Abstract
Aims/hypothesis
The aim of this study was to ascertain whether treatment of GAD65 autoantibody (GADA)-positive diabetic patients with alum-formulated recombinant GAD65 (GAD-alum) is safe and does not compromise beta cell function.
Methods
This Phase 2, placebo-controlled, dose-escalation clinical trial, which was randomized through a central office, was performed in 47 GADA-positive type 2 diabetic patients, who received subcutaneous injections of GAD-alum (4 [n = 9], 20 [n = 8], 100 [n = 9] or 500 [n = 8] μg) or placebo (n = 13) at weeks 1 and 4 of the trial. Participants and caregivers were blinded to group assignments. The primary outcome was safety as assessed by neurological tests, medications and beta cell function evaluated over 5 years, representing the end of the trial.
Results
No severe study-related adverse events occurred during the 5 year follow-up. None of the dose groups was associated with an increased risk of starting insulin treatment compared with the placebo group. The use of oral hypoglycaemic agents did not differ between the dose groups. After 5 years, fasting C-peptide levels declined in the placebo group (−0.24; 95% CI −0.41 to −0.07 log10 nmol/l; p = 0.01) and the 500 µg dose group (−0.37; 95% CI −0.57 to −0.17 log10 nmol/l; p = 0.003), but not in the 4 µg (−0.10; 95% CI −0.28 to 0.07 log10 nmol/l; p = 0.20), 20 µg (0.04; 95% CI −0.12 to 0.19 log10 nmol/l; p = 0.58) and 100 µg (0.00; 95% CI −0.20 to −0.20 log10 nmol/l; p = 0.98) dose groups.
Conclusions/interpretation
The primary outcome of safety was achieved, since no severe study-related adverse events occurred.
Trial registration
Because the study was initiated before 1 July 2005, the protocol was not registered in a registry.
Funding
This trial was funded by the National Institutes of Health (grant numbers DK26190 and DK53004), the Swedish Research Council (grant number 72X-14064) and Diamyd Therapeutics (Stockholm, Sweden).
Similar content being viewed by others
Introduction
Autoimmune destruction of pancreatic islet beta cells is the major cause of type 1 diabetes mellitus [1]. This destruction is associated with cellular and humoral immune responses to several beta cell autoantigens, both of which can precede clinical diagnosis of diabetes. In particular, GAD65 autoantibody (GADA), insulinoma-associated antigen (IA-2A) or insulin autoantibody (IAA) with or without islet cell antibodies (ICAs) precede clinical onset with 80–90% of patients with type 1 diabetes having one or several of these autoantibodies at the time of diagnosis [2]. The presence of all three islet autoantibodies, i.e. GADA, IA-2A and IAA, also predicts type 1 diabetes [3, 4]. In addition, these autoantibodies, especially GADA, occur in up to 10% of adults clinically presenting with type 2 diabetes. This patient group is often referred to as latent autoimmune diabetes in adults (LADA) [5]. The disease process in LADA patients is similar to that in type 1 diabetes in that they share HLA genetic susceptibility and autoantibodies associated with type 1 diabetes. However, in comparison to type 1 diabetes, insulin secretion is higher and the rate of progression to insulin dependency is slower in LADA patients [6].
We previously reported 24 week data for a Phase 2 study in LADA patients treated with recombinant human GAD65 formulated with aluminium hydroxide (GAD-alum; Diamyd Therapeutics, Stockholm, Sweden) [7]. The results showed that administration of GAD-alum in escalating dosages was safe and did not compromise beta cell function. We have now followed the 47 patients prospectively for 5 years to evaluate long-term clinical safety and dose level effects on beta cell function.
Methods
Participants and trial design
The trial was designed as a randomised, double-blind, placebo-controlled, group comparison, dose-escalation study conducted in GADA-positive type 2 diabetic patients at the Department of Endocrinology, University Hospital MAS, Malmö and the Department of Medicine, St Görans Hospital, Stockholm, Sweden, as previously described in detail [7]. Randomisation was concealed by the clinical research organisation monitoring the study without any involvement by study investigators. Briefly, 47 patients were allocated to one of four groups receiving 4 μg (n = 9), 20 μg (n = 8), 100 μg (n = 9) or 500 μg (n = 8) of GAD-alum or placebo (n = 13). Sequential immunisation of each dose group was conducted after no safety issues had arisen at lower doses. Interim safety evaluation to approve dose escalation was conducted by a separate committee 4 weeks after the second GAD-alum injection. Nine patients in each group were planned to receive GAD-alum and three to receive placebo. A chart of participant flow through the study is presented in Electronic supplementary material (ESM) Fig. 1. The study was carried out according to the intent-to-treat principle. National regulatory and local ethics committee approvals were obtained for this study and written informed consent was obtained from participating individuals in accordance with the Declaration of Helsinki. Because the study was initiated before 1 July 2005, the protocol was not registered in a registry.
Patients were eligible to enter the trial if they fulfilled the following entry criteria at their first visit: (1) male or female patient aged 30 to 70 years; (2) diagnosed with type 2 diabetes within the previous 5 years; (3) presence of GADA; (4) diabetes treated only by diet, oral hypoglycaemic agents or both; (5) women of non child-bearing potential only; (6) absence of associated serious diseases or conditions that in the opinion of the investigators would exclude the patient from the trial; and (7) patients who had given written informed consent at the screening visit.
During the 5 year study period each patient was followed as an outpatient at regular intervals, with a total of 28 study visits during which islet autoantibodies, diabetes status, fasting lipids, haematological and biochemical variables were assessed and physical examinations, as well as the reporting of concomitant medication and adverse effects were undertaken. In total, 40/47 patients completed the 5 year study, which included information about adverse events. GADA and IA-2A were determined as previously described [8]. However, after 12 months, only GADA was analysed. Our laboratory is number 156 in the Diabetes Antibody Standardization Program for GADA and IA-2A [9]. Diabetes status assessment included fasting glucose, fasting and 2 h Sustacal-stimulated C-peptide, and HbA1c for assessment of long-term metabolic control. Fasting C-peptide continued to be measured after patients started insulin treatment, while fasting glucose, stimulated C-peptide and HbA1c were no longer assessed in patients starting insulin treatment. In the patients without insulin treatment, fasting glucose, and fasting and 2 h Sustacal-stimulated C-peptide were measured at baseline then at 2, 6, 9 and 12 months, and thereafter every half year up to year 5. HbA1c was similarly measured except that it started at 3 months. Blood samples for haematology were analysed for haemoglobin, erythrocyte count (including mean corpuscular volume and mean cell haemoglobin concentration) and packed cell volume, leucocyte cell count, differential white cell count and platelets. Biochemical variables analysed included plasma levels of glucose, C-peptide, HbA1c, urea, creatinine, phosphorus, total bilirubin, alkaline phosphatase, alanine transferase, glutamyl transferase, lactic dehydrogenase, amylase, albumin, C-reactive protein, total protein, and fasting lipid and lipoproteins. The criteria for the introduction of insulin treatment were left to the discretion of each attending physician. HLA was kindly determined by J.-X. She at the Center for Biotechnology and Genomic Medicine, Medical College of Georgia, Augusta, GA, USA as described previously [10]. Clinical neurological assessment and electromyography (EMG) were performed at baseline and after 6 months to detect adverse effects on the neuromuscular system [11, 12]. Thereafter, a clinical neurological assessment was performed each year until the end of the study (month 60).
Test substances
Diamyd Therapeutics provided sterile, pre-filled vials of GAD-alum and placebo for clinical trial use [7]. Briefly, the unmodified recombinant form of human GAD65 was formulated with aluminium hydroxide. The GAD65 was manufactured using baculovirus/insect cell expression of the cDNA for recombinant human GAD65 [13]. Manufacture of the GAD-alum was performed under strict conditions of current Good Manufacturing Practice. Each vial contained a sterile formulation of 4, 20, 100 or 500 μg of GAD65 in a constant amount of aluminium hydroxide. Coded vials containing an identical amount of aluminium hydroxide alone were used as placebo.
Statistical analysis
Exact χ 2 tests were used to examine for differences between the placebo and dose groups in the percentage of patients starting insulin treatment. A proportional hazard model tested for an increased risk of starting insulin treatment. Mean (SEM) absolute fasting log10 C-peptide levels were drawn using time plots. For each patient, we calculated the 5 year change in fasting log10 C-peptide levels from baseline and checked whether the changes in log values were normally distributed. One-sample t tests were used to test whether mean changes differed from zero. Two-sample independent t tests tested whether the mean change per dose group differed from placebo. Similar analyses were performed for HbA1c and stimulated C-peptide in participants who had not started insulin treatment. All graphs were generated using GraphPad PRISM 4.0 (GraphPad Software, San Diego, CA, USA) and analyses performed using SPSS 14 (www.spss.com, accessed 31 March 2008).
Results
Diabetes markers in the placebo and dose groups
On inspection, no important differences in baseline characteristics (high risk HLA, islet autoantibodies, BMI, LDL-cholesterol, HDL-cholesterol and triacylglycerol) were seen among the treatment and placebo participants (Table 1). Of the 47 patients, 20 (43%) had the type 1 diabetes high-risk HLA DQ B1*0302 allele including 5/47 (11%) with the high-risk DQB1*0201/*0302 genotype. Autoimmune diabetes was confirmed by the presence not only of GADA, which was an inclusion criteria, but also of ICAs in 33/47 (70%) of the patients.
Study-related adverse events
There were 14 serious adverse events (SAE) in ten patients during the 5 year follow-up. Four of these patients were in the placebo group (six SAE), one was in the 20 μg dose group (three SAE), two in the 100 μg dose group (two SAE) and three in the 500 μg dose group (three SAE). The SAE in the placebo group were: seizures, cholecystitis, myocardial infarction and cerebellar infarction leading to death in one patient, and subarachnoid bleeding and insulin treatment with hospitalisation due to cognitive dysfunction in one patient. The SAE in the 20 μg group occurred in the same patient and were myocardial infarction and fractures of the fibula and malleoli. The SAE in the 100 μg group were myocardial infarction and fracture of the left foot. The SAE in the 500 μg group were transurethral resection of a malignant bladder tumour, osteoarthritis in the knee and prostate cancer. None of the SAE was considered to be treatment-related by the local investigators and were evaluated by the independent study safety committee. There were no abnormal neurological assessments by clinical examination or by EMG, which was used to detect adverse effects on the neuromuscular system.
Characteristics of patients who started insulin treatment
The medications given at baseline and during follow-up (Table 2) indicate the use of various oral hypoglycaemic agents. Only seven patients were lost to follow-up.
None of the dose groups was associated with an increased risk of starting insulin treatment compared with the placebo group. Of the 40 patients who remained in the study, 19 started insulin treatment within 5 years of the prime dose being administered. Of these, ten (53%) had low fasting C-peptide (lower quartile <0.55 nmol/l) at baseline.
Beta cell function among all patients followed for 5 years
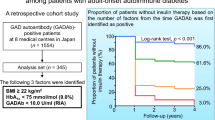
Over the time course, fasting C-peptide in the 20 µg dose group increased significantly within the 1st year compared with baseline and remained elevated (Fig. 1). Although not significant at 5 years compared with baseline, the increase in fasting C-peptide (0.04; 95% CI −0.12 to 0.19 log nmol/l; p = 0.58) in this dose group was significantly greater (0.28; 0.04, 0.51 log nmol/l; p = 0.01) than in the placebo group (Fig. 1). Fasting C-peptide remained unchanged over time in the 100 µg dose group (0.00; 95% CI −0.20 to 0.20 log nmol/l; p = 0.98). At 5 years, fasting C-peptide levels showed a decline from baseline in the placebo group (−0.24; 95% CI −0.41 to −0.07 log nmol/l; p = 0.01) (Fig. 1). In the 500 µg dose group there was also a decline from baseline (−0.37; 95% CI −0.57 to −0.17 log nmol/l; p = 0.003).
Fasting C-peptide levels (log nmol/l) when prime dose was administered (baseline) and at 1, 2, 3, 4 and 5 years thereafter in (a) placebo and (b) 4 μg, (c) 20 μg, (d) 100 μg and (e) 500 μg groups. Numbers in parentheses, patients (n) for whom levels were available. Values are shown as mean ± SEM. *p < 0.05 at 5 years vs. baseline
In the patients who were followed for 5 years (ESM Tables 1 and 2), the GAD-alum dose was significantly associated with the number of patients starting insulin treatment (placebo 7/11 [64%]; 4 μg group 5/7 [71%]; 20 μg 1/7 [14%]; 100 μg 1/7 [14%]; 500 μg 5/8 [63%]; p = 0.046). The time until start of insulin treatment was not associated with any of the GAD-alum dose groups. However, patients receiving a 20 or 100 µg dose had a reduced risk of starting insulin treatment (HR 0.29, 95% CI 0.10 to 0.90; p = 0.024).
Discussion
The primary aim of this Phase 2 study was to evaluate whether alum-formulated recombinant human GAD65 given to LADA patients is safe and does not compromise beta cell function. The results confirm our previous report after 24 weeks [7] and extend to 5 years the clinical safety of GAD-alum and the finding that beta cell function was not compromised. The design of this trial was also meant to create potential hypotheses for testing in future trials. Our data suggest that the 20 μg dose may be suitable for future clinical trials on safety and efficacy, since members of the 20 μg dose group increased their fasting C-peptide over 5 years compared with placebo.
The LADA form of diabetes occurs in about 10% of patients classified as type 2 diabetes and not initially requiring insulin [14]. However, as demonstrated in the UKPDS study, about 80% of adult individuals with recently diagnosed type 2 diabetes and GADA and ICAs progressed to insulin requirements within 6 years, indicating the autoimmune nature of this condition and the progressive beta cell destruction associated with it [15]. At present no treatment modalities have been effective in halting this progression to insulin-requiring diabetes [16]. The approach described here, using alum-formulated GAD65 in an attempt to immunomodulate GADA-positive LADA patients, therefore represents a novel way of interrupting or slowing down the disease progression that leads to beta cell loss and insulin requirement.
In conclusion, our 5 year follow-up of the 47 LADA patients who were given GAD-alum at escalating dosages shows that the treatment was safe and did not compromise beta cell function. It should be noted that our study cannot reliably exclude rare SAE as a result of treatment with human recombinant GAD65. Larger trials are needed to address this unavoidable limitation of any small randomised trial. The increase in fasting and stimulated C-peptide levels that had previously been reported after 6 months in the group given 20 μg was maintained during the 5 year follow-up. As there were no treatment-related SAE, further exploration of the immunomodulatory effects of 20 μg GAD-alum is warranted.
Abbreviations
- EMG:
-
Electromyography
- GADA:
-
GAD65 autoantibody
- IA-2A:
-
Insulinoma-associated antigen
- IAA:
-
Insulin autoantibody
- ICA:
-
Islet cell antibody
- LADA:
-
Latent autoimmune diabetes in adults
- SAE:
-
Serious adverse events
References
Gepts W (1965) Pathologic anatomy of the pancreas in juvenile diabetes mellitus. Diabetes 14:619–633
Graham J, Hagopian WA, Kockum I et al (2002) Diabetes incidence in Sweden study group; Swedish childhood diabetes study group: genetic effects on age-dependent onset and islet cell autoantibody markers in type 1 diabetes. Diabetes 51:1346–1355
Notkins AL, Lernmark Å (2002) Autoimmune type 1 diabetes: resolved and unresolved issues. J Clin Invest 108:1247–1252
Krischer JP, Cuthbertson DD, Yu L et al (2003) Screening strategies for the identification of multiple antibody-positive relatives of individuals with type 1 diabetes. J Clin Endocrinol Metab 88:103–108
Falorni A, Brozzetti A (2005) Diabetes-related antibodies in adult diabetic patients. Best Pract Res Clin Endocrinol Metab 19:119–133
Tuomi T, Carlsson A, Li H et al (1999) Clinical and genetic characteristics of type 2 diabetes with and without GAD antibodies. Diabetes 48:150–157
Agardh C-D, Cilio CM, Lethagen ÅL et al (2005) Clinical evidence for the safety of GAD65 immunomodulation in adult-onset autoimmune diabetes. J Diabetes Complications 19:238–246
Lethagen ÅL, Ericsson UB, Hallengren B, Groop L, Tuomi T (2002) Glutamic acid decarboxylase antibody positivity is associated with an impaired insulin response to glucose and arginine in nondiabetic patients with autoimmune thyroiditis. J Clin Endocrinol Metab 87:1177–1183
Bingley PJ, Bonifacio E, Mueller PW (2003) Diabetes Antibody Standardization Program: first assay proficiency evaluation. Diabetes 52:1128–1136
Park YS, Wang CY, Ko KW et al (1998) Combinations of HLA DR and DQ molecules determine the susceptibility to insulin-dependent diabetes mellitus in Koreans. Hum Immunol 59:794–780
Brown P, Rothwell JC, Marsden CD (1997) The stiff leg syndrome. J Neurol Neurosurg Psychiatr 62:31–37
Barker RA, Revesz T, Thom M, Marsden CD, Brown P (1998) Review of 23 patients affected by the stiff man syndrome, stiff limb syndrome, and progressive encephalomyelitis with rigidity. J Neurol Neurosurg Psyciatr 65:640–663
Smith GE, Summers MD, Fraser MJ (1983) Production of human beta interferon in insect cells infected with baculovirus expression vector. Mol Cell Biol 3:2156–2165
Zimmet PZ, Tuomi T, Mackay IR et al (1994) Latent autoimmune diabetes mellitus in adults (LADA): the role of antibodies to glutamic acid decarboxylase in diagnosis and prediction of insulin dependency. Diabet Med 11:299–303
Turner R, Stratton I, Horton V et al (1997) Autoantibodies to islet-cell cytoplasm and glutamic acid decarboxylase for prediction of insulin requirement in type 2 diabetes. UK Prospective Diabetes Study (UKPDS). Lancet 350:1288–1293
Palmer J (2000) Therapeutic importance of subset of type 2 diabetes. Diabetes Care 23:574–575
Acknowledgements
Å. Lernmark was supported by the National Institutes of Health (grant numbers DK26190 and DK53004) and the Swedish Research Council (grant number 72X-14064). Diamyd Therapeutics, Stockholm, Sweden supported the study. The authors appreciate the technical support provided by G. Ahlqvist, H. Söderling, A. Kastensson, A. Nilsson, J. Ljungberg, C. Brundin and J. Arvastsson (all at the Department of Clinical Sciences, Lund University, University Hospital MAS, Malmö, Sweden).
Duality of interest
K. F. Lynch previously provided statistical assistance for Diamyd Medical. The other authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
ESM Table 1
(PDF 42.7 kb)
ESM Table 2
(PDF 42.2 kb)
ESM Fig. 1
(PDF 13 kb)
Rights and permissions
About this article
Cite this article
Agardh, CD., Lynch, K.F., Palmér, M. et al. GAD65 vaccination: 5 years of follow-up in a randomised dose-escalating study in adult-onset autoimmune diabetes. Diabetologia 52, 1363–1368 (2009). https://doi.org/10.1007/s00125-009-1371-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-009-1371-2