Abstract
Aims/hypothesis
Insufficient insulin release and hyperglucagonaemia are culprits in type 2 diabetes. Cocaine- and amphetamine-regulated transcript (CART, encoded by Cartpt) affects islet hormone secretion and beta cell survival in vitro in rats, and Cart −/− mice have diminished insulin secretion. We aimed to test if CART is differentially regulated in human type 2 diabetic islets and if CART affects insulin and glucagon secretion in vitro in humans and in vivo in mice.
Methods
CART expression was assessed in human type 2 diabetic and non-diabetic control pancreases and rodent models of diabetes. Insulin and glucagon secretion was examined in isolated islets and in vivo in mice. Ca2+ oscillation patterns and exocytosis were studied in mouse islets.
Results
We report an important role of CART in human islet function and glucose homeostasis in mice. CART was found to be expressed in human alpha and beta cells and in a subpopulation of mouse beta cells. Notably, CART expression was several fold higher in islets of type 2 diabetic humans and rodents. CART increased insulin secretion in vivo in mice and in human and mouse islets. Furthermore, CART increased beta cell exocytosis, altered the glucose-induced Ca2+ signalling pattern in mouse islets from fast to slow oscillations and improved synchronisation of the oscillations between different islet regions. Finally, CART reduced glucagon secretion in human and mouse islets, as well as in vivo in mice via diminished alpha cell exocytosis.
Conclusions/interpretation
We conclude that CART is a regulator of glucose homeostasis and could play an important role in the pathophysiology of type 2 diabetes. Based on the ability of CART to increase insulin secretion and reduce glucagon secretion, CART-based agents could be a therapeutic modality in type 2 diabetes.
Similar content being viewed by others
Introduction
Insufficient insulin secretion and exaggerated glucagon secretion are key features of type 2 diabetes [1–3]. The pancreatic islets are vital regulators of glucose homeostasis, and islet dysfunction is a primary cause of type 2 diabetes [4]. Islet hormone secretion is controlled by the metabolic state, e.g. plasma levels of glucose, amino acids and fatty acids. Furthermore, the islets are influenced by regulatory peptides expressed in islet cells or released from nerve fibres innervating the islets [5].
The anorexigenic regulatory peptide cocaine- and amphetamine-regulated transcript (CART) [6–10] is expressed in islet cells and islet nerve fibres in animals [11–17]. CART regulates islet hormone secretion and protects beta cells from glucotoxicity-induced cell death in vitro in rat islets [12, 18]. Importantly, CART is required for normal islet function: Cart −/− mice exhibit islet dysfunction with diminished insulin secretion and reduced glucose elimination [15]. On the other hand, expression of CART is augmented in beta cells in rat models of type 2 diabetes [12]. Moreover, Cart −/− mice are obese [15, 19], and genetic variations in CARTPT associate with obesity in humans [20, 21].
It is not known if CART affects human islet function or if CART is expressed in human islets and is affected by type 2 diabetes. Furthermore, it is not known how CART affects glucose homeostasis in vivo. To address this, we examined islet CART expression in non-diabetic and type 2 diabetic individuals, as well as the effect of CART on islet hormone secretion in human islets. Furthermore, we studied the effect of exogenous CART in mice to pinpoint the mechanisms underlying the effect of CART on insulin secretion.
Methods
Human tissue
Human pancreases from nine type 2 diabetic patients (five men, four women; median age 54 years, BMI 28.9 ± 7 kg/m2) and ten controls (four men, six women; median age 56 years, BMI 25.8 ± 2 kg/m2) were used for morphometric analysis. Human islets were provided by the Nordic Network for Clinical Islet Transplantation, Uppsala University. All procedures were approved by Uppsala and Lund University ethics committees.
CART peptide
Rat CART55-102 peptide (American Peptide, Sunnyvale, CA, USA or gift from L. Thim [Novo Nordisk, Målöv, Denmark]) was used.
Immunocytochemistry, in situ hybridisation and image analysis
Immunocytochemistry was performed using characterised antibodies as detailed [13, 22]. The specificity of CART antibodies (Cocalico, Stevens, PA, USA) was verified in Cart −/− mice and with pre-absorption with CART55-102 [23]. For in situ hybridisation (ISH), 30-mer oligodeoxyribonucleotide probes for Cart mRNA were used in human [24] and rat [12] specimens as described previously [25]. Hybridisation in the presence of excess unlabelled probe on adjacent sections was used as a negative control. CART-immunoreactive alpha cells and beta cells, and CART ISH-labelled area/whole-islet area were quantified blinded in the indicated samples in all islets in three separate sections as described [12].
Western blot
Western blot was performed as described previously [26] using CART primary antibody (Cocalico) diluted 1:1000 with CART55-102 (Novo Nordisk) as a positive control.
Animal models of type 2 diabetes
Experiments were approved by the regional animal ethics committee and the Guide for the care and use of laboratory animals (8th edn) was followed. Female Sprague Dawley rats (225 g) were used. Six rats received dexamethasone (DEX), 2 mg/kg/day i.p. for 10 days [12, 27]. Six rats received DEX and insulin detemir (Levemir, Novo Nordisk), 10 U/day for 10 days. Controls (n = 6) received NaCl 154 mmol/l. In addition, the genetically modified mouse strains (1) HNF1α dominant-negative (Hnf1α dn) mice [28] and (2) ob/ob mice with respectively matched control mice, as well as C57Bl/6J mice (Taconic, Bomholt, Denmark) fed a high-fat diet (HFD) or control diet for 6 months were used (all female mice, aged 10–14 weeks, n = 5–8 in each group) [29]. The pancreases were processed as described previously [12].
Real-time quantitative PCR
Total RNA was isolated using All Prep DNA/RNA kit (Qiagen, Hilden, Germany). RNA, 1 μg, was reverse-transcribed to cDNA with QuantiTect Reverse Transcription kit (Qiagen). Quantitative RT-PCR was performed using the ABI Prism 7900 HT system (Applied Biosystems, Foster City, CA, USA) with TaqMan technology and assay Hs00182861_m1 for Cart and 4333768F for Hprt1, which served as an endogenous control. Gene expression was analysed with the ΔΔCt method.
In vitro islet studies
Secretion studies in human and mouse islets (1 h incubations) with insulin secretagogues, with and without CART55-102 as indicated, were performed as described previously [15, 30, 31]. One experiment represents one donor/animal, with 6–8 technical repeats for each experiment. For Cart mRNA expression studies, rat islets were cultured for 24 h in 5, 11.1 or 25 mmol/l glucose in RPMI 1640 medium (1% serum).
IVGTT
IVGTT was performed as previously described [15] in female C57Bl/6J mice with or without 150 nmol/kg CART55-102 and 4 nmol/kg glucagon-like peptide 1 (GLP-1) co-injected, i.v, with glucose, 0.75 g/kg. Controls received NaCl. Acute insulin response (AIR) was calculated as mean suprabasal insulin level of insulin at mins 1 and 5 (i.e. [ins5 min + ins1 min]/2 – ins0 min). The glucose elimination rate (KG) was calculated as the slope for 1-20 min of the logarithmic transformation of individual plasma glucose values [15].
Glucagon secretion in vivo
Female C57Bl/6J mice were fasted overnight and given i.v. CART55-102, 150 nmol/kg. Blood samples were taken from the retro-orbital plexus after 2 min. Controls received NaCl.
Electrophysiology
Depolarisation-evoked exocytosis was recorded by capacitance measurements using standard whole-cell configuration with or without CART55-102 as indicated [30]. Islets from female C57Bl/6J mice were used. Exocytosis was induced by 500 ms depolarisation from −70 mV to 0 mV.
Ca2+ signalling and analysis of cell synchronisation
Changes in the cytoplasmic Ca2+ concentration ([Ca2+]i) were recorded as previously described [32]. In brief, mouse islets or islet cells were loaded with Fura-2 LR acetoxymethyl ester (TEFLabs, Austin, TX, USA) and transferred to poly-l-lysine-coated coverslips in a 50 μl chamber on the stage of an Eclipse TE2000U microscope (Nikon, Tokyo, Japan) equipped for ratiometric epifluorescence recordings of [Ca2+]i [32]. The chamber was superfused at 160 μl/min with 37°C buffer containing 138 mmol/l NaCl, 4.8 mmol/l KCl, 1.2 mmol/l MgCl2, 1.3 mmol/l CaCl2, 3 mmol/l glucose and 25 mmol/l HEPES with pH set to 7.40, and 1 mg/ml BSA. [Ca2+]i is expressed as the background-corrected Fura-2 LR 340/380 nm fluorescence excitation ratio.
To estimate the synchronisation of [Ca2+]i signals between different non-overlapping regions-of-interest (ROI) in the islet, we calculated the linear correlation (Pearson’s r) between all possible ROI pairs and displayed the correlation coefficients in a matrix. The correlation matrices were subsequently used to construct undirected graphs representing functional connectivity. These graphs show the geometric location of each ROI with lines added between the ROI pairs with significant correlation coefficients (p < 0.001) equal to or exceeding a threshold value of 0.8. Correlation analyses and the construction of correlation matrices and connectivity maps were performed with standard tools using Igor Pro software version 6.37 (Wavemetrics, Lake Oswego, OR, USA).
Glucose insulin and glucagon measurements
Glucose was measured using Infinity Glucose (Ox) (Thermo Scientific, Lexington, MA, USA) [15]. Insulin and glucagon levels were determined with ELISA (Mercodia, Uppsala, Sweden).
Statistics and overall design for experimental studies
Human insulin secretion data were analysed using a Wilcoxon signed-rank test. All other data were analysed using one-way ANOVA, followed by Bonferroni’s test, or unpaired Student’s t test. Data are expressed as means (SEM). All experiments were performed and analysed in a randomised and blinded fashion when possible. Outliers were identified using Grubbs’ test for outliers.
Results
CART is expressed in human beta cells and alpha cells
Islet CART expression was demonstrated using immunocytochemistry (ICC) (Fig. 1a), ISH (Fig. 1b, electronic supplementary material [ESM] Fig. 1) and quantitative PCR (n = 10, not shown). Western blot confirmed processing of active CART55-102 (Fig. 1c) and ICC localised CART to alpha and beta cells (Fig. 1a).
CART is elevated in islets of diabetic humans and mice. (a) Human pancreatic sections from non-diabetic and type 2 diabetic donors, triple immunostained for CART, insulin and glucagon. CART is localised to alpha (arrows) and beta cells (arrowheads) in both a type 2 diabetic patient and a control (scale bar, 100 μm). (b) In situ hybridisation showing higher expression of CART mRNA in a type 2 diabetic patient (arrows indicate labelling, scale bar, 20 μm). (c) Western blot showing that human islet CART is processed to biologically active CART55-102 in isolates containing 50% islets (lane 1) and 75% islets (lane 2). (d–f) Islets from type 2 diabetic patients (n = 9) exhibit higher CART mRNA expression (quantification of in situ hybridisation, relative units labelled area/islet area) (d) and more CART-positive beta cells (e) and CART-positive alpha cells (f) than controls (n = 10). (g) Double-immunostaining for CART and insulin showing that CART is upregulated in beta cells of ob/ob mice compared with wild type. Arrows indicate beta cells with CART (scale bar, 50 μm). (h–j) The number of CART-positive beta cells is elevated several fold in three mouse models of type 2 diabetes: ob/ob (h), HFD-fed mice (i) and Hnf1α dn mice (j), compared with controls. n = 5–8 per group. *p < 0.05 and **p < 0.01. C, control; peptide, biologically active CART55-102; ND, normal diet; RU, relative units; T2D, type 2 diabetes; WT, wild type
Islet CART expression is increased in type 2 diabetic patients and mouse models of diabetes
CART mRNA expression was threefold higher in islets from type 2 diabetic patients (n = 9; p < 0.009) (Fig. 1b, d) and type 2 diabetic patients had threefold more CART-positive beta cells (p < 0.008; Fig. 1a, e) and twofold more CART-positive alpha cells (p < 0.007) (Fig 1a, f) than controls (n = 10). CART-positive beta cells were also several fold more abundant in three mouse models of diabetes (Fig. 1h-j), whereas CART was absent in mouse alpha cells (ESM Fig. 2).
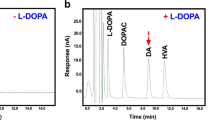
Beta cell CART is regulated by glucose in vivo and in vitro in rats
As CART expression was elevated in islets from type 2 diabetic patients and diabetic mice, we hypothesised that islet CART expression is regulated by glucose. To test this, we used DEX-treated rats (DEX-rats) previously shown to have overexpressed beta cell CART [12], and DEX-rats treated with insulin. DEX-rats displayed 50% higher plasma glucose than controls (p < 0.05) and more CART-positive beta cells (p < 4 × 10−6, Fig. 2a, b), as well as upregulated islet Cart mRNA (p < 0.001, Fig. 2c and ESM Fig. 3); CART staining was evident in delta cells and inert to DEX treatment (Fig. 2a), as previously reported [12] and CART was not expressed in alpha or PP cells (ESM Fig. 4). Insulin treatment of DEX-rats normalised glucose levels (p < 0.05 vs DEX-rats) and prevented the upregulation of beta cell CART (Fig. 2a–c). The frequency of CART-positive beta cells correlated positively with plasma glucose (r 2 = 0.28, p < 0.02) and Cart mRNA increased in rat islets cultured in 11 mmol/l (2.8-fold, p < 0.03) and 25 mmol/l (3.2-fold, p < 0.03) compared with 5 mmol/l glucose (Fig. 2d). Western blot confirmed that biologically active CART55-102 is processed in DEX-rats and controls (Fig. 2e). Thus, beta cell CART expression is increased by hyperglycaemia in vivo and in vitro.
Beta cell CART is regulated by glucose in vivo and in vitro in rats. (a) Triple-immunostaining for CART, insulin and somatostatin in control rat, DEX-rat and insulin (INS)-treated DEX-rat. White arrows indicate beta cells and red arrows delta cells with CART immunostaining (scale bar, 100 μm). (b) CART-positive beta cells (quantification of immunohistochemistry) and (c) islet Cart mRNA (quantification of in situ hybridisation relative units labelled area/islet area) are upregulated in DEX-rats (n = 6), and insulin treatment (n = 6) prevents the upregulation. (d) Cart mRNA expression is increased in isolated rat islets after 24 h culture in 11 mmol/l and 25 mmol/l vs 5 mmol/l glucose (quantitative PCR, ΔΔCt, relative to 11 mmol/l, n = 5). (e) Western blot showing that islet CART in DEX-rats and controls is the biologically active form, CART55-102. *p < 0.05 and ***p < 0.001. C, control; HT, rat hypothalamus positive control; RU, relative units; T2D, type 2 diabetes
CART stimulates insulin secretion and inhibits glucagon secretion in human islets
As it is not known whether CART affects insulin or glucagon secretion in humans, we treated human islets with CART during 1 h static incubations. CART (100 nmol/l) enhanced glucose-stimulated insulin secretion (GSIS) by 24 ± 11% (n = 19 donors, p < 0.03) at 16.7 mmol/l glucose (Fig. 3a). This dose was previously shown to increase insulin secretion in INS-1 (832/13) cells [12]. Importantly, CART also stimulated GSIS in islets from diabetic donors (22 ± 5%, n = 7 donors, p < 0.02) (Fig. 3b). CART had no effect on insulin secretion at low glucose (2.8 mmol/l) and a slight but non-significant effect at intermediate glucose (8.3 mmol/l; Fig. 3a, b). Finally, CART reduced glucagon secretion by 30 ± 11% (n = 4 donors) at 1 mmol/l glucose, but was without effect at a non-stimulatory glucose concentration (8.3 mmol/l; Fig. 3c). Thus, CART increased insulin secretion and inhibited glucagon secretion in human islets in a glucose-dependent fashion.
CART increases insulin secretion, improves glucose elimination, and inhibits glucagon secretion in vivo in mice and in vitro in humans. (a) CART (100 nmol/l) enhances insulin secretion in human islets (n = 19) at 16.7 mmol/l glucose. (b) A similar effect is seen in islets from diabetic donors (n = 7). (c) CART (100 nmol/l) reduces glucagon secretion at 1 mmol/l glucose. (d–g) Intravenous injection of CART (150 nmol/kg) provokes a twofold increase in first-phase insulin secretion (d), enhances AIR (e), lowers plasma glucose (f) and improves KG (g) during an IVGTT in mice (n = 16). (h) CART raises AIR to a similar extent as GLP-1 (4 nmol/kg) and when CART is given together with GLP-1, AIR is further increased (n = 16). (i) Injection of CART (150 nmol/kg) reduces glucagon secretion after 2 min in fasted mice (n = 8), compared with controls (n = 7). Black bars/squares, CART; white bars/squares, NaCl. *p < 0.05 and ***p < 0.001. C, control
CART stimulates insulin secretion, reduces glucagon secretion and improves glucose elimination in vivo in mice
To examine the effect of exogenous CART on whole-body glucose homeostasis, CART (150 nmol/kg) was given together with glucose (0.75 g/kg) during IVGTT in mice (n = 16). CART provoked a twofold increase in first-phase insulin secretion (AIR 783 ± 99 vs 365 ± 26 pmol/l in controls; p < 0.001; Fig. 3d, e) and improved KG (CART treated: 4.0 ± 0.2%/min; controls: 3.2 ± 0.2%/min; p < 0.05; Fig. 3f, g). Next, we tested the effect of CART on GLP-1-stimulated GSIS. CART alone provoked a similar response in insulin secretion to that of GLP-1 (AIR 2140 ± 382 vs 2349 ± 365 pmol/l; p = 0.28). Notably, CART caused a further 30% increase in insulin secretion above that achieved by GLP-1 alone (AIR 2871 ± 522 vs 2349 ± 365 pmol/l, p < 0.02) (n = 16; Fig. 3h). To test if CART affects glucagon secretion, fasted mice were given i.v. CART, 150 nmol/kg. This provoked a 40% reduction in glucagon secretion after 2 min (n = 8; p < 0.001) compared with controls (n = 7; Fig. 3i). In summary, CART increased both GSIS and GLP-1-stimulated GSIS, reduced glucagon secretion and enhanced glucose elimination in mice.
CART increases insulin and inhibits glucagon secretion in vitro in mice
Next, we explored the effect of CART on insulin secretion stimulated with secretagogues other than glucose, as well as the effect on glucagon secretion in static incubations of isolated mouse islets. Similar to the findings in human islets, CART (10 nmol/l) increased GSIS at 16.7 (1.7-fold, p < 0.004, Fig. 4a), but not at 2.8 or 8.3 mmol/l glucose. CART had no effect on insulin secretion induced by 10 mmol/l α-ketoisocaproic acid (α-KIC; an activator of mitochondrial metabolism), 100 μmol/l carbachol, or 35 mmol/l K+ at 11.1 (Fig. 4b) or 16.7 mmol/l glucose (data not shown). In keeping with the in vivo data, CART increased (30%, p < 0.05) GLP-1-stimulated (100 nmol/l) GSIS (Fig. 4c). To test the effect of long-term exposure to CART, as evident in type 2 diabetic patients and diabetic mice, islets were pre-incubated with 100 nmol/l CART for 24 h before the insulin secretion assay. This provoked increased GSIS at 16.7 (40%, p < 0.05), but not at 2.8 mmol/l glucose (Fig. 4d). Finally, CART (10 nmol/l) reduced glucagon secretion at 2.8 (−26%, p < 0.05), 5.5 (−36%, p < 0.05) and 11.1 mmol/l glucose (−50%, p < 0.001) (Fig. 4e). Thus, CART increased glucose- and GLP-1-stimulated insulin secretion and reduced glucagon secretion in mouse islets.
CART enhances insulin secretion and exocytosis and reduces glucagon secretion and exocytosis in vitro in mice. (a–e) Insulin and glucagon secretion in mouse islets. CART (10 nmol/l) increases insulin secretion at 16.7 mmol/l glucose (a). CART has no effect on insulin secretion stimulated with K+ (35 mmol/l), carbachol (100 μmol/l) or α-KIC (10 mmol/l) (b), but CART increases GLP-1-enhanced (100 nmol/l) insulin secretion (c). (d) 24 h pre-treatment with CART (100 nmol/l) enhances insulin secretion at 16.7 mmol/l glucose. (e) CART (10 nmol/l) reduces glucagon secretion at 2.8, 5.5 and 11.1 mmol/l glucose. Data from five to eight experiments, eight technical replicates in each. (f–l) Effects of CART on single cell exocytosis in mouse islet cells. Exocytosis was evoked by trains of ten depolarisations (V), each lasting 500 ms, and monitored as increases in cell capacitance (ΔC) in control beta cells (n = 15) (f), beta cells treated with 10 nmol/l CART for 1 h (n = 12) (g), and beta cells treated with CART for 24 h (n = 5) (h). Control alpha cells (n = 6) (j) and alpha cells treated with CART (n = 8) for 1 h (k). Representative cell recordings are shown. Average total increase in capacitance evoked by the trains (ΔCTOT) in (i) beta cells and (l) alpha cells. n = number of patched cells, data from two to six independent experiments and animals. *p < 0.05, **p < 0.01 and ***p < 0.001. C, control
CART enhances exocytosis of insulin and reduces exocytosis of glucagon in vitro in mice
To assess the effect of CART on exocytosis at the single cell level in beta and alpha cells, we used patch clamp in intact mouse islets. In control beta cells, the capacitance increase (ΔCtot) induced by a train of depolarisations amounted to 139 ± 23 fF. Beta cells treated with CART (10 nmol/l, 1 h) showed a slight, but non-significant, increase in exocytosis (Fig. 4f-i). When pre-treated for 24 h, insulin exocytosis increased twofold compared with controls (287 ± 102 fF, p < 0.05) (Fig. 4f-i). Control alpha cells responded with a capacitance increase of 338 ± 98 fF. Already after 1 h treatment, 10 nmol/l CART robustly reduced glucagon exocytotic capacity by 62% to 130 ± 22 fF (p < 0.05) (Fig. 4j-l).
CART alters the [Ca2+]i signalling pattern in intact mouse islets
We next measured changes in [Ca2+]i in intact mouse islets and dispersed islet cells loaded with Fura-2 LR. CART had no effect on slow (∼0.2/min) [Ca2+]i oscillations induced by 16.7 mmol/l glucose (n = 10, not shown). However, islets often respond to glucose with fast (period ∼20 s) [Ca2+]i oscillations that are sometimes superimposed on the slow ones. The probability of evoking the fast pattern is increased under conditions of elevated cAMP [33, 34]. Accordingly, islets stimulated by 16.7 mmol/l glucose and 2.5 μmol/l forskolin almost invariably responded with fast or mixed fast and slow [Ca2+]i oscillations. The average period of the fast oscillations was 19 ± 5 s (n = 388 oscillations from five experiments). Under these conditions, 100 nmol/l CART consistently transformed the [Ca2+]i response into large-amplitude slow oscillations without a fast component (period 176 ± 19 s, n = 43 oscillations from five experiments; p < 0.001 vs the fast pattern; Fig. 5a). A weaker effect was sometimes seen with 10 nmol/l CART (ESM Fig. 5). Interestingly, the CART-induced change in [Ca2+]i oscillations was associated with improved synchronisation of different regions within the islet (n = 5; Fig. 5b-d, ESM Fig. 5). Notably, CART had no effect on [Ca2+]i oscillations in dispersed islet cells (data not shown). Thus, our data show that CART promoted slow [Ca2+]i oscillations and improved synchronisation of [Ca2+]i signalling, known to influence the kinetics of insulin secretion [35].
CART modulates the cytoplasmic Ca2+ signalling pattern in mouse islets. Effects of CART on [Ca2+]i recorded from an individual mouse islet during elevation of the glucose concentration from 3 to 16.7 mmol/l, followed by stimulation with 2.5 μmol/l forskolin. (a) [Ca2+]i response pattern recorded from the entire islet (top panel, black trace) and from indicated smaller ROIs (lower panel, coloured traces). CART transforms fast [Ca2+]i oscillations into slow ones. (b) Time-expanded segments from recording shown in (a). Arrows indicate time points used for construction of correlation matrices. (c) Correlation of [Ca2+]i responses in different islet subregions at the time points indicated in (b). These time points are selected to show correlation before (I) and after (II) addition of CART and after washout (III) and reintroduction (IV) of CART. Correlation matrices show colour-coded Pearson’s r coefficients for each possible ROI pair. CART improves the synchronisation between different islet subregions. (d) Connectivity maps highlighting the ROI pairs with correlation coefficients exceeding 0.8
Discussion
Agents that stimulate insulin secretion and reduce glucagon secretion are attractive in the search for new treatments for type 2 diabetes. Here, we provide evidence for CART being a novel human islet peptide, which holds promise for use as diabetes therapy. This is based on our data showing that CART inhibits glucagon secretion and stimulates insulin secretion, even on top of GLP-1.
Importantly, CART increased insulin secretion in islets from type 2 diabetic patients, a finding that gains support from previous observations in GK rat islets [12]. Furthermore, similar to incretins, the stimulatory effect of CART on insulin secretion was glucose dependent. Notably, and in agreement with our previous in vitro data [12], CART augmented GLP-1-stimulated GSIS even further. This, together with the fact that Cart −/− mice have diminished insulin secretion, suggests that CART is a physiologically important regulator of insulin secretion. Acute CART stimulation was not associated with alterations of beta cell [Ca2+]i level. However, CART promoted a change in the pattern of [Ca2+]i oscillations, with fast oscillations being replaced by slow ones, known to underlie the pulsatile release of insulin [33, 36]. Furthermore, the change in [Ca2+]i oscillation pattern was paralleled by improved synchronisation of the [Ca2+]i signal between different islet subregions. Synchronisation of beta cells is critical for normal insulin secretion kinetics [35] but it is not known how it is modulated by CART. The exact mechanism underlying CART amplification of insulin secretion remains to be established. We suggest that the short-term stimulatory action of CART on glucose-induced secretion may be related to its effect on the islet [Ca2+]i signalling pattern. This would explain why CART lacks effect when glucose is combined with high K+ or carbachol, known to induce pronounced, non-oscillatory islet [Ca2+]i increases [37, 38].
A factor complicating the mechanistic studies is that the CART receptor remains unknown [7, 39]. The majority of the effects of CART on islets were rapid, and evident within 1 h, however 24 h stimulation with CART was needed to increase exocytosis from single voltage-clamped beta cells. Whether this effect was secondary to transcriptional effects of CART, as reported previously [40], is not known.
We also showed that CART is an inhibitor of glucagon secretion in vivo in mice, in human islets and in mouse islets via a direct effect on the alpha cell. Of note, insulin [41], somatostatin [42] and GLP-1 [31] are the only hormones reported so far to have such a direct effect. In human islets the glucagon-lowering effect of CART was glucose dependent and only evident at stimulatory glucose levels. Together with the insulinotropic actions and protective effects against beta cell death [18], this positions CART as a plausible target for diabetes therapy.
Furthermore, CART was found to be a novel constituent of human beta and alpha cells. It is of notice that there are large species differences in islet CART expression. Thus, in rats CART is mainly expressed in delta cells [11, 12], whereas in mice CART is expressed in a small subpopulation of beta cells. Pigs have no CART expression in islet cells [16]. Notably, individuals with type 2 diabetes, as well as four different rodent models of diabetes, had increased islet CART expression. Our data suggest that beta cell CART is upregulated as a response to hyperglycaemia as the upregulation of CART in rat models of type 2 diabetes was prevented by glucose-normalising insulin therapy and Cart mRNA expression was enhanced in rat islets cultured at high glucose. Our data also show that islet CART expression is dynamic, which is supported by the fact that CART is transiently upregulated in rodent islets during development [13].
In view of the insulinotropic and glucagon-lowering effects of CART, the upregulation of CART in type 2 diabetic islets is most likely a homeostatic compensatory response trying to overcome hyperglycaemia via paracrine actions. Even though CART has been localised to beta and delta cell secretory granules [12], it is not known if islet CART contributes to circulating levels or if these are altered by type 2 diabetes.
The present study expands previous knowledge obtained in vitro in rodents and shows that CART affects islet hormone secretion in human islets and in vivo in mice. We conclude that CART is an important regulator of glucose homeostasis and, based on its properties of stimulating insulin secretion and inhibiting glucagon secretion, CART is a peptide that should be explored as a potential future therapy for diabetes.
Abbreviations
- [Ca2+]i :
-
Cytoplasmic Ca2+ concentration
- ΔCtot :
-
Capacitance increase
- AIR:
-
Acute insulin response
- CART:
-
Cocaine- and amphetamine-regulated transcript
- DEX:
-
Dexamethasone
- GSIS:
-
Glucose-stimulated insulin secretion
- ICC:
-
Immunocytochemistry
- ISH:
-
In situ hybridisation
- KG :
-
Glucose tolerance index
References
Ahrén B (2011) The future of incretin-based therapy: novel avenues—novel targets. Diabetes Obes Metab 13(Suppl 1):158–166
Gromada J, Franklin I, Wollheim CB (2007) Alpha-cells of the endocrine pancreas: 35 years of research but the enigma remains. Endocr Rev 28:84–116
D’Alessio D (2011) The role of dysregulated glucagon secretion in type 2 diabetes. Diabetes Obes Metab 13(Suppl 1):126–132
Groop L, Lyssenko V (2009) Genetic basis of beta-cell dysfunction in man. Diabetes Obes Metab 11(Suppl 4):149–158
Ahrén B, Wierup N, Sundler F (2006) Neuropeptides and the regulation of islet function. Diabetes 55:S98–S107
Douglass J, McKinzie AA, Couceyro P (1995) PCR differential display identifies a rat brain mRNA that is transcriptionally regulated by cocaine and amphetamine. J Neurosci 15:2471–2481
Rogge G, Jones D, Hubert GW, Lin Y, Kuhar MJ (2008) CART peptides: regulators of body weight, reward and other functions. Nat Rev Neurosci 9:747–758
Kristensen P, Judge ME, Thim L et al (1998) Hypothalamic CART is a new anorectic peptide regulated by leptin. Nature 393:72–76
Lambert PD, Couceyro PR, McGirr KM, Dall Vechia SE, Smith Y, Kuhar MJ (1998) CART peptides in the central control of feeding and interactions with neuropeptide Y. Synapse 29:293–298
Elefteriou F, Ahn JD, Takeda S et al (2005) Leptin regulation of bone resorption by the sympathetic nervous system and CART. Nature 434:514–520
Jensen PB, Kristensen P, Clausen JT et al (1999) The hypothalamic satiety peptide CART is expressed in anorectic and non-anorectic pancreatic islet tumors and in the normal islet of Langerhans. FEBS Lett 447:139–143
Wierup N, Björkqvist M, Kuhar MJ, Mulder H, Sundler F (2006) CART regulates islet hormone secretion and is expressed in the beta-cells of type 2 diabetic rats. Diabetes 55:305–311
Wierup N, Kuhar M, Nilsson BO, Mulder H, Ekblad E, Sundler F (2004) Cocaine- and amphetamine-regulated transcript (CART) is expressed in several islet cell types during rat development. J Histochem Cytochem 52:169–177
Wierup N, Sundler F (2006) CART is a novel islet regulatory peptide. Peptides 27:2031–2036
Wierup N, Richards WG, Bannon AW, Kuhar MJ, Ahren B, Sundler F (2005) CART knock out mice have impaired insulin secretion and glucose intolerance, altered beta cell morphology and increased body weight. Regul Pept 129:203–211
Wierup N, Gunnarsdottir A, Ekblad E, Sundler F (2007) Characterisation of CART-containing neurons and cells in the porcine pancreas, gastro-intestinal tract, adrenal and thyroid glands. BMC Neurosci 8:51
Arciszewski MB, Calka J, Majewski M (2008) Cocaine- and amphetamine-regulated transcript (CART) is expressed in the ovine pancreas. Ann Anat 190:292–299
Sathanoori R, Olde B, Erlinge D, Göransson O, Wierup N (2013) Cocaine- and amphetamine-regulated transcript (CART) protects beta cells against glucotoxicity and increases cell proliferation. J Biol Chem 288:3208–3218
Asnicar MA, Smith DP, Yang DD et al (2001) Absence of cocaine- and amphetamine-regulated transcript results in obesity in mice fed a high caloric diet. Endocrinology 142:4394–4400
del Giudice EM, Santoro N, Cirillo G, D’Urso L, Di Toro R, Perrone L (2001) Mutational screening of the CART gene in obese children: identifying a mutation (Leu34Phe) associated with reduced resting energy expenditure and cosegregating with obesity phenotype in a large family. Diabetes 50:2157–2160
Guerardel A, Barat-Houari M, Vasseur F et al (2005) Analysis of sequence variability in the CART gene in relation to obesity in a Caucasian population. BMC Genet 6:19
Wierup N, Svensson H, Mulder H, Sundler F (2002) The ghrelin cell: a novel developmentally regulated islet cell in the human pancreas. Regul Pept 107:63–69
Landerholm K, Shcherbina L, Falkmer SE, Järhult J, Wierup N (2012) Expression of cocaine- and amphetamine-regulated transcript is associated with worse survival in small bowel carcinoid tumors. Clin Cancer Res 18:3668–3676
Landerholm K, Falkmer SE, Järhult J, Sundler F, Wierup N (2011) Cocaine- and amphetamine-regulated transcript in neuroendocrine tumors. Neuroendocrinology 94:228–236
Mulder H, Lindh AC, Sundler F (1993) Islet amyloid polypeptide gene expression in the endocrine pancreas of the rat: a combined in situ hybridization and immunocytochemical study. Cell Tissue Res 274:467–474
Vicentic A, Dominguez G, Hunter RG, Philpot K, Wilson M, Kuhar MJ (2004) Cocaine- and amphetamine-regulated transcript peptide levels in blood exhibit a diurnal rhythm: regulation by glucocorticoids. Endocrinology 145:4119–4124
Myrsen U, Ahrén B, Sundler F (1995) Neuropeptide Y is expressed in subpopulations of insulin- and non-insulin-producing islet cells in the rat after dexamethasone treatment: a combined immunocytochemical and in situ hybridisation study. Regul Pept 60:19–31
Hagenfeldt-Johansson KA, Herrera PL, Wang H, Gjinovci A, Ishihara H, Wollheim CB (2001) Beta-cell-targeted expression of a dominant-negative hepatocyte nuclear factor-1 alpha induces a maturity-onset diabetes of the young (MODY)3-like phenotype in transgenic mice. Endocrinology 142:5311–5320
Ahrén J, Ahrén B, Wierup N (2010) Increased beta-cell volume in mice fed a high-fat diet: a dynamic study over 12 months. Islets 2:353–356
Rosengren AH, Jokubka R, Tojjar D et al (2010) Overexpression of alpha2A-adrenergic receptors contributes to type 2 diabetes. Science 327:217–220
De Marinis YZ, Salehi A, Ward CE et al (2010) GLP-1 inhibits and adrenaline stimulates glucagon release by differential modulation of N- and L-type Ca2+ channel-dependent exocytosis. Cell Metab 11:543–553
Dyachok O, Gylfe E (2004) Ca(2+)-induced Ca(2+) release via inositol 1,4,5-trisphosphate receptors is amplified by protein kinase A and triggers exocytosis in pancreatic beta-cells. J Biol Chem 279:45455–45461
Bergsten P, Grapengiesser E, Gylfe E, Tengholm A, Hellman B (1994) Synchronous oscillations of cytoplasmic Ca2+ and insulin release in glucose-stimulated pancreatic islets. J Biol Chem 269:8749–8753
Liu YJ, Tengholm A, Grapengiesser E, Hellman B, Gylfe E (1998) Origin of slow and fast oscillations of Ca2+ in mouse pancreatic islets. J Physiol 508:471–481
Tengholm A, Gylfe E (2009) Oscillatory control of insulin secretion. Mol Cell Endocrinol 297:58–72
Gilon P, Shepherd RM, Henquin JC (1993) Oscillations of secretion driven by oscillations of cytoplasmic Ca2+ as evidences in single pancreatic islets. J Biol Chem 268:22265–22268
Gilon P, Henquin JC (1992) Influence of membrane potential changes on cytoplasmic Ca2+ concentration in an electrically excitable cell, the insulin-secreting pancreatic B cell. J Biol Chem 267:20713–20720
Gilon P, Nenquin M, Henquin JC (1995) Muscarinic stimulation exerts both stimulatory and inhibitory effects on the concentration of cytoplasmic Ca2+ in the electrically excitable pancreatic B cell. Biochem J 311:259–267
Vicentic A, Lakatos A, Jones D (2006) The CART receptors: background and recent advances. Peptides 27:1934–1937
Lv L, Jimenez-Krassel F, Sen A et al (2009) Evidence supporting a role for cocaine- and amphetamine-regulated transcript (CARTPT) in control of granulosa cell estradiol production associated with dominant follicle selection in cattle. Biol Reprod 81:580–586
Franklin I, Gromada J, Gjinovci A, Theander S, Wollheim CB (2005) Beta-cell secretory products activate alpha-cell ATP-dependent potassium channels to inhibit glucagon release. Diabetes 54:1808–1815
Schuit FC, Derde MP, Pipeleers DG (1989) Sensitivity of rat pancreatic A and B cells to somatostatin. Diabetologia 32:207–212
Acknowledgements
We thank D. Persson, B.-M. Nilsson, L. Bengtsson, L. Kvist, A.-H. Thorén-Fischer, U. Voss, L. Wallgren, and A. Östlund at Lund University, Sweden for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by grants from the Swedish Research Council (Project grants: 521-2012-2119, 522-2008-4216, K2009-55X 21111-01-4 (NW), 521-2010-3490 (LG), 325-2012-6778 (AT), 6834 (BA), Linneaeus grant to Lund University Diabetes Centre 349-2006-237, Strategic Research Area grant EXODIAB 2009-1039), from Novo Nordisk Foundation, European Foundation For the Study of Diabetes/Merck Sharp & Dohme, Royal Physiographic Society in Lund, Faculty of Medicine at Lund University, Region Skåne, Crafoord Foundation, Gyllenstiernska Krapperup, Tore Nilsson, Åke Wiberg, Lars Hierta, Fredrik and Ingrid Thuring, Magnus Bergwall, Albert Påhlsson, Knut & Alice Wallenberg foundation (KAW 2009.0243), Swedish Diabetes Foundation, Family Ernfors Fund, Heart and Lung Foundation and Åhlén Foundation. MJK: RR00165, DA15162, and DA15040. LG: ERC Advanced Researcher grant GENETARGET-T2D (GA-269045), Sigrid Juselius Foundation, Folkhälsan Research, Finnish Diabetes Research Foundation.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
Each author: (1) contributed substantially to the conception and design, acquisition of data and/or analysis and interpretation of data; (2) drafted the article and/or revised it critically for important intellectual content; and (3) gave final approval of the version to be published. NW is guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Figs
(PDF 1392 kb)
Rights and permissions
About this article
Cite this article
Abels, M., Riva, M., Bennet, H. et al. CART is overexpressed in human type 2 diabetic islets and inhibits glucagon secretion and increases insulin secretion. Diabetologia 59, 1928–1937 (2016). https://doi.org/10.1007/s00125-016-4020-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-016-4020-6