Abstract
Aims/hypothesis
The treatment of type 2 diabetes with full peroxisome proliferator-activated receptor gamma (PPARγ) agonists improves insulin sensitivity, but is associated with weight gain, heart failure, peripheral oedema and bone loss. Endotrophin, the C-terminal fragment of the α3 chain of procollagen type VI (also called Pro-C6), is involved in both adipose tissue matrix remodelling and metabolic control. We established a serum assay for endotrophin to assess if this novel adipokine could identify type 2 diabetic patients who respond optimally to PPARγ agonists, improving the risk-to-benefit ratio.
Methods
The BALLET trial (NCT00515632) compared the glucose-lowering effects and safety of the partial PPARγ agonist balaglitazone with those of pioglitazone in individuals with type 2 diabetes on stable insulin therapy. The per protocol population (n = 297) was stratified into tertiles based on baseline endotrophin levels. Participants were followed-up after 26 weeks, after which correlational analysis was carried out between endotrophin levels and measures of glucose control. This is a secondary post hoc analysis.
Results
Endotrophin was significantly associated with therapeutic response to balaglitazone and pioglitazone. At week 26, only individuals in the upper two tertiles showed significant reductions in HbA1c and fasting serum glucose compared with baseline. The OR for a 1% and a 0.5% reduction in HbA1c for individuals in the upper two tertiles were 3.83 (95% CI 1.62, 9.04) p < 0.01, and 3.85 (95% CI 1.94, 7.61) p < 0.001, respectively. Endotrophin levels correlated with adipose tissue mass, insulin resistance and fatty liver index. Notably, PPARγ-associated adverse effects, such as moderate-to-severe lower extremity oedema, only occurred in the lower tertile.
Conclusions/interpretation
Elevated endotrophin serum levels predict response to two insulin sensitisers and reduce the risk of associated adverse effects, thereby, identifying patients with type 2 diabetes who may profit from PPARγ agonist treatment.
Similar content being viewed by others
Introduction
Type 2 diabetes is a major cause of morbidity and mortality in the industrialised and developing world [1]. There are numerous treatment options including metformin, insulin, glucagon-like peptide 1 (GLP-1) agonists, dipeptidyl peptidase IV (DPP-IV) inhibitors, partial and full agonists of peroxisome proliferator-activated receptor gamma (PPARγ), and drugs with alternative molecular targets [2]. However, there is a need for personalised healthcare (PHC) to identify those individuals who are likely to respond best to certain treatment options in order to increase the safety and benefits of a given intervention.
Recent research has revealed that the extracellular matrix (ECM) harbours properties of an endocrine organ. Its structural proteins generate signalling molecules that can modulate cellular processes at distant sites, including cell migration, differentiation and angiogenesis. These molecules include the potent anti-angiogenic peptide, endostatin, which is derived from type XVIII collagen, and tumstatin, vastatin and restin, which are released from types IV, VII and XV collagens, respectively [3].
The microflamentous interstitial type VI collagen, a triple helical molecule composed of the constituent chains α1(VI), α2(VI) and α3(VI), is expressed in most connective tissues and prominently in adipose tissue [4], where it anchors cells through its interconnections with other ECM proteins [5]. During formation of the microfilaments, the triple helical core of this type VI collagen is proteolytically released from its pro-peptide [6, 7]. Here, further cleavage of the C-terminal pro-peptide of the α3(VI) chain generates endotrophin (also known as Pro-C6), a newly identified adipokine. Endotrophin is predominantly produced by adipose tissue and induces upregulation of TGF-β, adipose tissue fibrosis, angiogenesis and inflammation [8]. In animal models, it has also been shown to unfavourably modulate several metabolic functions, such as insulin sensitivity, food intake, energy balance [8–10] and adipose tissue inflammation [11, 12]. These findings suggest that levels of endotrophin in the blood may be useful for classifying and/or monitoring patients with metabolic dysfunction, especially those with type 2 diabetes.
Thiazolidinediones (TZDs) are PPARγ agonists and have been used widely to treat type 2 diabetes because of their ability to improve insulin sensitivity, lower glucose levels and reduce the need for insulin [13, 14]. However, the use of TZDs, such as pioglitazone, has been limited substantially by associated adverse effects (AEs), such as heart failure [15], weight gain [16], peripheral oedema [17] and bone loss in women [18]. In an attempt to minimise the AEs associated with PPARγ agonists, partial activators of PPARγ, such as balaglitazone, which trigger only a subset of PPARγ downstream signals, have been developed [19, 20]. Such partial agonists achieve good glycaemic control with a reduced risk of AEs [21]. A serum biomarker that would optimally define treatment responders could further improve the efficacy and safety associated with such glitazones.
Using our recently developed serum assay for the assessment of endotrophin [22], we hypothesised that endotrophin levels may predict insulin resistance and possibly identify those patients with an optimal response to insulin sensitisers, such as balaglitazone or pioglitazone. In the present work, data from participants of the BALLET study were used to make a head-to-head comparison of balaglitazone and pioglitazone in late-stage insulin-dependent type 2 diabetes.
Methods
Study design
The BALLET study was a phase III, randomised, double-blind, parallel-group, placebo- and active comparator-controlled clinical study designed to determine the efficacy and safety of 6 months of balaglitazone or pioglitazone treatment in individuals with type 2 diabetes on stable insulin therapy. The baseline demographics, CONSORT diagram and efficacy and safety data have previously been published [23]. The current serological assessment is a secondary post-hoc analysis in which we used the per protocol population of the BALLET study (ClinicalTrial.gov registration no. NCT00515632), which consisted of 308 individuals (from whom 297 serum samples had been procured), randomised 1:1:1:1 across four groups (placebo, balaglitazone 10 mg, balaglitazone 20 mg and pioglitazone 45 mg) as previously described [23]. Existing serum samples from the BALLET study were used and reanalysed specifically for endotrophin for the current investigation. All other measures were collected previously [23] and used in the reanalysis. Study participants gave informed consent, allowing for re-analysis of their samples, and the study was approved by the local ethics committee and carried out in accordance with the Declaration of Helsinki as revised in 2008.
Endotrophin/Pro-C6 assay protocol
An endotrophin/Pro-C6 ELISA, targeting the C-terminus of the α3 chain of endotrophin, was previously designed [22] and employed for use in the present study. This is a standard competitive ELISA, using a mono-clonal mouse detection antibody. It has previously been shown to have acceptable dilution recovery, response to spiking, and intra- and inter-individual variation [22].
Statistical analysis
The analysis included individuals from the per protocol population, from whom a baseline measurement of serum endotrophin had been obtained. Participants were grouped into tertiles based on their endotrophin level at baseline (tertile 1, ≤6.2 ng/ml; tertile 2, 6.3–7.7 ng/ml; tertile 3, ≥7.8 ng/ml). The baseline characteristics of the three subgroups were compared by ANOVA and sex was compared by Fisher’s exact test.
Spearman’s ranked correlation was conducted on baseline levels of serum endotrophin, fasting serum glucose (FSG), blood HbA1c, BMI and the derived variables of HOMA-IR and the fatty liver index (FLI). The HOMA-IR was calculated according to the homeostasis model assessment including serum glucose and insulin [24], and FLI was calculated as described by Bedogni et al [25] using the equation (triacylglycerides [mmol/l], BMI [kg/m2], gamma-glutamyl transferase [GGT; U/l] and waist circumference [cm]):
Changes from baseline in FSG, blood HbA1c and serum endotrophin were studied as a function of time and treatment in each tertile. The least squares (LS) means ± SE were estimated from a mixed-effect repeated measure model (using baseline level, ‘visit’ (after 12 weeks of treatment) and end of treatment (after 26 weeks of treatment) with change from baseline as the dependent variable, and the baseline level vs visit, and end of treatment vs visit interactions as fixed effects, with an unstructured covariance structure for participants.
For each individual the mean change from baseline was calculated as AUC by the trapezoidal method, and the LS means ± SE were estimated from an ANCOVA model with mean change as the dependent variable, baseline level as the covariate and treatment as a fixed effect. Each tertile within each of the active treatment groups was compared with the placebo group, with the level of significance adjusted for multiple comparisons using the Dunnett method. Assessment of difference between mean change from baseline compared with zero was based on the LS mean ± SE.
All statistical calculations were performed using the SAS software package version 9.3 or higher for Windows (SAS Institute, Cary, NC, USA). Graphing was performed using GraphPad Prism version 7.01 for Windows (GraphPad, La Jolla, CA, USA).
Results
Serum endotrophin is correlated with metabolic measures
The efficacy (as assessed by metabolic measures) and safety data of the treatments used in the BALLET trial have been published elsewhere [23]. The correlations of baseline levels of endotrophin with variables associated with the metabolic syndrome are presented in Table 1. Endotrophin levels were significantly correlated with HOMA-IR, FLI, triacylglycerol and BMI, but not with FSG and HbA1c (Table 1), supporting findings that endotrophin is indeed an adipokine, related to adipocyte function, fat mass and some aspects of insulin sensitivity. Endotrophin levels were not correlated with cholesterol.
In the placebo group, the correlations observed at baseline between endotrophin and the metabolic variables, FSG, HbA1c, HOMA-IR, FLI and BMI (see Table 2), were maintained at the end of the 26 week treatment period (Table 3). However, in the PPARγ agonist treatment groups, the correlation between HOMA-IR and endotrophin was eliminated, while the correlation between endotrophin and BMI or FLI persisted and even showed a trend towards being stronger (Table 3).
Endotrophin identifies responders to glitazone therapy
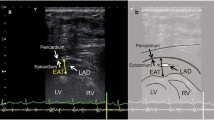
When assessing the change from baseline in FSG over time (Fig. 1a–d) and mean per cent change in FSG over time (Fig. 1e–h), from baseline to end of treatment (week 26), it was apparent that FSG was significantly reduced by ∼2.5 mmol/l compared with baseline and placebo for participants with endotrophin in the upper two tertiles in all three glitazone treatment groups. A less marked reduction in FSG, compared with baseline and placebo, was observed for participants in the lower tertile.
Mean change in FSG over time from baseline to end of treatment (week 26) in the (a) placebo, (b) balaglitazone 10 mg, (c) balaglitazone 20 mg and (d) pioglitazone 45 mg groups. Data were analysed using a mixed-effect repeated measures model for each tertile of baseline endotrophin. Mean absolute change in FSG from baseline to end of treatment (week 26) in the (e) placebo, (f) balaglitazone 10 mg, (g) balaglitazone 20 mg and (h) pioglitazone 45 mg groups. White circles, tertile 1; grey circles, tertile 2; black circles, tertile 3. T1, tertile 1; T2, tertile 2; T3, tertile 3. All data are LS estimates (± SE). *p < 0.05, **p < 0.01, ***p < 0.001, Dunnett-adjusted level of significance of treatment effect against placebo; § p < 0.05, §§§ p < 0.001, level of significance of change from baseline
When response to therapy was investigated, patients in the upper two tertiles for baseline serum endotrophin were more likely to show a clinically significant response to glitazone therapy at week 26, compared with patients in the lower tertile. Furthermore, compared with participants in the lower tertile, those in the upper two tertiles had an OR of 3.83 (95% CI 1.62, 9.04) (p < 001) and 3.85 (95% CI 1.94, 7.61) (p < 0.001) for achieving a reduction in HbA1c of ≥1% or ≥0.5%, respectively (Fig. 2a). The power of baseline serum endotrophin for predicting the probability of responding to treatment is illustrated in Fig. 2b. For example, at a baseline serum endotrophin level of 4 ng/ml, the predicted probability of achieving a treatment response of a reduction in HbA1c ≥0.5% is 26%, whereas an endotrophin level of 10 ng/ml at baseline is associated with a predicted probability of treatment response of ∼65%. For changes in HOMA-IR during therapy, individuals in the upper tertiles again showed the strongest numerical improvement (Fig. 3a–c), albeit non-significant. Interestingly, despite the variable efficacy of therapy between tertiles there were no marked differences in weight gain (data not shown).
(a) Responder analysis at week 26 based on a reduction (compared to baseline) in blood HbA1c of ≥0.5% (black circle, solid line), or ≥1.0% (grey circle, dashed line). ORs (95% CI) were calculated for response to therapy based on baseline endotrophin level. The analysis compares the upper two tertiles vs the lowest tertile for treatment groups combined. **p < 0.01, ***p < 0.001. (b) Power of baseline endotrophin levels for predicting the probability of treatment response. Data from treatment groups were combined and analysed in a logistic regression model including baseline HbA1c and baseline endotrophin as predictors. Based on regression estimates the predicted probability of endotrophin was calculated at a mean baseline level of HbA1c at 8.64% (70.9 mmol/mol)
Mean absolute change from baseline in HOMA-IR during the 26 week treatment period in participants stratified into (a) tertile 1, (b) tertile 2 or (c) tertile 3 based on baseline endotrophin levels. White bars, placebo; light grey bars, balaglitazone 10 mg; dark grey bars, balaglitazone 20 mg; black bars, pioglitazone 45 mg. All data are LS estimates (± SE). *p < 0.05, Dunnett-adjusted level of significance of treatment effect against placebo; § p < 0.05, level of significance of change from baseline
The effect on serum endotrophin as a function of treatment and time expressed as percentage change relative to baseline is shown in Fig. 4a–d. Figure 4e–h shows the mean change from baseline at 26-weeks. Overall, an increase in serum endotrophin was observed in the placebo group and in all three glitazone treatment groups, with the exceptions of the placebo and balaglitazone 10 mg groups within the uppermost tertile.
Values relative to baseline serum endotrophin level during the 26 week treatment period. (a) Relative level in the placebo, (b) balaglitazone 10 mg, (c) balaglitazone 20 mg and (d) pioglitazone 45 mg groups. Data were analysed in a mixed-effect repeated measures model. Data are presented as LS estimates (± SE), calculated at the geometric mean level of baseline endotrophin within each tertile: white circles, 5.2 ng/ml; grey circles, 6.9 ng/ml; black circles, 9.8 ng/ml. Mean change in endotrophin relative to baseline in the (e) placebo, (f) balaglitazone 10 mg, (g) balaglitazone 20 mg and (h) pioglitazone 45 mg groups. T1, tertile 1; T2, tertile 2; T3, tertile 3. All data are LS estimates (± SE). *p < 0.05, Dunnett-adjusted level of significance of treatment effect against placebo; § p < 0.05, §§ p < 0.01, §§§ p < 0.001, level of significance of change from baseline
Adverse effects
Lower leg oedema, measured as volume increase due to water displacement, was correlated with baseline serum endotrophin level. Certain glitazone therapies led to increased lower leg volume in the lower and middle tertiles, while there were no differences between the treatment and placebo groups in the upper tertile (Fig. 5). The AEs and severe AEs (SAEs) observed within the different tertiles are presented in Table 4. There were no significant differences in the occurrence of AEs or SAEs between the three active treatment groups when stratified according to endotrophin level. The SAEs presented in Table 4 differ from lower leg oedema (reported in Fig. 5) since lower leg volume is a quantitative measure and oedema is a patient-reported outcome.
Absolute mean change in lower leg volume from baseline to 26 weeks following treatment in participants stratified into (a) tertile 1, (b) tertile 2 or (c) tertile 3 based on baseline endotrophin levels. White bars, placebo; light grey bars, balaglitazone 10 mg; dark grey bars, balaglitazone 20 mg; black bars, pioglitazone 45 mg. All data are LS estimates (± SE). *p < 0.05, **p < 0.01, Dunnett-adjusted level of significance of treatment effect against placebo; § p < 0.05, §§§ p < 0.001, level of significance of change from baseline
Discussion
The ECM is increasingly recognised as a dynamic structure that does not only lend stability and spatial organisation to multicellular tissue and organisms, but that also transmits signals of differentiation, growth and migration to neighbouring cells. Moreover, the ECM can serve as an endocrine organ due to the signalling potential of certain fragments released by proteolysis, creating ligands with paracrine and potential endocrine functions [3]. Endotrophin (Pro-C6) is a soluble fragment of the C-terminal α3 chain of type VI procollagen that is released by naturally occurring proteolysis [4, 8, 22, 26]. Here we demonstrate that serum endotrophin levels are predictive of a response to the insulin sensitisers, pioglitazone and balaglitazone, in patients with type 2 diabetes. Individuals within the upper two tertiles for baseline endotrophin serum levels (tertile two, 6.3–7.7 ng/ml and tertile three, ≥7.8 ng/ml) were four times more likely to respond to treatment, compared with patients in the lower tertile (≤6.2 ng/ml baseline serum endotrophin). Since the glitazones are associated with safety concerns, such as non-fatal heart failure and bone fractures [15, 27–31], identification of individuals who will gain the most benefit from treatment and also the fewest AEs is crucial for the continued use of these drugs, which are still considered highly effective insulin sensitisers. Participants in the upper two tertiles who responded to treatment with a reduction in FPG and HbA1c levels were at a reduced risk of developing lower leg oedema, a major AE associated with glitazone treatment. These efficacy and safety data are highly relevant for predicting benefit-to-risk ratios for patients treated with glitazones; this should also apply when the medications are considered for other indications, such as liver disease [32–34].
In animal models, endotrophin levels have been shown to reflect insulin sensitivity, food intake and energy balance, as well as angiogenesis [4, 5, 8]. Accordingly, suppression of endotrophin improves insulin sensitivity and attenuated adipose tissue inflammation in animals [8]. This correlates well with our findings that elevated serum endotrophin levels are indicative of a response to PPARγ agonists. Furthermore, mRNA levels of the endotrophin precursor procollagen α3(VI) are upregulated in obese adipose tissue, paralleling adipose tissue inflammation and fibrosis [9]. The ECM and its products, especially procollagen type VI and endotrophin, may be of particular relevance in fatty liver, including in the severe form of the disease, non-alcoholic steatohepatitis (NASH). NASH is a metabolic-fibrotic disorder of the liver that shows at least a partial overlap with type 2 diabetes [32–34]. Accordingly, we expect that this novel biomarker should assist in the diagnosis and management of NASH patients where insulin sensitisers may be beneficial for subpopulations, both for the treatment of insulin resistance and liver fibrosis. Here, ECM components, in particular collagens/collagen type VI, and their functional role in the transition of fatty liver to overt fibrotic NASH needs to be further investigated.
In line with this, in the current study we observed a strong correlation between serum triacylglycerol and FLI, an index that correlates with NASH inflammatory activity and predicts more severe liver fibrosis [25]. In support of a role for type VI collagen in NASH-related fibrosis, studies have demonstrated its prominent expression in areas of active scar formation [35, 36], and elevated serum levels of the collagen VI core structure (which lacks the endotrophin domain) have been shown to be associated with advanced liver fibrosis in rodents [37], humans [38–41], and with elevated portal pressure [42]. The expression of procollagen α3(VI) is regulated by PPARγ and our findings are in alignment with this. In fact, procollagen α3(VI) mRNA is suppressed by PPARγ, as demonstrated by an increase in procollagen α3(VI) mRNA expression in adipocyte cultures treated with siRNA against PPARγ [9] and by a decrease in its transcripts in subcutaneous adipose tissue of individuals with type 2 diabetes treated with the PPARγ agonist pioglitazone, especially in patients with high baseline tissue levels of procollagen α3(VI) mRNA [12]. These data may in part explain the change in correlation, from baseline to the end of glitazone treatment, between endotrophin serum levels and HbA1c or HOMA-IR, and in particular the lack of a correlation between endotrophin and the metabolic variables. Another clinical study provides further supportive evidence by showing that tissue endotrophin levels in obese individuals correlated with chronic inflammation and systemic insulin resistance [10, 26].
Generally, the ECM has, until now, been considered to be a passive scaffold. Type VI collagen has mostly been recognised through mutations in the genes COL6A1, COL6A2 and COL6A3 that encode its three constituent chains. These mutations cause muscle disorders, such as Bethlem myopathy, Ullrich congenital muscular dystrophy, limb-girdle muscular dystrophy and autosomal recessive myosclerosis [43–46]. This provides an interesting link to metabolic dysfunction, since type VI collagen mutations are associated with muscle abnormalities and muscle represents an important regulator of insulin resistance. Therefore, the available evidence strongly suggests that collagen type VI is more than a passive ECM component, but an important mediator of adipose (and liver) metabolic dysfunction related to insulin resistance, type 2 diabetes and NASH.
Of note, the measurement of only one standard biochemical variable is a weakness of the current study; because of limited sample availability we were only able to assess endotrophin levels in serum for comparisons with HbA1c, limiting the possibility of investigating other potential biomarkers for response to treatment.
In conclusion, elevated circulating levels of endotrophin, predominantly derived from adipocytes and adipose tissue, are correlated with insulin resistance and are predictive of the response to insulin sensitisers. This enables the identification and monitoring of patients who will respond optimally to an insulin sensitiser, improving the benefit-to-risk ratio for PPARγ agonists in the treatment of type 2 diabetes and possibly NASH.
Abbreviations
- AE:
-
Adverse effect
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- DXA:
-
Dual-energy x-ray absorptiometry
- ECM:
-
Extracellular matrix
- GGT:
-
Gamma-glutamyl transferase
- GLP-1:
-
Glucagon-like peptide 1
- NASH:
-
Non-alcoholic steatohepatitis
- PHC:
-
Personalised healthcare
- PPARγ:
-
Peroxisome proliferator-activated receptor gamma
- Pro-C6:
-
C-terminal pro-peptide of the α3 type IV collagen chain
- SAE:
-
Severe adverse effect
- TZDs:
-
Thiazolidinediones
References
World Health Organization (2008) Diabetes. Fact sheet no 312. World Health Organization, Geneva
Krentz AJ, Patel MB, Bailey CJ (2008) New drugs for type 2 diabetes mellitus: what is their place in therapy? Drugs 68:2131–2162
Karsdal MA, Manon-Jensen T, Genovese F et al (2015) Novel insights into the function and dynamics of extracellular matrix in liver fibrosis. Am J Physiol Gastrointest Liver Physiol 308:G807–G830
Park J, Scherer PE (2012) Adipocyte-derived endotrophin promotes malignant tumor progression. J Clin Invest 122:4243–4256
Mak KM, Sehgal P, Harris CK (2014) Type VI collagen: its biology and value as a biomarker of hepatic fibrosis. Austin Biomark Diagn 1:id1012
Aigner T, Hambach L, Soder S, Schlotzer-Schrehardt U, Poschl E (2002) The C5 domain of COL6A3 is cleaved off from the Col6 fibrils immediately after secretion. Biochem Biophys Res Commun 290:743–748
Lamande SR, Morgelin M, Adams NE, Selan C, Allen JM (2006) The C5 domain of the collagen VI alpha3(VI) chain is critical for extracellular microfibril formation and is present in the extracellular matrix of cultured cells. J Biol Chem 281:16607–16614
Sun K, Park J, Gupta OT et al (2014) Endotrophin triggers adipose tissue fibrosis and metabolic dysfunction. Nat Commun 5:3485
Dankel SN, Svard J, Mattha S et al (2014) COL6A3 expression in adipocytes associates with insulin resistance and depends on PPARγ and adipocyte size. Obesity (Silver Spring) 22:1807–1813
Park J, Scherer PE (2013) Endotrophin in the tumor stroma: a new therapeutic target for breast cancer? Expert Rev Anticancer Ther 13:111–113
Khan T, Muise ES, Iyengar P et al (2009) Metabolic dysregulation and adipose tissue fibrosis: role of collagen VI. Mol Cell Biol 29:1575–1591
Pasarica M, Gowronska-Kozak B, Burk D et al (2009) Adipose tissue collagen VI in obesity. J Clin Endocrinol Metab 94:5155–5162
Cho N, Momose Y (2008) Peroxisome proliferator-activated receptor gamma agonists as insulin sensitizers: from the discovery to recent progress. Curr Top Med Chem 8:1483–1507
Charbonnel B, DeFronzo R, Davidson J et al (2010) Pioglitazone use in combination with insulin in the prospective pioglitazone clinical trial in macrovascular events study (PROactive19). J Clin Endocrinol Metab 95:2163–2171
Home PD, Pocock SJ, Beck-Nielsen H et al (2009) Rosiglitazone evaluated for cardiovascular outcomes in oral agent combination therapy for type 2 diabetes (RECORD): a multicentre, randomised, open-label trial. Lancet 373:2125–2135
Takada I, Suzawa M, Matsumoto K, Kato S (2007) Suppression of PPAR transactivation switches cell fate of bone marrow stem cells from adipocytes into osteoblasts. Ann N Y Acad Sci 1116:182–195
Karalliedde J, Buckingham RE (2007) Thiazolidinediones and their fluid-related adverse effects: facts, fiction and putative management strategies. Drug Saf 30:741–753
Soroceanu MA, Miao D, Bai XY, Su H, Goltzman D, Karaplis AC (2004) Rosiglitazone impacts negatively on bone by promoting osteoblast/osteocyte apoptosis. J Endocrinol 183:203–216
Berger JP, Akiyama TE, Meinke PT (2005) PPARs: therapeutic targets for metabolic disease. Trends Pharmacol Sci 26:244–251
Agrawal R, Jain P, Dikshit SN (2012) Balaglitazone: a second generation peroxisome proliferator-activated receptor (PPAR) gamma (γ) agonist. Mini Rev Med Chem 12:87–97
Larsen PJ, Lykkegaard K, Larsen LK et al (2008) Dissociation of antihyperglycaemic and adverse effects of partial perioxisome proliferator-activated receptor (PPAR-γ) agonist balaglitazone. Eur J Pharmacol 596:173–179
Sun S, Henriksen K, Karsdal MA et al (2015) Collagen type III and VI turnover in response to long-term immobilization. PLoS One 10, e0144525
Henriksen K, Byrjalsen I, Qvist P et al (2011) Efficacy and safety of the PPARγ partial agonist balaglitazone compared with pioglitazone and placebo: a phase III, randomized, parallel-group study in patients with type 2 diabetes on stable insulin therapy. Diabetes Metab Res Rev 27:392–401
Feigh M, Henriksen K, Andreassen KV et al (2011) A novel oral form of salmon calcitonin improves glucose homeostasis and reduces body weight in diet-induced obese rats. Diabetes Obes Metab 13:911–920
Bedogni G, Bellentani S, Miglioli L et al (2006) The Fatty Liver Index: a simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol 6:33
Park J, Morley TS, Scherer PE (2013) Inhibition of endotrophin, a cleavage product of collagen VI, confers cisplatin sensitivity to tumours. EMBO Mol Med 5:935–948
Lincoff AM, Wolski K, Nicholls SJ, Nissen SE (2007) Pioglitazone and risk of cardiovascular events in patients with type 2 diabetes mellitus: a meta-analysis of randomized trials. JAMA 298:1180–1188
Erdmann E, Charbonnel B, Wilcox RG et al (2007) Pioglitazone use and heart failure in patients with type 2 diabetes and preexisting cardiovascular disease: data from the PROactive study (PROactive 08). Diabetes Care 30:2773–2778
Singh S, Loke YK, Furberg CD (2007) Long-term risk of cardiovascular events with rosiglitazone: a meta-analysis. JAMA 298:1189–1195
McDonough AK, Rosenthal RS, Cao X, Saag KG (2008) The effect of thiazolidinediones on BMD and osteoporosis. Nat Clin Pract Endocrinol Metab 4:507–513
Douglas IJ, Evans SJ, Pocock S, Smeeth L (2009) The risk of fractures associated with thiazolidinediones: a self-controlled case-series study. PLoS Med 6, e1000154
Bell LN, Wang J, Muralidharan S et al (2012) Relationship between adipose tissue insulin resistance and liver histology in nonalcoholic steatohepatitis: a pioglitazone versus vitamin E versus placebo for the treatment of nondiabetic patients with nonalcoholic steatohepatitis trial follow-up study. Hepatology 56:1311–1318
Sanyal AJ, Chalasani N, Kowdley KV et al (2010) Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N Engl J Med 362:1675–1685
Sanyal AJ, Friedman SL, McCullough AJ, Dimick-Santos L (2015) Challenges and opportunities in drug and biomarker development for nonalcoholic steatohepatitis: findings and recommendations from an American Association for the Study of Liver Diseases-U.S. Food and Drug Administration Joint Workshop. Hepatology 61:1392–1405
Griffiths MR, Shepherd M, Ferrier R, Schuppan D, James OF, Burt AD (1992) Light microscopic and ultrastructural distribution of type VI collagen in human liver: alterations in chronic biliary disease. Histopathology 21:335–344
Burt AD, Griffiths MR, Schuppan D, Voss B, MacSween RN (1990) Ultrastructural localization of extracellular matrix proteins in liver biopsies using ultracryomicrotomy and immuno-gold labelling. Histopathology 16:53–58
Veidal SS, Karsdal MA, Vassiliadis E et al (2011) MMP mediated degradation of type VI collagen is highly associated with liver fibrosis—identification and validation of a novel biochemical marker assay. PLoS One 6, e24753
Lebensztejn DM, Sobaniec-Lotowska ME, Kaczmarski M, Voelker M, Schuppan D (2006) Matrix-derived serum markers in monitoring liver fibrosis in children with chronic hepatitis B treated with interferon alpha. World J Gastroenterol 12:3338–3343
Lebensztejn DM, Sobaniec-Lotowska ME, Bauer M, Kaczmarski M, Voelker M, Schuppan D (2005) Serum fibrosis markers as predictors of an antifibrotic effect of interferon alfa in children with chronic hepatitis B. Eur J Gastroenterol Hepatol 17:843–848
Stickel F, Urbaschek R, Schuppan D et al (2001) Serum collagen type VI and XIV and hyaluronic acid as early indicators for altered connective tissue turnover in alcoholic liver disease. Dig Dis Sci 46:2025–2032
Shahin M, Schuppan D, Waldherr R et al (1992) Serum procollagen peptides and collagen type VI for the assessment of activity and degree of hepatic fibrosis in schistosomiasis and alcoholic liver disease. Hepatology 15:637–644
Leeming DJ, Karsdal MA, Byrjalsen I et al (2013) Novel serological neo-epitope markers of extracellular matrix proteins for the detection of portal hypertension. Aliment Pharmacol Ther 38:1086–1096
Lampe AK, Bushby KM (2005) Collagen VI related muscle disorders. J Med Genet 42:673–685
Lampe AK, Zou Y, Sudano D et al (2008) Exon skipping mutations in collagen VI are common and are predictive for severity and inheritance. Hum Mutat 29:809–822
Bonaldo P, Braghetta P, Zanetti M, Piccolo S, Volpin D, Bressan GM (1998) Collagen VI deficiency induces early onset myopathy in the mouse: an animal model for Bethlem myopathy. Hum Mol Genet 7:2135–2140
Bushby KM, Collins J, Hicks D (2014) Collagen type VI myopathies. Adv Exp Med Biol 802:185–199
Acknowledgements
The Danish Research foundation is acknowledged for supporting the work involved in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The Danish research foundation is acknowledged for support of this study. Funding was received from ‘Den Danske Forskningsfond’ and the EPoS project, part of the European Union’s Horizon 2020 research and innovation programme (No. 634413).
Duality of interest
MAK, KH, BJR and CC are employees of, and own stocks in Nordic Bioscience. FG, IB, MJN and DJL are employees of Nordic Bioscience. DS declares that there is no duality of interest associated with this manuscript. The study sponsor was not involved in the design of the study; the collection; analysis and interpretation of data; writing of the manuscript or the decision to submit the manuscript for publication.
Contribution statement
MAK, DS, CC, IB, MJN, KH, BJR, FG and DJL all made substantial contributions to conception and design, acquisition of data, as well as analysis and interpretation of data. MAK, DS, CC, IB, MJN, KH, BJR and DJL all were part of drafting the article and have revised it critically for important intellectual content. FG also provided expert knowledge on type VI collagen and endotrophin. All authors provided substantial contributions to conception and design, acquisition of data and analysis and interpretation of data, drafting the article and revising it critically for important intellectual content, and approval of the version to be published. MAK is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Rights and permissions
About this article
Cite this article
Karsdal, M.A., Henriksen, K., Genovese, F. et al. Serum endotrophin identifies optimal responders to PPARγ agonists in type 2 diabetes. Diabetologia 60, 50–59 (2017). https://doi.org/10.1007/s00125-016-4094-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-016-4094-1