Abstract
Aims/hypothesis
A diet rich in meat has been reported to contribute to the risk of type 2 diabetes. The present study aims to investigate the association between meat consumption and incident type 2 diabetes in the EPIC-InterAct study, a large prospective case-cohort study nested within the European Prospective Investigation into Cancer and Nutrition (EPIC) study.
Methods
During 11.7 years of follow-up, 12,403 incident cases of type 2 diabetes were identified among 340,234 adults from eight European countries. A centre-stratified random subsample of 16,835 individuals was selected in order to perform a case-cohort design. Prentice-weighted Cox regression analyses were used to estimate HR and 95% CI for incident diabetes according to meat consumption.
Results
Overall, multivariate analyses showed significant positive associations with incident type 2 diabetes for increasing consumption of total meat (50 g increments: HR 1.08; 95% CI 1.05, 1.12), red meat (HR 1.08; 95% CI 1.03, 1.13) and processed meat (HR 1.12; 95% CI 1.05, 1.19), and a borderline positive association with meat iron intake. Effect modifications by sex and class of BMI were observed. In men, the results of the overall analyses were confirmed. In women, the association with total and red meat persisted, although attenuated, while an association with poultry consumption also emerged (HR 1.20; 95% CI 1.07, 1.34). These associations were not evident among obese participants.
Conclusions/interpretation
This prospective study confirms a positive association between high consumption of total and red meat and incident type 2 diabetes in a large cohort of European adults.
Similar content being viewed by others
Introduction
Recent estimates from the International Diabetes Federation indicate that, in the year 2011, 366 million people in the world had diabetes and this estimate is projected to increase to 552 million by 2030 [1]. In the European Union, type 2 diabetes and impaired glucose tolerance currently represent two of the major public health concerns [2]. Moreover, at present there is no real cure for type 2 diabetes but only long-term treatment with glucose-lowering drugs or insulin. In this scenario the identification of primary prevention strategies for type 2 diabetes represents an important issue.
While individual characteristics such as age, overweight or obesity, family history, sedentary lifestyle, ethnicity, hypertension and hyperlipidaemia are established risk factors for type 2 diabetes [3], less is known about the influence of dietary factors.
Three recent meta-analyses of prospective studies emphasised that a diet rich in red and processed meat consumption is an important and independent contributor to type 2 diabetes risk [4–6]. In these meta-analyses a large proportion of the available studies of the association between dietary habits and type 2 diabetes risk were conducted in the USA. More recently, several studies have been conducted in European countries confirming the association between meat consumption and risk of type 2 diabetes in European populations [7–11].
The present study aims to investigate the association between consumption of total meat and meat subtypes and incident type 2 diabetes in a large collaborative project including adults from 26 cohorts in eight European countries participating in the ‘InterAct project, an examination of the interaction of genetic and lifestyle factors on the incidence of type 2 diabetes’ [12], thus taking into account differences in meat consumption patterns across Europe [13, 14].
Methods
Study design
The EPIC-InterAct study is a large prospective case-cohort study nested within the European Prospective Investigation into Cancer and Nutrition (EPIC) [15]. Its aim is to investigate the influence of lifestyle and genetic factors (and their interaction) on the risk of developing type 2 diabetes in a large cohort of adults from eight European countries [12]. The EPIC study was initiated in the late 1980s as a collaboration between 23 research institutions in ten European countries (Denmark, France, Germany, Italy, the Netherlands, Spain, Sweden, UK, Greece and Norway). Greece and Norway did not participate in the EPIC-InterAct study. The EPIC study has been previously described by Riboli et al [15].
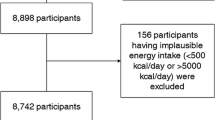
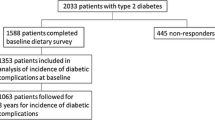
During a mean follow-up of 11.7 years a total of 12,403 verified newly diagnosed cases of type 2 diabetes were identified among 340,234 EPIC participants (men and women aged 20-80 years at baseline with a stored blood sample and reported diabetes status). Using a case-cohort design, a centre-stratified random subcohort of 16,835 participants (5%) was selected from the 340,234 EPIC participants. After exclusions of participants with prevalent diabetes (n = 548) or those with missing data on diet (n = 117), smoking status (n = 241), BMI (n = 169), physical activity (n = 289) or education (n = 479), as well as those who fell in the top or bottom 1% of the ‘energy intake/energy requirement ratio’ (n = 619), a total of 26,088 individuals remained for the analysis (14,529 subcohort non-cases, 729 subcohort type 2 diabetes cases and 10,830 non-subcohort type 2 diabetes cases).
All participants in the EPIC cohorts involved in the InterAct project gave their informed consent. The EPIC-InterAct study has been approved by the responsible ethics committees.
Dietary exposure assessment
At baseline, in the EPIC study, total daily consumption of food items was assessed for each participant by country-specific validated dietary questionnaires [16]. The total daily intake of each nutrient and the total daily energy intake were calculated [17]. The mean daily intake of meat iron was calculated as the mean of the total daily intake of iron (both heme and non-heme iron) from all types of meat. Glycaemic index and glycaemic load values were calculated based on glucose as a reference [18].
In the present study, the food group ‘red meat’ included the daily consumption (g) of unprocessed beef, pork, veal, mutton, lamb, goat and horse, hamburgers, meatballs and minced meat. The food group ‘poultry’ included chicken, hen, turkey, duck and goose; also domestic rabbit was added to this group. The food group ‘processed meat’ included bacon-, ham- and liver-containing items and all other processed meats (black pudding, chorizo, sausages, corned beef). The category ‘offals’ included liver, kidney, tripe, tongue, heart and sweetbread. A ‘red and processed meat’ group was created by combining the ‘red meat’ and the ‘processed meat’ groups. A ‘total meat’ group was also created by combining all types of meat.
Non-dietary exposure assessment
At baseline, in the EPIC study, information on lifestyle habits (including tobacco smoking, alcohol drinking and physical activity), education, occupation, previous diseases and reproductive history was collected by means of a specific lifestyle questionnaire. Height, weight, waist and hip circumference of participants were also collected.
Ascertainment and verification of type 2 diabetes incident cases
In each InterAct centre a list of all ascertained type 2 diabetes incident cases was created including individuals with evidence of type 2 diabetes from self-reported history of diabetes during follow-up contacts, linkage to primary and secondary care registers, type 2 diabetes-specific medication use and type 2 diabetes diagnosis reported in hospital admissions records or in mortality data. A detailed description of the ascertainment and verification procedure in all InterAct centres is provided elsewhere [12]. Follow-up was censored at the date of diagnosis, 31 December 2007 or the date of death, whichever came first.
Statistical analysis
Sex-specific quintiles of daily consumption of total meat, red meat, processed meat, red and processed meat, poultry and meat iron were obtained based on the subcohort sample. Sex-specific tertiles were obtained for offals due to their small daily consumption.
Within the subcohort sample the distribution of the main baseline non-dietary characteristics according to sex-specific quintiles of total meat consumption were explored. Generalised linear models, adjusted for age and daily energy intake at enrolment, were used to explore the baseline dietary variables.
Cox regression, with an estimation procedure for case-cohort designs according to the Prentice weighting method [19], was used to estimate HR and 95% CI of incident diabetes according to sex-specific quantiles of consumption of total meat, red meat, processed meat, red and processed meat, poultry, offals and meat iron. The time at entry was age at recruitment; exit time was the age at which participants were diagnosed with diabetes, died, were lost-to-follow-up or were censored at the end of the follow-up period, whichever came first. HR and 95% CI were computed with the lowest quantile of consumption as reference. Tests for linear trend in HR were based on medians across quantiles. In the basic model the baseline hazard function was stratified by centre and adjusted for sex and energy intake (natural log kJ). In multivariate model 1, analyses were performed stratified by centre and adjusted for sex, energy intake, smoking status (dummy variables for former and current smokers; never smokers as reference), alcohol (quintiles of daily intake), physical activity (four levels) and educational level (five levels) based on a priori knowledge of the main risk factors for type 2 diabetes [3, 20–22]. In multivariate model 2, a term for BMI (continuous) was added. The same models were performed with each type of meat and meat iron as continuous variables (50 g increments for total meat, red meat, processed meat, red and processed meat, and poultry; 10 g increments for offals; 1 mg increments for meat iron). Further analyses were performed with adjustment for intake of other foods and nutrients such as potatoes, total vegetables, bread and pasta, fish, cakes, soft drinks, coffee (50 g increments), total fats, magnesium, fibre and glycaemic load (continuous). Further analyses were also performed with meat consumption values scaled by additive calibration [23].
Possible effect modification by sex was tested by adding to multivariate model 2 the corresponding interaction terms obtained from quantiles of intake of the several meat items. The likelihood ratio test was used to assess the significance of the interaction terms. Multivariate model 2 was then performed separately by sex. Possible effect modification by BMI was also tested by adding to the model the corresponding interaction terms. Models were performed separately by BMI categories (<25, 25–30, ≥30 kg/m2).
Sex-specific models, simultaneously adjusted for red meat, processed meat, poultry and offals (sex-specific quantiles of consumption) were also performed in order to explore the effect of the different meat groups adjusting for each other.
Random-effect meta-analysis was used to assess heterogeneity (I 2 statistic) among countries in the association between meat consumption (overall and by specific types) or meat iron intake and occurrence of type 2 diabetes.
Sensitivity analyses were performed by excluding participants with myocardial infarction, angina, stroke, hypertension or hyperlipidaemia at baseline and by excluding the first 2 years of follow-up.
Analyses were performed with Stata 9.2 (StataCorp, TX, USA).
Results
The baseline non-dietary characteristics of the subcohort sample according to quintiles of consumption of total meat are reported in Table 1. In comparison with individuals in the lowest quintile of total meat consumption, those in the highest quintile were less educated, had higher waist circumference and BMI and were more frequently current smokers. The baseline non-dietary characteristics of the subcohort sample according to country are reported in electronic supplementary material (ESM) Table 1. The mean estimates of daily consumption of the main foods and nutrients in subcohort participants according to quintiles of consumption of total meat are shown in Table 2.
The mean daily consumption of the several types of meat in the subcohort sample is reported in ESM Table 2. Mean daily consumption of total meat by country ranged from 85.2 g/day (SD 54.1) in the UK to 134.3 g/day (SD 60.2) in Denmark.
In Table 3, a positive association with type 2 diabetes was observed in the basic model, comparing highest vs lowest quantile of consumption of total meat, red meat, processed meat, offals, poultry and meat iron. In multivariate model 1, the association was significant for increments of total meat (50 g: HR 1.18; 95% CI 1.15, 1.22), red meat (HR 1.18; 95% CI 1.13, 1.23), processed meat (HR 1.24; 95% CI 1.18, 1.31), offals (10 g: HR 1.08; 95% CI 1.03, 1.14), poultry (HR 1.12; 95% CI 1.05, 1.20) and meat iron (1 mg: HR 1.05; 95% CI 1.03, 1.08). In multivariate model 2 (including adjustment for BMI), the association was still significant for total meat (HR 1.08; 95% CI 1.05, 1.12), red meat (HR 1.08; 95% CI 1.03, 1.13) and processed meat (HR 1.12; 95% CI 1.05, 1.19). A borderline suggestion remained for meat iron (HR 1.02; 95% CI 0.998, 1.04). No association persisted for poultry and offals. Results from crude and adjusted models according to quantiles of consumption are also shown. After performing multivariate model 2 with further adjustment for consumption of other foods (total vegetables, bread, pasta, fish and cakes) the results did not materially change: total meat HR 1.08 (95% CI 1.04, 1.11); red meat HR 1.07 (95% CI 1.02, 1.13); processed meat HR 1.12 (95% CI 1.05, 1.18); meat iron HR 1.02 (95% CI 0.996, 1.03). When meat consumption was scaled by additive calibration, significant associations with type 2 diabetes were lightly strengthened. Non-significant associations remained unchanged.
Significant interactions with sex were observed for consumption of total meat, red meat, processed meat, poultry and meat iron intake (all p ≤ 0.01). In the overall models a 50% lower point estimate for HR in all quintiles was observed in women compared with men, while the linear relationship between total meat consumption and type 2 diabetes risk had a similar slope in both sexes (ESM Fig. 1). Results from sex-specific analyses (Table 4) showed a weakening of the association and a consequent lack of significance for processed meat and red and processed meat consumption in women but not in men. A significant positive association with type 2 diabetes risk was confirmed, however, in women, for total and red meat (p for trend 0.003 and 0.042, respectively) and for poultry consumption (p for trend 0.015). Similar results were obtained after further adjustment for menopausal status (data not shown). In men, the results obtained in the total sample were all confirmed. In sex-specific models simultaneously adjusted for consumption of red meat, processed meat, poultry and offals, the significant positive associations between red and processed meat and type 2 diabetes risk were confirmed among men, while no association emerged for offals and poultry. Among women only the significant positive association between poultry and incident type 2 diabetes persisted (data not shown).
A significant interaction with BMI was observed for the association with total meat, red meat, processed meat and poultry consumption (all p < 0.0001). Results from the analyses performed separately for BMI classes showed a progressive attenuation of the positive associations between meat consumption and incident type 2 diabetes from normal-weight to obese individuals (ESM Table 3). The positive associations between quintiles of consumption of total meat, processed meat, and red and processed meat with type 2 diabetes risk were indeed statistically significant in normal-weight and overweight individuals, but were borderline or not significant among obese individuals.
Country-specific random-effect meta-analyses showed overall a significant between-country heterogeneity for poultry consumption (Fig. 1d; I 2 = 58.3%; p = 0.019). Among women the meta-analyses showed, in all countries except the UK, a positive association between poultry consumption and type 2 diabetes risk that reached statistical significance in France, Italy and Sweden (ESM Fig. 2a; I 2 = 37.7%; p = 0.129). Among men a significant between-country heterogeneity emerged for poultry consumption (ESM Fig. 2b; I 2 = 53.0%; p = 0.047). Country-specific random-effect meta-analysis also showed a significant between-country heterogeneity for meat iron intake overall (Fig. 1f; I 2 = 61.0%; p = 0.012). Among men a significant between-country heterogeneity emerged for meat iron intake (ESM Fig. 3b; I 2 = 59.0%; p = 0.023). For all the other types of meat no significant heterogeneity emerged (Fig. 1).
Country-specific and overall HR for type 2 diabetes associated with 50 g increments of consumption of total meat (a), red meat (b), processed meat (c), poultry (d), offals (e) and meat iron intake (1 mg increments) (f) overall. HR and 95% CI derived by modified Cox proportional models stratified by centre and adjusted for sex, energy intake (log kJ), BMI (continuous), smoking status (dummy variable for former and current smokers), alcohol (quintiles of daily intake), physical activity (four levels) and education (five levels). Weights are from random effects analysis
The results did not materially change when sensitivity analyses were performed that excluded a total of 9,865 individuals reporting a history of myocardial infarction (n = 547), angina (n = 522), stroke (n = 261), hypertension (n = 6,863) or hyperlipidaemia (n = 4,402) at baseline, or that excluded those with a diagnosis of type 2 diabetes in the first 2 years after recruitment (n = 1,037).
Discussion
In this large European prospective study we found an overall positive association between consumption of meat and risk of type 2 diabetes. Individuals in the highest quintiles of consumption of total meat had a higher risk of developing type 2 diabetes compared with those in the lowest quintile of consumption. According to specific types of meat, we observed a higher risk of type 2 diabetes in high consumers of red and processed meat overall, in male high consumers of red meat, processed meat and meat iron and in female high consumers of poultry.
The large amount of information on health and lifestyle items collected at baseline allowed control for several possible confounders of the meat–diabetes association. After controlling for these well-known risk factors for type 2 diabetes (including sex, BMI, cigarette smoking, alcohol consumption, physical inactivity and educational level), the positive associations between total meat, red meat and processed meat and type 2 diabetes risk in the basic model were indeed largely attenuated, although the associations remained statistically significant. Nevertheless further residual confounding effects cannot be excluded.
No screening for undiagnosed type 2 diabetes was done, while detailed information on clinical diabetes diagnosed before recruitment was collected at baseline. During the ascertainment and verification procedure for incident cases of type 2 diabetes, additional cases of prevalent diabetes not reported in the baseline questionnaire were also identified and excluded from these analyses.
In a series of sensitivity analyses we excluded participants with a diagnosis of myocardial infarction, angina, stroke, hypertension or hyperlipidaemia at baseline and participants with a diagnosis of type 2 diabetes in the first 2 years of follow-up. In these subgroups dietary changes towards a ‘healthier’ pattern might have occurred as a consequence of the clinical diagnosis of a chronic disease or prediabetic condition, possibly leading to a distortion of the real associations between meat and diabetes risk. After exclusions of these subgroups no relevant changes were observed in the association between meat consumption and type 2 diabetes.
Imprecise dietary assessment or inaccuracies in self-reporting of adjusting variables, as sources of potential residual confounding, may represent a limitation of all epidemiological studies, including the current one. Possible errors in the collection of individual dietary habits at baseline by country-specific food frequency questionnaires were partially overcome by the exclusion of individuals who fell in the top or bottom 1% of the ‘energy intake/energy requirement ratio’.
Our conclusions are partially consistent with the results of three recent systematic reviews and meta-analyses. In the review by Aune et al (12 cohort studies from the USA, Europe, Asia and Australia) [4], a statistically significant positive association between total red meat and processed meat and type 2 diabetes risk emerged (21% and 41% increased risk for highest vs lowest intake, respectively), while total meat consumption was not significantly associated. In the review by Micha et al (seven cohort studies from the USA, Germany and China) [5], a statistically significant positive association emerged between processed meat and the combination of processed and unprocessed red meat and risk of type 2 diabetes (19% and 12% increased risk for 50 and 100 g/day, respectively), which is well in agreement with our estimates. Also, in the more recent review by Pan et al (nine cohort studies from the USA, Finland, Germany and China) [6], both unprocessed and processed red meat were significantly associated with an increased risk of type 2 diabetes (19% and 51% increased risk for 100 and 50 g/day, respectively).
In a study aimed to examine the association between meat consumption and risk of type 2 diabetes in a large cohort of Finnish middle-aged male smokers [9], over 1,000 incident cases of diabetes were identified in 12 years of follow-up. High total and processed meat consumption emerged as risk factors for type 2 diabetes with 50% and 37% increased adjusted risks, respectively, in the highest vs the lowest quintiles.
In 2012, two prospective studies that aimed to investigate the association between meat consumption and type 2 diabetes were performed in two European countries. In the frame of a prospective study among 66,118 disease-free French women (1,369 cases of incident diabetes identified between 1993 and 2007), one serving increment of processed meat was associated with a 29% increased risk [10]. In a prospective cohort of 4,366 Dutch participants, 456 diabetes cases were confirmed during a median follow-up period of 12.4 years. In the highest category of red and processed meat consumption, compared with the lowest category, a 42% and 87% increased risk was shown, respectively [11]. These results from specific countries were confirmed in our study, which included, for the first time, a large series of adults from the general population of several European countries in the same analysis, thus allowing an evaluation of the association between meat consumption and diabetes independently of country-specific dietary patterns.
The results of the sex-specific analysis showed a significant positive association between total meat consumption and type 2 diabetes risk both for women and men, with women showing a 50% lower risk in comparison with men at all levels of consumption. This positive association seems, however, to be driven by different types of meat consumed among women and men (red and processed meat for men, red meat and poultry for women). The finding of a positive association between type 2 diabetes and poultry consumption in women is not consistent with findings in several previous studies [24–26]. In their meta-analysis, Pan et al [6] modelled the substitution of total red meat consumption with poultry consumption and showed a lower risk of type 2 diabetes. On the other hand, in a case–control study (192 cases of incident type 2 diabetes and 382 control subjects) nested in the population-based EPIC-Potsdam cohort a dietary pattern score inversely associated with diabetes-related biomarkers was derived by reduced rank regression. Low consumption of poultry, high-calorie soft drinks, beer, red meat, processed meat, legumes and white bread was associated with a substantially reduced incidence of type 2 diabetes [27].
The borderline or non-significant associations between consumption of total meat, red meat, processed meat, and red and processed meat and type 2 diabetes among obese participants and the effect modification by BMI categories could be explained by the strong independent effect of obesity on type 2 diabetes risk. The important role of overweight and obesity in the onset of new cases of type 2 diabetes was discussed in a recent meta-analysis [28], while obesity has been cited as an important factor accounting for more than half of new diabetes cases [20]. This is also evident from our analyses, as BMI was the covariate that induced the largest attenuation of risk estimates for type 2 diabetes. On the other hand, obese participants might have a greater tendency to under-report meat consumption, thus contributing to attenuation of the association between meat intake and type 2 diabetes.
The positive association with meat was also independent of the consumption of the other main food items that were added to the model. A number of possible hypotheses have been considered in order to clarify the mechanisms responsible for the positive association of meat consumption with incidence of type 2 diabetes. It has been observed that nitrites, frequently used for preservation of meat and meat products, may have a toxic effect on pancreatic beta cells, mediated by the formation of nitrosamines in the stomach or in the meat product itself. Nitrosamines could also be produced in well cooked meat from heterocyclic amines or polycyclic aromatic hydrocarbons [29]. Some nitrosamines were found to be associated with type 1 diabetes in humans [30], while streptozotocin, a nitrosamine-related compound, was found to be associated with type 2 diabetes in animal models [31, 32]. Advanced glycation end-products, present in meat and meat products as a result of cooking or processing, have been associated with insulin resistance or type 2 diabetes both in animal models [33] and in humans [34]. A role in the onset of type 2 diabetes might be played by saturated and trans-fatty acids present in meat. Several studies suggested a detrimental effect of saturated fat (animal origin foods as main source) [35–38], or trans-fatty acids (main sources including also beef, lamb, mutton and derived products) [39] in the development of type 2 diabetes due to adverse metabolic effects on insulin sensitivity.
A diet rich in meat and meat products could lead to an increase in the body’s iron stores, which is suspected to impair insulin sensitivity and increase blood glucose concentration thus leading to higher type 2 diabetes risk [40–42]. Heme iron is in fact more bioavailable than non-heme iron, since its absorption is partially independent of body iron status and is less influenced by consumption of various foods and nutrients [43, 44]. Heme iron could, moreover, promote the endogenous formation of nitrosamines [45]. In agreement with these hypotheses, in our study we found that intake of iron from meat (consisting of heme iron in large proportion [46]) was associated with a higher risk of type 2 diabetes. A further consideration should be kept in mind in relation to the different heme iron status in men and women. In premenopausal women a significant amount of iron is lost during menstrual cycles, leading to lower body iron stores than in men and postmenopausal women [43]. This could partially explain the weaker association observed in our study between red and processed meat consumption and type 2 diabetes in women compared with men.
A clear excess of diabetes has been reported among workers in the meat industry [47, 48], and it has been proposed that this might be related to exposures to zoonotic infective agents present in fresh cuts of meat, including poultry [49], although overweight might play a relevant role in this category of workers.
In conclusion this study involving a large cohort of European adults showed a positive association between high consumption of total and red meat and incident type 2 diabetes overall. Among men, a positive association between high consumption of total, red and processed meat and incident type 2 diabetes emerged. Among women, a positive association between high consumption of total meat, red meat and poultry and incident type 2 diabetes emerged. This study provides further evidence of the role of meat and meat products as risk factors to be considered in the identification of primary prevention strategies for type 2 diabetes.
Abbreviations
- EPIC:
-
European Prospective Investigation into Cancer and Nutrition
- I 2 :
-
Index of between-study heterogeneity
References
International Diabetes Federation (2011) Diabetes atlas 5th edn. Available from www.idf.org/diabetesatlas/5e/the-global-burden accessed 25 May 2012
Valensi P, Schwarz EH, Hall M, Felton AM, Maldonato A, Mathieu C (2005) Pre-diabetes essential action: a European perspective. Diabetes Metab 31:606–620
Sherwin RS, Anderson RM, Buse JB et al (2003) The prevention or delay of type 2 diabetes. Diabetes Care 26(Suppl 1):S62–S69
Aune D, Ursin G, Veierød MB (2009) Meat consumption and the risk of type 2 diabetes: a systematic review and meta-analysis of cohort studies. Diabetologia 52:2277–2287
Micha R, Wallace SK, Mozaffarian D (2010) Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus. A systematic review and meta-analysis. Circulation 121:2271–2283
Pan A, Sun Q, Bernstein AM et al (2011) Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. Am J Clin Nutr 94:1088–1096
Montonen J, Järvinen R, Heliövaara M, Reunanen A, Aromaa A, Knekt P (2005) Food consumption and the incidence of type II diabetes mellitus. Eur J Clin Nutr 59:441–448
Schulze MB, Hoffmann K, Boeing H et al (2007) An accurate risk score based on anthropometric, dietary, and lifestyle factors to predict the development of type 2 diabetes. Diabetes Care 30:510–515
Männistö S, Kontto J, Kataja-Tuomola M, Albanes D, Virtamo J (2010) High processed meat consumption is a risk factor of type 2 diabetes in the Alpha-Tocopherol, Beta-Carotene Cancer Prevention study. Br J Nutr 103:1817–1822
Lajous M, Tondeur L, Fagherazzi G, de Lauzon-Guillain B, Boutron-Ruaualt MC, Clavel-Chapelon F (2012) Processed and unprocessed red meat consumption and incident type 2 diabetes among French women. Diabetes Care 35:128–130
van Woudenbergh GJ, Kuijsten A, Tigcheler B et al (2012) Meat consumption and its association with C-reactive protein and incident type 2 diabetes: The Rotterdam Study. Diabetes Care 35:1499–1505
The InterAct Consortium (2011) Design and cohort description of the InterAct Project: an examination of the interaction of genetic and lifestyle factors on the incidence of type 2 diabetes in the EPIC study. Diabetologia 54:2272–2282
Halkjaer J, Olsen A, Bjerregaard LJ et al (2009) Intake of total, animal and plant proteins, and their food sources in 10 countries in the European Prospective Investigation into Cancer and Nutrition. Eur J Clin Nutr 63(Suppl 4):S16–S36
Linseisen J, Kesse E, Slimani N et al (2002) Meat consumption in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohorts: results from 24-hour dietary recalls. Public Health Nutr 5:1243–1258
Riboli E, Hunt KJ, Slimani N et al (2002) European Prospective Investigation into Cancer and Nutrition (EPIC): study populations and data collection. Public Health Nutr 5:1113–1124
Margetts BM, Pietinen P (1997) European Prospective Investigation into Cancer and Nutrition: validity studies on dietary assessment methods. Int J Epidemiol 26(Suppl 1):S1–S5
Slimani N, Deharveng G, Unwin I et al (2007) The EPIC Nutrient Database Project (ENDB): a first attempt to standardize nutrient databases across the 10 European countries participating in the EPIC study. Eur J Clin Nutr 61:1037–1056
van Bakel MM, Slimani N, Feskens EJ et al (2009) Methodological challenges in the application of the glycemic index in epidemiological studies using data from the European Prospective Investigation into Cancer and Nutrition. J Nutr 139:568–575
Barlow WE, Ichikawa L, Rosner D, Izumi S (1999) Analysis of case-cohort designs. J Clin Epidemiol 52:1165–1172
Psaltopoulou T, Ilias I, Alevizaki M (2010) The role of diet and lifestyle in primary, secondary, and tertiary diabetes prevention: a review of meta-analyses. Rev Diabet Stud 7:26–35
Feskens EJ, Loeber JG, Kromhout D (1994) Diet and physical activity as determinants of hyperinsulinemia: the Zutphen Elderly Study. Am J Epidemiol 140:350–360
Cox M, Boyle PJ, Davey PG, Feng Z, Morris AD (2007) Locality deprivation and type 2 diabetes incidence: a local test of relative inequalities. Soc Sci Med 65:1953–1964
Kaaks R, Riboli E (1997) Validation and calibration of dietary intake measurements in the EPIC project: methodological considerations. European Prospective Investigation into Cancer and Nutrition. Int J Epidemiol 26(Suppl 1):S15–S25
Steinbrecher A, Erber E, Grandinetti A, Kolonel LN, Maskarinec G (2011) Meat consumption and risk of type 2 diabetes: the multiethnic cohort. Public Health Nutr 14:568–574
Schulze MB, Manson JE, Willett WC, Hu FB (2003) Processed meat intake and incidence of type 2 diabetes in younger and middle-aged women. Diabetologia 46:1465–1473
Villegas R, Shu XO, Gao YT et al (2006) The association of meat intake and the risk of type 2 diabetes may be modified by body weight. Int J Med Sci 3:152–159
Heidemann C, Hoffmann K, Spranger J et al (2005) A dietary pattern protective against type 2 diabetes in the European Prospective Investigation into Cancer and Nutrition (EPIC)—Potsdam Study cohort. Diabetologia 48:1126–1134
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH (2009) The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health 9:88
Lijinsky W (1999) N-Nitroso compounds in the diet. Mutat Res 443:129–138
Dahlquist G (1998) The aetiology of type 1 diabetes: an epidemiological perspective. Acta Paediatr Suppl 425:5–10
Ito M, Kondo Y, Nakatani A, Naruse A (1999) New model of progressive non-insulin-dependent diabetes mellitus in mice induced by streptozotocin. Biol Pharm Bull 22:988–989
Tong M, Neusner A, Longato L, Lawton M, Wands JR, de la Monte SM (2009) Nitrosamine exposure causes insulin resistance diseases: relevance to type 2 diabetes mellitus, non-alcoholic steatohepatitis, and Alzheimer's disease. J Alzheimers Dis 17:827–844
Hofmann SM, Dong HJ, Li Z et al (2002) Improved insulin sensitivity is associated with restricted intake of dietary glycoxidation products in the db/db mouse. Diabetes 51:2082–2089
Peppa M, Goldberg T, Cai W, Rayfield E, Vlassara H (2002) Glycotoxins: a missing link in the ‘relationship of dietary fat and meat intake in relation to risk of type 2 diabetes in men’. Diabetes Care 25:1898–1899
Feskens EJ, Virtanen SM, Räsänen L et al (1995) Dietary factors determining diabetes and impaired glucose tolerance. A 20-year follow-up of the Finnish and Dutch cohorts of the Seven Countries Study. Diabetes Care 18:1104–1112
Maron DJ, Fair JM, Haskell WL (1991) Saturated fat intake and insulin resistance in men with coronary artery disease. The Stanford Coronary Risk Intervention Project Investigators and Staff. Circulation 84:2020–2027
Parker DR, Weiss ST, Troisi R, Cassano PA, Vokonas PS, Landsberg L (1993) Relationship of dietary saturated fatty acids and body habitus to serum insulin concentrations: the Normative Aging Study. Am J Clin Nutr 58:129–136
Marshall JA, Bessesen DH, Hamman RF (1997) High saturated fat and low starch and fibre are associated with hyperinsulinaemia in a non-diabetic population: the San Luis Valley Diabetes Study. Diabetologia 40:430–438
Salmerón J, Hu FB, Manson JE et al (2001) Dietary fat intake and risk of type 2 diabetes in women. Am J Clin Nutr 73:1019–1026
Fernández-Real JM, Ricart-Engel W, Arroyo E et al (1998) Serum ferritin as a component of the insulin resistance syndrome. Diabetes Care 21:62–68
Hua NW, Stoohs RA, Facchini FS (2001) Low iron status and enhanced insulin sensitivity in lacto-ovo vegetarians. Br J Nutr 86:515–519
Jiang R, Manson JE, Meigs JB, Ma J, Rifai N, Hu FB (2004) Body iron stores in relation to risk of type 2 diabetes in apparently healthy women. JAMA 291:711–717
Cook JD (1990) Adaptation in iron metabolism. Am J Clin Nutr 51:301–308
Monsen ER (1988) Iron nutrition and absorption: dietary factors which impact iron bioavailability. J Am Diet Assoc 88:786–790
Bingham SA, Hughes R, Cross AJ (2002) Effect of white versus red meat on endogenous N-nitrosation in the human colon and further evidence of a dose response. J Nutr 132(11 Suppl):3522S–3525S
Carpenter CE, Clark E (1995) Evaluation of methods used in meat iron analysis and iron content of raw and cooked meats. J Agric Food Chem 43:1824–1827
Johnson ES, Zhou Y (2007) Non-cancer mortality in supermarket meat workers. J Occup Environ Med 49:846–852
Johnson ES, Yau LC, Zhou Y, Singh KP, Ndetan H (2010) Mortality in the Baltimore union poultry cohort: non-malignant diseases. Int Arch Occup Environ Health 83:543–552
Porte D Jr, Sherwin RS, Baron A (2003) Ellenberg and Rifkin’s diabetes mellitus, 6th edn. McGraw-Hill Medical Publishing Division, New York
Acknowledgements
We thank all EPIC participants and staff for their contribution to the study.
Funding
The EPIC-InterAct study received funding from the European Union (Integrated Project LSHM-CT-2006-037197 in Framework Programme 6 of the European Community). In addition, InterAct investigators acknowledge funding from the following agencies: DP: Italian Association for Research on Cancer (AIRC) and PIO Programma Integrato Oncologia; DLvdA: Dutch Ministry of Public Health, Welfare and Sports (VWS), Netherlands Cancer Registry (NKR), LK Research Funds, Dutch Prevention Funds, Dutch ZON (Zorg Onderzoek Nederland), World Cancer Research Fund (WCRF), Statistics Netherlands; FLC: Cancer Research UK; PWF: Swedish Research Council, Novo Nordisk, Swedish Diabetes Association, Swedish Heart–Lung Foundation; JMH: Health Research Fund of the Spanish Ministry of Health, Murcia Regional Government (no. 6236); KTK: Medical Research Council UK, Cancer Research UK; PMN: Swedish Research Council; KO: Danish Cancer Society; LR-S: Asturias Regional Government; OR: Västerboten County Council; GD and IS: NL Agency grant IGE05012, incentive grant from the board of UMC Utrecht; AMWS: Dutch Ministry of Public Health, Welfare and Sports (VWS), Netherlands Cancer Registry (NKR), LK Research Funds, Dutch Prevention Funds, Dutch ZON (Zorg Onderzoek Nederland), World Cancer Research Fund (WCRF), Statistics Netherlands; BT: German Cancer Aid; AT: Danish Cancer Society; RT: AIRE-ONLUS Ragusa, AVIS-Ragusa, Sicilian Regional Government; ER: Imperial College Biomedical Research Centre; PJ: Spanish Ministry of Health (ISCIII RETICC RD06/0020), Spanish Regional Governments of Andalusia, Asturias, Basque Country, Murcia (no. 6236) and Navarra, and the Catalan Institute of Oncology.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
Author contributions were as follows: BB, DP and GM analysed the data and wrote the paper. SJS, MBS, MG, DLvdA and FS made extensive revisions to subsequent drafts. NW designed the research project. All authors contributed to the interpretation of data, revised the article critically for important intellectual content and approved the final version of the paper to be published.
Author information
Authors and Affiliations
Consortia
Additional information
The InterAct Consortium list of authors is shown in the Appendix.
Electronic Supplementary Materials
Below is the link to the electronic supplementary material.
ESM Fig. 1
(PDF 5 kb)
ESM Fig. 2
(PDF 9 kb)
ESM Fig. 3
(PDF 9 kb)
ESM Table 1
(PDF 14 kb)
ESM Table 2
(PDF 9 kb)
ESM Table 3
(PDF 15 kb)
Appendix
Appendix
The InterAct Consortium list of authors is as follows:
B. Bendinelli (Molecular and Nutritional Epidemiology Unit, Cancer Research and Prevention Institute [ISPO], Florence, Italy); D. Palli (Molecular and Nutritional Epidemiology Unit, Cancer Research and Prevention Institute [ISPO], Florence, Italy); G. Masala (Molecular and Nutritional Epidemiology Unit, Cancer Research and Prevention Institute [ISPO], Florence, Italy); S. J. Sharp (MRC Epidemiology Unit, Cambridge, UK); M. B. Schulze (Department of Molecular Epidemiology, German Institute of Human Nutrition, Potsdam-Rehbruecke, Germany); M. Guevara (Navarre Public Health Institute, Pamplona, Spain and CIBER de Epidemiología y Salud Pública [CIBERESP], Spain, URL www.ciberesp.es); D. L. van der A (National Institute for Public Health and the Environment [RIVM], Bilthoven, the Netherlands); F. Sera (Molecular and Nutritional Epidemiology Unit, Cancer Research and Prevention Institute [ISPO], Florence, Italy); P. Amiano (CIBER de Epidemiología y Salud Pública [CIBERESP], Spain, URL www.ciberesp.es, Public Health Division of Gipuzkoa, San Sebastian, Spain and Instituto BIO-Donostia, Basque Government, Spain); B. Balkau (INSERM, University Paris Sud, France); A. Barricarte (Navarre Public Health Institute, Pamplona, Spain and CIBER de Epidemiología y Salud Pública [CIBERESP], Spain, URL www.ciberesp.es); H. Boeing (Department of Epidemiology, German Institute of Human Nutrition Potsdam-Rehbruecke, Germany); F. L. Crowe (Cancer Epidemiology Unit, Nuffield Department of Clinical Medicine, University of Oxford, UK); C. C. Dahm (Department of Epidemiology, School of Public Health, Aarhus, Denmark and Department of Cardiology, Aalborg Hospital, Denmark); G. Dalmeijer (Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, the Netherlands); B. de Lauzon-Guillain (University Paris Sud and INSERM, France); R. Egeberg (Danish Cancer Society Research Center, Copenhagen, Denmark ), G. Fagherazzi (INSERM, France); P. W. Franks (Department of Public Health and Clinical Medicine, Umeå University, Sweden and Department of Clinical Sciences, Skåne University Hospital, Lund University, Malmö, Swede); V. Krogh (Fondazione IRCCS Istituto Nazionale dei Tumori, Milan, Italy); J. M. Huerta (CIBER de Epidemiología y Salud Pública [CIBERESP], Spain, URL www.ciberesp.es, and Department of Epidemiology, Murcia Regional Health Council, Spain); P. Jakszyn (Unit of Nutrition, Environment and Cancer, Cancer Epidemiology Research Programme. Catalan Institute of Oncology [ICO], Barcelona, Spain); K. T. Khaw (Department of Public Health and Primary Care, University of Cambridge, UK); K. Li (Division of Cancer Epidemiology, German Cancer Research Centre [DKFZ], Heidelberg, Germany); A. Mattiello (Department of Clinical and Experimental Medicine, Federico II University, Naples, Italy); P. M. Nilsson (Department of Clinical Sciences Medicine, University of Lund, Sweden); K. Overvad (Department of Cardiology, Aalborg Hospital, Denmark); F. Ricceri (Human Genetics Foundation [HuGeF], Torino, Italy); L. Rodríguez-Suárez (Public Health Directorate, Asturias, Spain); O. Rolandsson (Department of Public Health and Clinical Medicine, Umea University, Sweden); M. J. Sánchez (CIBER de Epidemiología y Salud Pública [CIBERESP], Spain, URL www.ciberesp.es, and Andalusian School of Public Health, Granada, Spain); N. Slimani (International Agency for Research on Cancer, Lyon, France); I. Sluijs (Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, the Netherlands); A. M. W. Spijkerman (National Institute for Public Health and the Environment (RIVM), Bilthoven, the Netherlands); B. Teucher (Division of Cancer Epidemiology, German Cancer Research Centre [DKFZ], Heidelberg, Germany); A. Tjonneland (Danish Cancer Society Research Center, Copenhagen, Denmark); R. Tumino (Cancer Registry and Histopathology Unit, ‘Civile - M.P. Arezzo’ Hospital, Ragusa, Italy); S. W. van den Berg (National Institute for Public Health and the Environment [RIVM], Bilthoven, the Netherlands); N. G. Forouhi (MRC Epidemiology Unit, Cambridge, UK); C. Langenberg (MRC Epidemiology Unit, Cambridge, UK); E. J. M. Feskens (Division of Human Nutrition - Section Nutrition and Epidemiology, University of Wageningen, the Netherlands); E. Riboli (Department of Epidemiology and Biostatistics, School of Public Health, Imperial College London, UK), N. J. Wareham (MRC Epidemiology Unit, Cambridge, UK).
Rights and permissions
About this article
Cite this article
The InterAct Consortium. Association between dietary meat consumption and incident type 2 diabetes: the EPIC-InterAct study. Diabetologia 56, 47–59 (2013). https://doi.org/10.1007/s00125-012-2718-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-012-2718-7