Abstract
Aims/hypothesis
Coronary flow reserve (CFR) and coronary artery calcium (CAC) represent functional and structural aspects of atherosclerosis. We examined the prevalence of reduced CFR and high CAC scores in three predefined groups of participants without known cardiovascular disease: (1) patients with type 2 diabetes and albuminuria; (2) patients with type 2 diabetes and normoalbuminuria; and (3) non-diabetic controls.
Methods
In a cross-sectional design, cardiac 82Rb positron emission tomography/computed tomography was conducted in 60 patients with type 2 diabetes who were free of overt cardiovascular disease and who were stratified by normoalbuminuria (<30 mg/24 h) (n = 30; age [mean ± SD] 60.9 ± 10.1 years) and albuminuria (≥30 mg/24 h) (n = 30; age 65.6 ± 4.8 years), and in 30 healthy, non-diabetic controls (age 59.8 ± 9.9 years).
Results
In controls, normoalbuminuric and albuminuric patients, CFR was 3.0 ± 0.8, 2.6 ± 0.8 and 2.0 ± 0.5, respectively. Reduced CFR (<2.5) was observed in 16.7%, 40.0% and 83.3% of participants, respectively, and median (interquartile range) CAC scores were 0 (0–81), 36 (1–325) and 370 (152–1,025), respectively (p for trend <0.01). After adjustment, the difference in CFR and CAC between albuminuric patients and controls remained significant (p ≤ 0.001). There were trends towards lower CFR and higher CAC scores in normoalbuminuric patients vs controls (p ≤ 0.023) and towards higher CAC scores in albuminuric vs normoalbuminuric patients (p = 0.026). In multivariate regression analysis, a higher urinary albumin excretion rate (UAER) tended to predict reduced CFR in the total population (p = 0.045). When the CAC score was added, there was also a trend (p = 0.032) towards an inverse association with reduced CFR.
Conclusions/interpretation
Type 2 diabetic patients who were free of overt cardiovascular disease had a high prevalence of coronary microvascular dysfunction, especially with concomitant albuminuria, suggesting a common microvascular impairment occurring in multiple microvascular beds. Prospective studies are needed to show the prognostic significance of this finding.
Similar content being viewed by others
Introduction
Type 2 diabetes is commonly associated with the early development of coronary artery disease (CAD) [1]. For diabetic patients with concomitant albuminuria, the risk of cardiovascular disease is further pronounced [2]. More research is needed to define potential subsets of patients with diabetes who might benefit from additional testing for asymptomatic CAD.
Abnormalities of the coronary circulatory function are well documented to occur before and to accelerate during the development of CAD in patients with diabetes [3]. However, these changes in coronary circulatory function, as well as mild structural variations in the arterial wall, might begin early as subclinical forms, while it presumably takes substantially more time for the clinical appearance of advanced stages of CAD [4].
Definitions of clinically significant CAD vary substantially, based on whether anatomical or functional criteria are used. It is important to note that the agreement between anatomical (e.g. degree of coronary stenosis) and functional (e.g. myocardial perfusion) criteria is often poor [5].
Quantitative cardiac positron emission tomography (PET) is a new and innovative method with which to detect patients with subclinical CAD. One of the major advantages of cardiac PET is that, uniquely, it can measure absolute myocardial blood flow (in ml/min/g of tissue) at rest and during pharmacologically induced hyperaemic conditions, from which a ratio can be calculated (termed the coronary flow reserve [CFR]) as an adjunct to the visual interpretation of myocardial perfusion [6].
CFR is an important physiological variable in the coronary circulation that reflects the function of large epicardial arteries and the microcirculation. Thus, reduced CFR can be caused by both stenosis in the epicardial coronary arteries and coronary microvascular dysfunction. In individuals without epicardial coronary stenosis, cardiac PET can assess the function of the microcirculation, including the combined function of cells in the vascular smooth muscle and the endothelial cells. Among individuals without indications of CAD, microvascular dysfunction is associated with cardiovascular risk factors, including hypercholesterolaemia, diabetes, hypertension and smoking [7]. Moreover, it is a predictor of cardiac mortality [8]. Most patients with type 2 diabetes have associated hypertension, dyslipidaemia and obesity, all of which can contribute to coronary microvascular damage.
In addition, a computed tomography (CT) scan can be used to estimate coronary artery calcium (CAC), and this imaging modality can be usefully combined with quantitative cardiac PET in a hybrid scanner. CAC is known to be highly correlated with the extent of coronary atherosclerosis, and can identify asymptomatic patients who are at higher risk for inducible ischaemia and mortality [9, 10]. The presence of calcium in the coronary arteries is a specific marker of atherosclerosis, independent of its aetiology.
We undertook a cross-sectional study of type 2 diabetic patients with or without albuminuria and age- and sex-matched healthy controls without known manifest cardiovascular disease. The aims were twofold. First, to examine the prevalence of impaired CFR and elevated CAC in the three predefined groups of participants without known cardiovascular disease: (1) patients with type 2 diabetes and albuminuria; (2) patients with type 2 diabetes and normoalbuminuria; and (3) healthy controls. And second, to determine predictors of impaired CFR and elevated CAC in the total population.
The prespecified study hypotheses were that: (1) patients with type 2 diabetes and albuminuria have an impaired coronary microcirculation (assessed using the CFR) and increased coronary calcification (assessed using CAC) when compared with normoalbuminuric patients; and (2) patients with type 2 diabetes and normoalbuminuria have impaired CFR and increased CAC when compared with healthy controls.
Methods
Study population
A cohort of 60 consecutive outpatients with type 2 diabetes, defined according to the WHO criteria, was identified at Steno Diabetes Center. Participants were aged between 35 and 80 years, and had the ability to understand and give informed consent. Patients were stratified as normoalbuminuric if the urinary albumin excretion rate (UAER) was <30 mg/24 h in two of three consecutive urine collections (two of the samples were collected over 24 h in relation to the present study). A priori, we decided to include 30 patients with normoalbuminuria and 30 with persistent elevated albuminuria (UAER ≥30 mg/24 h). In addition, 30 non-diabetic controls were recruited from a newspaper advertisement and matched for age and sex to the 30 patients with normoalbuminuria. Participants were excluded if one of the following characteristics were present: (1) history of CAD or other cardiovascular disease (including stroke) or heart symptoms, assessed from patient files and thorough interviews and questionnaires; (2) asthma or chronic obstructive pulmonary disease requiring treatment; (3) kidney disease other than diabetic nephropathy; (4) end-stage renal disease; (5) office BP >200/110 mmHg; (6) second- or third-degree atrioventricular block; or (7) pregnancy or lactating.
A power calculation was performed using the power statement implemented in the SAS software, version 9.3 (SAS Institute, Cary, NC, USA). In the assumption of a mean difference in CFR of 0.6 and an SD of 0.8, at least 27 participants in each group were needed to provide 80% power for a type I error of 5%. To account for technical difficulties and incomplete investigations, we included a total of 30 participants in each group.
The study was performed from April to December 2013 and was conducted in compliance with the Declaration of Helsinki. All participants gave informed written consent and the study protocol was approved by the local ethics committee.
Clinical measurements
Three office BPs were measured in the sitting position after 5–10 min rest, with an oscillometric device (A&D Medical, San Jose, CA, USA) using an appropriate cuff size and averaged. HbA1c was measured by HPLC and plasma creatinine by an enzymatic method (Hitachi 912, Roche Diagnostics, Mannheim, Germany). Estimated (e)GFR was calculated using the CKD-EPI equation [11].
Measurement of 24 h BP was conducted using BPro (HealthStats, Singapore), a watch-like device that captures radial pulse wave reflection with tonometry and calculates brachial 24 h BP from the pulse wave after calibration to brachial BP. The device meets standards from the European Society of Hypertension and the Association for the Advancement of Medical Instrumentation [12]. The device was programmed to capture BP every 15 min for 24 h. Mean systolic and diastolic BP were calculated using all readings over the 24 h.
UAER was measured in two 24 h urine collections by an enzyme immunoassay and calculated as the geometric mean of the two collections.
A detailed medical history was obtained along with demographic and anthropometric variables, including smoking status. Current smoking was defined as one or more cigarettes, cigars or pipes per day. Information on medical treatment was obtained from questionnaires and cross-checked against medical records at the Steno Diabetes Center. The weight and height of each participant were measured, and BMI was calculated as body weight (kg) divided by height (m2). A standard 12-lead resting ECG was obtained.
Hybrid cardiac PET/CT imaging
A dynamic, gated cardiac PET study was performed using a hybrid PET/CT scanner in 3D mode (Siemens Biograph mCT 128, Siemens, Munich, Germany) following the administration of 1,100 MBq 82Rb (CardioGen-82, Bracco Diagnostics, Monroe Township, NJ, USA). The myocardium was covered in a single bed position, with ECG gating (8 frames/RR cycle; total acquisition time 7 min). Low-dose CT was acquired for attenuation correction. Images were reconstructed into 16 images (12 × 10 s, 2 × 30 s, 1 × 60 s, 1 × 120 s) with attenuation, scatter and decay corrections using iterative 3D ordered subsets expectation–maximisation (two iterations; 24 subsets) and Gaussian filtering with 10 mm full width at half maximum. Semiquantitative data were processed using Cedars QPS/QGS software (version 2012, Cedars-Sinai, Los Angeles, CA, USA). Non-gated images were presented in the horizontal and vertical long axis and in the short axis, and displayed in a polar map format divided into 17 segments, as suggested by the American Heart Association [13], and normalised to peak myocardial activity (100%) [14]. Myocardial blood flow was calculated automatically using the Siemens Syngo MBF 2.3 (Siemens Medical Solutions, Malvern, PA, USA) with one-compartment tracer kinetic models for 82Rb, including regional uptake and clearance variables, blood to myocardium spill-over and partial volume corrections [15], and the extraction curve from Lortie et al [16]. Maximal hyperaemia was induced with adenosine infused at 140 μg kg−1 min−1 for 6 min. For semiquantitative assessment of myocardial perfusion abnormalities, 17-segment visual interpretation of gated myocardial perfusion images was performed by two experienced operators. Participants abstained from all caffeine- or methylxanthine-containing substances for at least 18 h prior to the cardiac PET scan.
CAC content was quantified using the method described by Agatston et al [17] and semiautomated commercially available software (Corridor4DM, INVIA, Ann Arbor, MI, USA). Coronary artery specific scores were calculated in the three main coronary arteries and then summed to provide a total CAC score for each participant.
Coronary microvascular dysfunction was defined as CFR <2.5, as suggested by Schindler et al [18]. Elevated CAC was a value >300, according to a previous study by Detrano et al [19].
Statistical analysis
The distribution of CAC was skewed and was therefore log-transformed (log2 [CAC +1]) in all analyses, as was UAER and known duration of diabetes. These variables are given as medians with interquartile range (IQR). All other continuous variables are given as means ± SD and the categorical variables are given as total numbers with corresponding percentages. When analysing differences between two groups (controls vs normoalbuminuric patients, and normoalbuminuric vs albuminuric patients) we used independent samples t test for continuous variables and χ 2 for categorical variables. ANCOVA was applied when comparing levels of CFR and CAC between the three groups.
We ascertained that the four principal assumptions of linear regression were fulfilled. The proportion of the variability in the dependent variable explained by the model is presented as R 2. Because of the use of repeated independent t tests increasing the probability of a type I error, results were considered to be significant at a two-tailed p < 0.01, and p < 0.05 to p = 0.01 as trend. Statistical analyses were performed using SAS software (version 9.3; SAS Institute).
Rationale for selection of covariates
Because there was a modest number of participants in each group, only a limited sum of covariates could be included due to the risk of overfitting. Therefore, we included traditional cardiovascular risk factors based on prior evidence in the multivariate analysis. Owing to bias by indication, we did not include variables for medical treatment. Moreover, total cholesterol was not included because patients had lower levels than controls, likely due to lipid-lowering treatment. In the analysis comparing levels of CFR and CAC between the groups, HbA1c and UAER were not included, since the groups were precategorised based on these variables. Thus, the final adjustment for the group comparisons consisted of sex, age, 24 h systolic BP, eGFR and smoking.
For the multivariate linear regression models for predictors of reduced CFR and increased CAC, we applied the enter method. This approach was chosen because we did not know which independent variables would be significantly correlated to the outcome variables (i.e. CFR and CAC). The model included sex, age, 24 h systolic BP, eGFR, smoking, HbA1c and UAER.
To determine the robustness of the findings for the differences between groups, we additionally performed a multivariate analysis including variables showing statistically significant (p < 0.05) correlations in the sample; again excluding total cholesterol and medical treatment. This model included age, BMI, eGFR and heart rate. This approach can, however, result in biased estimates of effect [20].
Results
Clinical characteristics
The total cohort (n = 90) comprised 64.4% men and the mean ± SD age was 62.1 ± 9.2 years. The characteristics of the participants in the three groups are shown in Table 1. The normoalbuminuric patient group had a higher mean BMI and heart rate than controls, a higher frequency of antihypertensive or lipid-lowering treatment and lower total cholesterol (p ≤ 0.001). Patients with albuminuria had a lower eGFR than normoalbuminuric patients (p < 0.001). There were no intergroup differences in the proportion of men, 24 h BP or the prevalence of smoking (p ≥ 0.067). Patients with microalbuminuria (UAER 30–299 mg/24 h; n = 23) and macroalbuminuria (UAER >300 mg/24 h; n = 7) did not differ in any of the examined characteristics (p > 0.40), except for a trend towards lower eGFR in those with macroalbuminuria (p = 0.037).
All patients were treated with dietary modifications and oral glucose-lowering medication, and 48% also received insulin. Moreover, most patients received lipid-lowering therapy (93%), aspirin (88%) and renin–angiotensin–aldosterone system blocking treatment (90%).
Cardiac PET/CT scanning
Results from the cardiac PET/CT scanning are summarised in Table 2. There was a trend towards lower CFR and higher CAC in patients with normoalbuminuria compared with controls (p ≤ 0.045). CFR was significantly lower and CAC significantly higher in patients with albuminuria compared with normoalbuminuric patients (p ≤ 0.002). In trend tests across the three groups, CFR significantly decreased and CAC significantly increased (p < 0.001). There was a trend towards a higher frequency of reduced CFR (<2.5) in normoalbuminuric patients compared with controls (p = 0.045). The frequency of reduced CFR was significantly (p < 0.001) higher in patients with albuminuria compared with normoalbuminuric patients, and there was a trend (p = 0.035) towards a higher frequency of elevated CAC (>300).
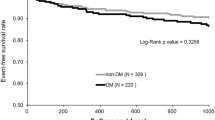
After adjustment for sex, age, 24 h systolic BP, eGFR and smoking, the difference in CFR and CAC between albuminuric patients and controls remained significant (p ≤ 0.001). There was a trend towards lower CFR and higher CAC in normoalbuminuric patients vs controls (p ≤ 0.023), and towards higher CAC in albuminuric vs normoalbuminuric patients (p = 0.026; Fig. 1).
Left ventricle ejection fraction (LVEF) was within the normal range (>50%) both during rest and stress conditions in all groups, with no intergroup difference (p ≥ 0.42; Table 2). The LVEF increased (mean ± SD: 6.0 ± 4.7) during stress conditions in all except five participants.
Reversible ischaemia was observed in 12 participants (13%; one control, seven normoalbuminuric patients and four albuminuric patients), with a median (range) extent of 7.5% (2–23%). Three patients had fixed perfusion defects, two of whom had fixed defects with partial reversibility.
Variables correlated with CFR and CAC
In the total population, CFR was significantly negatively correlated with CAC (R 2 = 0.24; p < 0.001) and UAER (R 2 = 0.20; p < 0.001), and positively correlated with eGFR (R 2 = 0.11; p = 0.001) (Fig. 2). Moreover, there was a tendency towards a negative correlation between CAC and eGFR (R 2 = 0.08; p = 0.034) and a significant positive correlation between CAC and UAER (R 2 = 0.21; p < 0.001).
Predictors of reduced CFR in adjusted analyses
In multivariate linear regression (model R 2 = 0.32), higher UAER tended to be a predictor of reduced CFR in the total population (p = 0.045). When CAC was added (model R 2 = 0.36), there was also a trend (p = 0.032) towards an inverse association with reduced CFR.
Predictors of increased CAC in adjusted analyses
In multivariate linear regression (model R 2 = 0.47), the predictors of an increased CAC in the total population were older age (p < 0.001) and higher HbA1c (p = 0.004), and a tendency for higher UAER (p = 0.046) and male sex (p = 0.015). When CFR was added (model R 2 = 0.50), there was also a trend (p = 0.032) towards an inverse association with elevated CAC.
Additional analyses
After adjustment for variables showing statistically significant correlations in the sample (i.e. age, BMI, eGFR and heart rate), the difference in CFR and CAC remained significant between albuminuric patients and controls (p ≤ 0.008) and between albuminuric and normoalbuminuric patients for CAC (p = 0.004). There was a trend towards a difference in CFR in normoalbuminuric patients vs controls (p = 0.039).
To avoid the potential confounding effect of epicardial stenosis on CFR, we performed a sensitivity analysis including only those participants without perfusion defects on semiquantitative analysis of the PET scan (n = 75). The results were confirmatory; CFR was 3.0 ± 0.8, 2.7 ± 0.7 and 2.1 ± 0.5 in controls, normoalbuminuric and albuminuric patients, respectively, and all intergroup differences were significant (p ≤ 0.024). Moreover, CFR was significantly negatively correlated with CAC (R 2 = 0.21; p < 0.001) and UAER (R 2 = 0.25; p < 0.001), and positively correlated with eGFR (R 2 = 0.13; p = 0.002).
Discussion
In asymptomatic patients with type 2 diabetes, impaired CFR and elevated CAC were demonstrable with 82Rb PET/CT, a new, fast and non-invasive hybrid imaging method for assessing these measures of vascular function and structure. The findings were further pronounced in patients with concomitant albuminuria. Our findings suggest that even in asymptomatic individuals, patients with type 2 diabetes and albuminuria, known to be at high risk of cardiovascular disease, have impaired coronary microcirculation when compared with normoalbuminuric patients. However, this was partly explained by other cardiovascular risk factors. Furthermore, asymptomatic normoalbuminuric type 2 diabetic patients showed a tendency towards impaired coronary microcirculation compared with age- and sex-matched controls, even after adjustment for cardiovascular risk factors.
Moreover, for CFR, we found a tendency towards a negative correlation with CAC and UAER. Older age and higher HbA1c were correlated with elevated CAC, and there was a tendency towards a correlation of higher UAER and male sex with elevated CAC.
Impaired CFR has previously been described as a powerful, independent correlate of cardiac mortality among patients with diabetes [8]. That study concluded that diabetic patients without known CAD and with impaired CFR experienced a rate of cardiac death comparable with that for non-diabetic patients with known CAD. Diabetic patients without known CAD and preserved CFR had very low annualised rate of cardiac mortality.
A CFR below 2.5 is considered reduced [18], and in our study 83% of patients with type 2 diabetes and albuminuria had impaired CFR according to this threshold, compared with 40% of normoalbuminuric patients. Previously, the degree of CFR restriction in diabetes has been associated with the magnitude of retinopathy [21] and with renal insufficiency [22]; altogether, suggestive of a common microvascular impairment occurring in multiple microvascular beds, which might be hypothesised to be part of the natural history of diabetic patients.
CAC is usually measured in asymptomatic patients with intermediate cardiovascular risk, and it has been consistently shown that a CAC level of 0 in this patient group is associated with a low risk of coronary events in 5–10 years [19]. A CAC level above 300, on the other hand, has been associated with an increased risk of cardiovascular events and mortality in both non-diabetic individuals and diabetic patients in 3–5 years of follow-up [9]. Furthermore, in a prospective study of 200 microalbuminuric patients with type 2 diabetes, we recently showed CAC to be the strongest predictor of cardiovascular events and mortality after 6 years of follow-up [23].
In the current study, we found that asymptomatic diabetic patients had higher CAC levels and a higher prevalence of increased CAC levels compared with healthy control participants. More than 50% of the albuminuria group had a CAC level above 300, indicative of a high risk of cardiovascular disease and mortality. Furthermore, both higher UAER and lower eGFR correlated with higher CAC. This could indicate that part of the increased cardiovascular risk in patients with impaired kidney function is mediated by metastatic calcification.
We found that CFR was negatively correlated with CAC. Recent cross-sectional studies have revealed a similar correlation between coronary microcirculation dysfunction and coronary artery calcification. Wang et al reported that CFR was negatively correlated with the presence and severity of CAC in a population of 222 individuals without known cardiovascular disease enrolled in a multiethnic study of atherosclerosis [24]. In contradiction to these findings, Pirich et al found no relationship between CAC and CFR in 22 asymptomatic individuals with a family history of premature CAD [25]. Curillova et al, however, documented a significant association between increasing CAC and declining CFR among patients suspected to have CAD [26]. Thus, although microvascular dysfunction is an important factor in the development of atherosclerosis, the association between functional and structural alterations in atherosclerosis might not be straightforward and might expose different pathophysiological processes and differences in time course.
This was also reflected in our population, where a CAC of 0 could not solely be used as a gatekeeper. In the 24 participants with a CAC of 0, the CFR range was 1.8–4.9, and three participants (3%) had coronary microvascular dysfunction (CFR <2.5).
Besides CFR and CAC, cardiac PET/CT imaging allows the identification of individuals with regional perfusion defects in the myocardium, induced by pharmacological stress. Interestingly, in our asymptomatic type 2 diabetic patients with a mean age of 63.2 ± 8.8 years, the prevalence of myocardial regional perfusion defects was only 20%. This suggests that advanced and flow-limiting damage to the vessels might require a longer period to develop than previously estimated. However, the low prevalence could be biased by the inclusion of only asymptomatic patients. It is likely that patients with a more rapid development of advanced lesions were excluded because of previous cardiovascular disease or symptoms.
Clinical implications
Cardiac PET imaging offers several advantages with regards to patient comfort, radiation safety and duration of image acquisition (<1 h, as compared with up to 2 days for classic cardiac single-photon emission CT). PET might be a promising imaging method to guide personalised care. However, every new technique must find its place in the clinical scenario through the demonstration of cost-effectiveness and superiority over established methodologies.
Because CFR provides a quantitative assessment of the integrated effects of epicardial coronary stenosis, diffuse atherosclerosis and microvascular dysfunction [27], its role as an early and sensitive marker of myocardial tissue perfusion impairment is promising. By adding the known prognostic value of both CAC and LVEF to CFR, cardiac PET/CT imaging might be a potential screening tool with which to identify asymptomatic patients with type 2 diabetes who are at high risk of cardiovascular disease and mortality. However, since this technique is cumbersome and costly, the added predictive value compared with other predictors should be proven in larger, prospective studies.
Strengths and limitations
The strength of this study is that, to our knowledge, it is the first to evaluate CFR in asymptomatic type 2 diabetic patients using the new, fast and non-invasive cardiac 82Rb PET/CT technique, while comparing these patients with healthy controls. Limitations of the study include the relatively small sample size and its cross-sectional nature. However, the findings were robust when applying two different statistical approaches for the multivariate models.
Prospective studies are needed to assess the relative impact on future cardiovascular events of the measures provided by cardiac 82Rb PET/CT imaging. Moreover, information on markers of inflammation and endothelial activation might have reinforced the concept that measuring CFR and CAC with the new technology works better than other approaches. In addition, evaluation of other parts of the vascular system (e.g. carotid arteries) would have strengthened our findings.
Conclusion
In asymptomatic patients with type 2 diabetes, we found a high prevalence of impaired CFR and elevated CAC, especially in patients with concomitant albuminuria, suggesting a common microvascular impairment occurring in multiple microvascular beds.
Abbreviations
- CAC:
-
Coronary artery calcium
- CAD:
-
Coronary artery disease
- CFR:
-
Coronary flow reserve
- CT:
-
Computed tomography
- eGFR:
-
Estimated GFR
- IQR:
-
Interquartile range
- LVEF:
-
Left ventricle ejection fraction
- PET:
-
Positron emission tomography
- UAER:
-
Urinary albumin excretion rate
References
Kannel WB, McGee DL (1979) Diabetes and glucose tolerance as risk factors for cardiovascular disease: the Framingham study. Diabetes Care 2:120–126
de Zeeuw D, Parving HH, Henning RH (2006) Microalbuminuria as an early marker for cardiovascular disease. J Am Soc Nephrol 17:2100–2105
Nahser PJ Jr, Brown RE, Oskarsson H, Winniford MD, Rossen JD (1995) Maximal coronary flow reserve and metabolic coronary vasodilation in patients with diabetes mellitus. Circulation 91:635–640
Zeiher AM, Drexler H, Wollschlager H, Just H (1991) Endothelial dysfunction of the coronary microvasculature is associated with coronary blood flow regulation in patients with early atherosclerosis. Circulation 84:1984–1992
Gaemperli O, Luscher TF, Bax JJ (2013) View point: what should the future design of clinical imaging studies be? Eur Heart J 34:2432–2435
Schindler TH, Quercioli A, Valenta I, Ambrosio G, Wahl RL, Dilsizian V (2014) Quantitative assessment of myocardial blood flow—clinical and research applications. Semin Nucl Med 44:274–293
Chade AR, Brosh D, Higano ST, Lennon RJ, Lerman LO, Lerman A (2006) Mild renal insufficiency is associated with reduced coronary flow in patients with non-obstructive coronary artery disease. Kidney Int 69:266–271
Murthy VL, Naya M, Foster CR et al (2012) Association between coronary vascular dysfunction and cardiac mortality in patients with and without diabetes mellitus. Circulation 126:1858–1868
Silverman MG, Blaha MJ, Krumholz HM et al (2014) Impact of coronary artery calcium on coronary heart disease events in individuals at the extremes of traditional risk factor burden: the Multi-Ethnic Study of Atherosclerosis. Eur Heart J 35:2232–2241
Raggi P, Shaw LJ, Berman DS, Callister TQ (2004) Prognostic value of coronary artery calcium screening in subjects with and without diabetes. J Am Coll Cardiol 43:1663–1669
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Theilade S, Joergensen C, Persson F, Lajer M, Rossing P (2012) Ambulatory tonometric blood pressure measurements in patients with diabetes. Diabetes Technol Ther 14:453–456
Cerqueira MD, Weissman NJ, Dilsizian V et al (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Int J Cardiovasc Imaging 18:539–542
Germano G, Kavanagh PB, Waechter P et al (2000) A new algorithm for the quantitation of myocardial perfusion SPECT. I: technical principles and reproducibility. J Nucl Med 41:712–719
DeKemp RA, Declerck J, Klein R et al (2013) Multisoftware reproducibility study of stress and rest myocardial blood flow assessed with 3D dynamic PET/CT and a 1-tissue-compartment model of 82Rb kinetics. J Nucl Med 54:571–577
Lortie M, Beanlands RS, Yoshinaga K, Klein R, Dasilva JN, DeKemp RA (2007) Quantification of myocardial blood flow with 82Rb dynamic PET imaging. Eur J Nucl Med Mol Imaging 34:1765–1774
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R (1990) Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 15:827–832
Schindler TH, Schelbert HR, Quercioli A, Dilsizian V (2010) Cardiac PET imaging for the detection and monitoring of coronary artery disease and microvascular health. JACC Cardiovasc Imaging 3:623–640
Detrano R, Guerci AD, Carr JJ et al (2008) Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 358:1336–1345
Groenwold RH, Klungel OH, Grobbee DE, Hoes AW (2011) Selection of confounding variables should not be based on observed associations with exposure. Eur J Epidemiol 26:589–593
Akasaka T, Yoshida K, Hozumi T et al (1997) Retinopathy identifies marked restriction of coronary flow reserve in patients with diabetes mellitus. J Am Coll Cardiol 30:935–941
Ragosta M, Samady H, Isaacs RB, Gimple LW, Sarembock IJ, Powers ER (2004) Coronary flow reserve abnormalities in patients with diabetes mellitus who have end-stage renal disease and normal epicardial coronary arteries. Am Heart J 147:1017–1023
von Scholten BJ, Reinhard H, Hansen TW et al (2015) Additive prognostic value of plasma N-terminal pro-brain natriuretic peptide and coronary artery calcification for cardiovascular events and mortality in asymptomatic patients with type 2 diabetes. Cardiovasc Diabetol 14:59
Wang L, Jerosch-Herold M, Jacobs DR Jr, Shahar E, Detrano R, Folsom AR (2006) Coronary artery calcification and myocardial perfusion in asymptomatic adults: the MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 48:1018–1026
Pirich C, Leber A, Knez A et al (2004) Relation of coronary vasoreactivity and coronary calcification in asymptomatic subjects with a family history of premature coronary artery disease. Eur J Nucl Med Mol Imaging 31:663–670
Curillova Z, Yaman BF, Dorbala S et al (2009) Quantitative relationship between coronary calcium content and coronary flow reserve as assessed by integrated PET/CT imaging. Eur J Nucl Med Mol Imaging 36:1603–1610
Gould KL (2009) Does coronary flow trump coronary anatomy? JACC Cardiovasc Imaging 2:1009–1023
Acknowledgements
We thank all participants and acknowledge the work of study nurse L. Jelstrup and laboratory technicians A. G. Lundgaard, B. R. Jensen, T. R. Juhl and J. A. Hermann (Steno Diabetes Center, Gentofte, Denmark).
Some of these data were presented as an abstract at the EASD and ARTERY meetings in 2014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Internal funding was provided by Steno Diabetes Center, Gentofte, Denmark, and Rigshospitalet, Copenhagen, Denmark.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
BJvS conceived and designed the research, acquired data, performed statistical analysis and drafted the manuscript. PH, AK and PR conceived and designed the research, acquired data, handled funding and supervision, and critically revised the manuscript for key intellectual content. TEC and AAG acquired data and critically revised the manuscript for key intellectual content. TWH conceived and designed the research, acquired data, performed statistical analysis and critically revised the manuscript for key intellectual content. All authors have approved the final version of the manuscript. TWH is responsible for the integrity of the work as a whole.
Rights and permissions
About this article
Cite this article
von Scholten, B.J., Hasbak, P., Christensen, T.E. et al. Cardiac 82Rb PET/CT for fast and non-invasive assessment of microvascular function and structure in asymptomatic patients with type 2 diabetes. Diabetologia 59, 371–378 (2016). https://doi.org/10.1007/s00125-015-3799-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-015-3799-x