National Insurance Service Survey 2006–2013. J Diabetes Investig 9:173–178
Tracey ML, McHugh SM, Fitzgerald AP, Buckley CM, Canavan RJ, Kearney PM (2016) Trends in blindness due to diabetic retinopathy among adults aged 18–69 years over a decade in Ireland. Diabetes Res Clin Pract 121:1–8
Hall HN, Chinn DJ, Sinclair A, Styles CJ (2013) Epidemiology of blindness attributable to diabetes in Scotland: change over 20 years in a defined population. Diabet Med 30:1349–1354
Rewers A (2017) Acute metabolic complications in diabetes. In: Diabetes in America, 3rd edn. National Institutes of Health, NIH Pub No. 17-1468; pp 17-1–17-19
Klingensmith GJ, Tamborlane WV, Wood J et al (2013) Diabetic ketoacidosis at diabetes onset: still an all too common threat in youth. J Pediatr 162:330–4.e1
Booth GL, Hux JE, Fang J, Chan BT (2005) Time trends and geographic disparities in acute complications of diabetes in Ontario, Canada. Diabetes Care 28:1045–1050
Lombardo F, Maggini M, Gruden G, Bruno G (2013) Temporal trend in hospitalizations for acute diabetic complications: a nationwide study, Italy, 2001–2010. PLoS One 8:e63675
Liu CC, Chen KR, Chen HF, Huang HL, Ko MC, Li CY (2010) Trends in hospitalization for diabetic ketoacidosis in diabetic patients in Taiwan: analysis of national claims data, 1997–2005. J Formos Med Assoc 109:725–734
Rao Kondapally Seshasai S, Kaptoge S et al (2011) Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 364:829–841
Harding JL, Shaw JE, Peeters A, Guiver T, Davidson S, Magliano DJ (2014) Mortality trends among people with type 1 and type 2 diabetes in Australia: 1997–2010. Diabetes Care 37:2579–2586
Thomas RJ, Palumbo PJ, Melton LJ III et al (2003) Trends in the mortality burden associated with diabetes mellitus: a population-based study in Rochester, Minn, 1970-1994. Arch Intern Med 163:445–451
Li HY, Jiang YD, Chang CH, Chung CH, Lin BJ, Chuang LM (2012) Mortality trends in patients with diabetes in Taiwan: a nationwide survey in 2000–2009. J Formos Med Assoc 111:645–650
Lind M, Garcia-Rodriguez LA, Booth GL et al (2013) Mortality trends in patients with and without diabetes in Ontario, Canada and the UK from 1996 to 2009: a population-based study. Diabetologia 56:2601–2608
Rosenquist KJ, Fox CS (2017) Mortality trends in type 2 diabetes. In: Diabetes in America, 3rd edn. National Institutes of Health, NIH Pub No. 17-1468; pp 36-1–36-14
Secrest AM, Washington RE, Orchard TJ 2017 Mortality in type 1 diabetes. In: Diabetes in America, 3rd edn. National Institutes of Health, NIH Pub No. 17-1468; pp 35-1–35-16
Centers for Disease Control and Prevention (2012) Diabetes death rates among youths aged ≤19 years — United States, 1968–2009. MMWR Morb Mortal Wkly Rep 61:869–872
Asao K, Sarti C, Forsen T et al (2003) Long-term mortality in nationwide cohorts of childhood-onset type 1 diabetes in Japan and Finland. Diabetes Care 26:2037–2042
Gagnum V, Stene LC, Sandvik L et al (2015) All-cause mortality in a nationwide cohort of childhood-onset diabetes in Norway 1973–2013. Diabetologia 58:1779–1786
Forssas E, Arffman M, Koskinen S, Reunanen A, Keskimaki I (2010) Socioeconomic differences in mortality among diabetic people in Finland. Scand J Public Health 38:691–698
Zghebi SS, Steinke DT, Carr MJ, Rutter MK, Emsley RA, Ashcroft DM (2017) Examining trends in type 2 diabetes incidence, prevalence and mortality in the UK between 2004 and 2014. Diabetes Obes Metab 19:1537–1545
Green A, Sortso C, Jensen PB, Emneus M (2015) Incidence, morbidity, mortality, and prevalence of diabetes in Denmark, 2000–2011: results from the Diabetes Impact Study 2013. Clin Epidemiol 7:421–430
Karpati T, Cohen-Stavi CJ, Leibowitz M, Hoshen M, Feldman BS, Balicer RD (2014) Towards a subsiding diabetes epidemic: trends from a large population-based study in Israel. Popul Health Metrics 12:32
Read SH, Kerssens JJ, McAllister DA et al (2016) Trends in type 2 diabetes incidence and mortality in Scotland between 2004 and 2013. Diabetologia 59:2106–2113
Egede LE, Hull BJ, Williams JS (2017) Infections associated with diabetes. In: Diabetes in America, 3rd edn. National Institutes of Health, NIH Pub No. 17-1468; pp 30-1-30-25
de Miguel-Yanes JM, Mendez-Bailon M, Jimenez-Garcia R, Hernandez-Barrera V, Perez-Farinos N, Lopez-de-Andres A (2015) Trends in sepsis incidence and outcomes among people with or without type 2 diabetes mellitus in Spain (2008–2012). Diabetes Res Clin Pract 110:266–275
Ali S, Stone MA, Peters JL, Davies MJ, Khunti K (2006) The prevalence of co-morbid depression in adults with type 2 diabetes: a systematic review and meta-analysis. Diabet Med 23:1165–1173
Fisher L, Skaff MM, Mullan JT, Arean P, Glasgow R, Masharani U (2008) A longitudinal study of affective and anxiety disorders, depressive affect and diabetes distress in adults with type 2 diabetes. Diabet Med 25:1096–1101
Ward A, Troop N, Cachia M, Watkins P, Treasure J (1995) Doubly disabled: diabetes in combination with an eating disorder. Postgrad Med J 71:546–550
Vancampfort D, Correll CU, Galling B et al (2016) Diabetes mellitus in people with schizophrenia, bipolar disorder and major depressive disorder: a systematic review and large scale meta-analysis. World Psychiatry 15:166–174
Li J, Shao YH, Gong YP, Lu YH, Liu Y, Li CL (2014) Diabetes mellitus and dementia - a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci 18:1778–1789
Gregg EW, Menke A (2017) Diabetes and disability. In: Diabetes in America, 3rd edn. National Institutes of Health, NIH Pub No. 17-1468; pp 34-1–34-15
Lopez-de-Andres A, Jimenez-Trujillo MI, Hernandez-Barrera V et al (2015) Trends in the prevalence of depression in hospitalized patients with type 2 diabetes in Spain: analysis of hospital discharge data from 2001 to 2011. PLoS One 10:e0117346
Manderbacka K, Sund R, Koski S, Keskimaki I, Elovainio M (2011) Diabetes and depression? Secular trends in the use of antidepressants among persons with diabetes in Finland in 1997–2007. Pharmacoepidemiol Drug Saf 20:338–343
Ford ES (2011) Trends in the control of risk factors for cardiovascular disease among adults with diagnosed diabetes: findings from the National Health and Nutrition Examination Survey 1999–2008*. J Diabetes 3:337–347
Imperatore G, Cadwell BL, Geiss L et al (2004) Thirty-year trends in cardiovascular risk factor levels among US adults with diabetes: National Health and Nutrition Examination Surveys, 1971–2000. Am J Epidemiol 160:531–539
GBD 2016 Risk Factors Collaborators (2017) Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390:1345–1422
Heart Protection Study Collaborative Group (2002) MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20536 high-risk individuals: a randomised placebo-controlled trial. Lancet 360:7–22
Ali MK, Bullard KM, Saaddine JB, Cowie CC, Imperatore G, Gregg EW (2013) Achievement of goals in U.S. diabetes care, 1999–2010. N Engl J Med 368:1613–1624
Acknowledgements
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
The interpretation and reporting of the ESRD data supplied by the United States Renal Data System (USRDS) are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the US government.
Author information
Authors and Affiliations
Contributions
JLH contributed to the literature search and data analyses and interpretation and wrote the manuscript. MEP contributed to the literature search and data analyses and interpretation and reviewed the manuscript. DJM and JES contributed to interpretation of data and reviewed the manuscript. EWG contributed to interpretation of data and writing of the manuscript. All authors approved the version to be published.
Corresponding author
Ethics declarations
The authors declare that there is no duality of interest associated with this manuscript.
Electronic supplementary material
ESM
(PPTX 621 kb)
Rights and permissions
About this article
Cite this article
Harding, J.L., Pavkov, M.E., Magliano, D.J. et al. Global trends in diabetes complications: a review of current evidence. Diabetologia 62, 3–16 (2019). https://doi.org/10.1007/s00125-018-4711-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-018-4711-2