Abstract
Aims/hypothesis
The nuclear receptors, including nuclear receptor subfamily 1, group H, member 3 (NR1HR, also known as liver X receptor [LXR]), are sensors of cholesterol metabolism and lipid biosynthesis that have recently been proposed as insulin sensitisers. TNFα has been described as a link between obesity and the development of insulin resistance, an important contributor to the pathogenesis of type 2 diabetes. Therefore, we decided to investigate the ability of NR1HR agonists to ameliorate TNFα-induced insulin resistance in brown adipocytes.
Methods
Primary brown adipocytes from rat fetuses, and from wild-type neonate mice and neonate mice deficient in the gene encoding protein tyrosine phosphatase-1B (Ptpn1, also known as Ptp1b) were cultured in the absence or presence of TNFα and different nuclear receptor agonists. Among them, the unrelated NR1HR ligands T0901317, GW3965 and (22R)-hydroxycholesterol were tested. After insulin stimulation, glucose uptake and solute carrier family 2 (facilitated glucose transporter), member 4 (SLC2A4, formerly known as GLUT4) translocation were measured. Next the insulin signalling cascade was determined by submitting cells to lysis, immunoprecipitation and immunoblotting.
Results
NR1HR agonists ameliorate TNFα-induced insulin resistance restoring completely insulin-stimulated glucose uptake and SLC2A4 translocation to plasma membrane. This effect is parallel to the recovery of the insulin cascade insulin receptor/IRS-2/phosphatidylinositol 3-kinase/protein kinase B, and could be due to the fact that T0901317 prevents the increase of PTPN1 production and phosphatase activity produced by TNFα. In this regard, Ptpn1-deficient brown adipocytes showed protection against insulin resistance by TNFα. Moreover, we observed that T0901317 produced in itself a significant increase over basal glucose uptake consistent with an increase of SLC2A4 protein content in plasma membrane, attributable to the activation of protein kinase ζ and/or the increase of Slc2a4 expression.
Conclusions/interpretation
Nuclear receptors NR1HR are interesting potential targets for drug treatment of insulin resistance.
Similar content being viewed by others
Introduction
Nuclear receptors such as retinoic acid receptor (RAR), peroxisome proliferator activated receptors (PPARs) and the orphan receptor nuclear receptor subfamily 1, group H, member 3 (NR1HR, also known as liver X receptor [LXR]) comprise a superfamily of related proteins, which act as transcription factors to activate expression of target genes in response to binding of ligands. These proteins bind preferentially to DNA as heterodimers with a common partner, retinoid X receptor (RXR), to regulate transcription. NR1HRs are activated by naturally produced oxysterols, including (22R)-hydroxycholesterol, (24,25S)-epoxycholesterol, and 27-hydroxycholesterol, as well as by synthetic compounds such as T0901317 and GW3965 [1, 2]. Although NR1HR function has been elucidated in detail with respect to cholesterol and lipid metabolism, new findings have indicated that NR1HR is an important regulator of glucose metabolism in liver and adipose tissue [3–5]. Recent studies have reported low plasma glucose, improved glucose tolerance and increased glucose-induced insulin secretion by islets in genetic and dietary models of type 2 diabetes treated with synthetic NR1HR agonists [6–8].
Several sources of evidence suggest that NR1HR activity may be important in adipocytes. First, NR1HRα and β are abundantly produced in adipocytes, preferentially in subcutaneous rather than in visceral white adipose tissue [9]. In addition, NR1HR production is regulated by the key adipocyte transcription factor PPARγ either in macrophages and in adipose tissue, and many NR1HR target genes are also highly expressed in adipocytes [10–12]. Moreover, ligand activation of NR1HR regulates production of the insulin-responsive glucose transporter solute carrier family 2 (facilitated glucose transporter), member 4 (SLC2A4, formerly known as GLUT4) both in vivo and in murine and human adipocytes, through direct interaction with a conserved NR1HR response element in the Slc2a4 promoter. By contrast, the ability of NR1HR ligands to regulate SLC2A4 production was abolished in mice lacking Nr1h3 [8, 13].
Although white adipose tissue is the main adipose tissue, brown adipose tissue, in which glucose is an important fuel in vivo, is also present in small mammals. Brown adipose tissue is a target tissue for insulin action, especially during late fetal development, when insulin promotes adipogenic and thermogenic differentiation and regulates glucose uptake, as reviewed [14]. Acute insulin treatment stimulates glucose transport in fetal brown adipocytes largely by mediating translocation of SLC2A4 to the plasma membrane, a process involving the activation of phosphatidylinositol (PI) 3-kinase, protein kinase B (PKB) and protein kinase C (PKC)ζ [15, 16]. Brown adipose tissue is also a target for nuclear receptor agonists, since it produces abundant PPARγ, NR1HRα and β [9, 17]. In this regard, the PPARγ agonist rosiglitazone up-regulates the expression of the lipoprotein lipase, hormone-sensitive lipase and uncoupling protein-1 genes in brown adipocytes [18], as well as achieving insulin sensitisation by increasing the Tyr kinase activity of the insulin receptor [19]. So far, the effect of activation of NR1HRs on glucose metabolism in brown adipocytes has not been explored.
Several factors secreted from adipose tissue, including cytokines, growth factors and NEFA, can produce insulin resistance by impairing insulin signalling. Among them, TNFα has been proposed as a link between adiposity and the development of insulin resistance, an important contributor to the pathogenesis of type 2 diabetes [20, 21]. In this regard, we had previously described that TNFα caused insulin resistance in brown adipocytes by impairing insulin signalling at the level of IRS-2. We had also identified ceramide production and activation of protein phosphatase 2A (PP2A), and induction of p38 and p42/p44 mitogen-activated protein kinase (MAPK) as mediators of insulin resistance by TNFα [22, 23]. Moreover, the thiazolidinedione rosiglitazone ameliorates TNFα-induced insulin resistance in brown adipocytes by impairing the stimulation of MAPKs by TNFα [22]. Thiazolidinediones are insulin-sensitising drugs, which improve insulin action in vivo across a wide spectrum of insulin-resistant states and which have recently been introduced for the clinical treatment of type 2 diabetes [24, 25]. However, several limitations of this therapy, such as increased adiposity, secondary insulin resistance in white adipose tissue, and pro- and anti-atherogenic effects, have now emerged [24, 25]. The fact that fetal brown adipocytes represent an ideal system for investigating the effectiveness of therapeutic agents in the treatment of insulin resistance prompted us to evaluate the potential role of the nuclear receptor NR1HR in alleviating TNFα-induced insulin resistance.
Materials and methods
Materials
Insulin, 4-[(E)-2-(5,6,7,8,-tetrahydro-5,5,8,8-tetramethyl-2-naphthalenyl)-1-propenyl]benzoic acid (TTNPB), phytanic acid, (22R)-hydroxycholesterol and (22S)-hydroxycholesterol were from Sigma (St Louis, MO, USA). TNFα was purchased from Prepotech (London, UK) and T0901317 from Cayman Chemical (Ann Arbor, MI, USA). 2-Deoxy-d-[1-3H]glucose and γ-32P-labelled ATP were purchased from Amersham Biosciences (Aylesbury, UK). Antibodies against solute carrier family 2 (facilitated glucose transporter), member 1 (SLC2A1) and SLC2A4 were supplied by Chemicon (Temecula, CA, USA). Antibodies against phosphorylated or total PKB, extracellular signal-regulated kinase (ERK)1/2 and PKCζ were from Cell Signaling (Beverly, MA, USA). Antibodies against IRS-2, P-Tyr, protein tyrosine phosphatase 1B (PTPN1, also known as PTP1B), PP2A and SH-2 containing inositol 5′-phosphatase (SHIP)2 were from Upstate Biotechnology (Lake Placid, NY, USA). Antibodies against caveolin-1 (sc-894), insulin receptor (sc-09) and anti-phosphatase and tensin homolog deleted on chromosome 10 (PTEN) (sc-7974) were from Santa Cruz (Palo Alto, CA, USA). All other reagents used were of the purest grade available.
Animals and cell culture
Wistar rats were obtained from the Complutense University Animal House. Ptpn1-deficient and wild-type mice were from Abbott Laboratories (Abbott Park, IL, USA). The principles of laboratory animal care were followed and the study was approved by the local ethics committee and carried out in accordance with the Federation of European Laboratory Animal Science.
Fetal brown adipocytes were obtained from interscapular brown adipose tissue of Wistar rat fetuses (20 days old) or Ptpn1-deficient and wild-type mice neonates (5 days old). Cells were isolated by collagenase dispersion, and plated in minimal essential medium with Earle’s salts supplemented with 10% fetal serum, as previously described [23]. After 4 h of culture at 37°C, cells were rinsed twice with PBS and a 70% confluent monolayer was observed under inverse light microscopy. Cells were maintained for 20 h in a serum-free medium supplemented with 0.2% (w/v) BSA and then cultured for 24 h in the absence or presence of 2 nmol/l TNFα with or without nuclear receptor agonists. The cells were then stimulated or not for 5 or 30 min with 10 nmol/l insulin.
Glucose transport determination
Glucose uptake was measured by incorporating 2-deoxy-d-[1-3H]glucose into cells during the last 10 min of culture as described previously [15]. Results are expressed as pmol glucose mg protein−1 10 min−1.
Subcellular fractionation
Cells were submitted to subcellular fractionation for plasma membrane fraction isolation, before protein quantification and western blotting with SLC2A4, SLC2A1 and caveolin-1 antibodies as previously described [23].
Immunoprecipitations
Cells were extracted with lysis buffer I containing: 10 mmol/l Tris–HCl, 5 mmol/l EDTA, 50 mmol/l NaCl, 30 mmol/l sodium pyrophosphate, 50 mmol/l NaF, 100 μmol/l Na3VO4, 1% Triton X-100, and 1 mmol/l phenylmethylsulfonyl fluoride (pH 7.6). After protein content determination, equal amounts of protein were immunoprecipitated at 4°C with the corresponding antibody. The immune complexes were collected on protein A-agarose and analysed on SDS-PAGE followed by western blotting or on PI3-kinase activity by in vitro phosphorylation of phosphatidylinositol as previously described [22].
PTPN1 activity
Cells were cultured in a phosphate-free MEM medium and lysed in lysis buffer containing: 50 mmol/l Tris, 150 mmol/l NaCl, 1% Triton X-100, 2 mmol/l EDTA (pH 7.5). PTPN1 activity was assessed by malachite green and p-nitrophenyl phosphate hydrolysis assays by dephosphorylation of specific phosphopeptides (Upstate Biotechnology) as previously described by us [19].
Western blotting
Proteins were submitted to SDS-PAGE, transferred to Immobilon membranes (Millipore, Bedford, MA, USA), blocked using 5% non-fat dried milk in 10 mmol/l Tris–HCl and 150 mmol/l NaCl (pH 7.5), and were then incubated overnight with several antibodies in 0.05% Tween-20, 1% non-fat dried milk in the same buffer. Blots were exposed to high-sensitivity films and developed using the enhanced chemiluminescence system (Amersham Biosciences).
Northern blotting
RNA was isolated and submitted to northern blot analysis as described previously [26]. Serial hybridisation with Slc2a4 and Slc2a1 probes was done before a final hybridisation with the 18S rRNA probe.
Real-time quantitative RT-PCR assays
DNAse I treated RNA was reverse transcribed into cDNA before performing the PCR assay for Slc2a4 and Ptpn1 gene expression using gene expression assays (Taqman; Applied Biosystems, Foster City, CA, USA), as previously described [26]. The results are given as percentage over control (untreated cells) after normalising mRNA to 18S rRNA expression.
Data analysis
Results are presented as means ± SEM from three to five independent experiments. Statistical significance was tested by one-way analysis of variance, followed by the protected least-significant different test. p values less than 0.01 were considered significant. In experiments using X-ray films (Hyperfilm), different exposure times were used to ensure that bands were not saturated.
Results
Nuclear receptor NR1HR agonists regulate glucose uptake in brown adipocytes under physiological and insulin-resistant conditions
In order to investigate the impact of nuclear receptor activation on glucose uptake, rat fetal brown adipocytes were cultured for 24 h in the absence or presence of different nuclear receptor agonists, prior to stimulation for 30 min with 10 nmol/l insulin, after which glucose uptake was determined (Fig. 1a). We used the following dosages: rosiglitazone as PPARγ agonist, 10 μmol/l, a dose previously used in brown adipocytes [19]; TTNPB as RAR agonist, 10 μmol/l; and phytanic acid as RXR agonist, 20 μmol/l. The latter two doses are similar to those used in other studies in vitro [27]. To activate NR1HR we tested the synthetic compounds T0901317 and GW3965 at the optimal doses of 3 and 15 μmol/l, respectively, calculated from dose–response experiments (Fig. 1b), as well as the natural ligand (22R)-hydroxycholesterol at 100 μmol/l, a dose 20 times higher than its EC50 [28], using (22S)-hydroxycholesterol (100 μmol/l) as a negative control (Fig. 1a). The non-steroid NR1HR ligands T0901317 and GW3965 both produced a significant increase (50%) over basal glucose uptake, a level of stimulation slightly higher than that produced by (22R)-hydroxycholesterol (40%). An increase over basal glucose uptake was also observed in cells treated with rosiglitazone (55%), but not in those treated with TTNB or phytanic acid. Stimulation with insulin increased glucose uptake by 2.5-fold, as expected [15]. Insulin sensitisation on glucose uptake was only observed when cells were treated with rosiglitazone, but not when they were treated with NR1HR ligands, TTNPB or phytanic acid.
Effect of different nuclear receptor agonists on glucose uptake in rat brown adipocytes under physiological and insulin-resistant conditions. a Rat fetal brown adipocytes were cultured for 24 h either in the absence or presence of different nuclear receptor agonists and stimulated or not with 10 nmol/l insulin (Ins) for 30 min. The ligands used were rosiglitazone (Rosi; 10 μmol/l) as PPARγ agonist; TTNPB (20 μmol/l) as RAR agonist; phytanic acid (PA; 20 μmol/l) as RXR agonist; T0901317 (T1317; 3 μmol/l), GW3965 (15 μmol/l) and (22R)-hydroxycholesterol [(22R)-OH; 100 μmol/l] as NR1HR agonists. (22S)-hydroxycholesterol [(22S)-OH; 100 μmol/l] was used as negative control of NR1HR activation. b Brown adipocytes were cultured for 24 h with different doses of T0901317 or GW3965. Control cells were maintained in the absence of NR1HR agonists. c Cells were cultured for 24 h either in the absence or presence of 2 nmol/l TNFα and/or the different nuclear receptor agonists described above, and stimulated or not for 30 min with Ins. Glucose uptake was measured during the last 10 min by incorporation of 2-deoxy-D-[1-3H]glucose into the cells. Results are the mean ± SEM of triplicate measurements made in three to five independent cultures. *p < 0.01 for differences vs control; Δ p < 0.01 for difference vs Ins; ♦p < 0.01 for difference vs TNFα plus Ins
The fact that TNFα induces insulin resistance in brown adipocytes [23] prompted us to investigate whether nuclear receptor agonists can restore glucose uptake under these conditions. Cells were cultured in the absence or presence of 2 nmol/l TNFα with or without nuclear receptor ligands, prior to stimulation for 30 min with insulin. As shown in Fig. 1c, the three NR1HR agonists tested (T0901317, GW3965, (22R)-hydroxycholesterol) and the RAR agonist TTNPB completely restored insulin-stimulated glucose uptake in the presence of TNFα, in a similar fashion to rosiglitazone. Nevertheless, neither phytanic acid nor (22S)-hydroxycholesterol treatment impaired TNFα-induced insulin resistance upon glucose uptake. According to these results, we decided to focus our studies on the effects of NR1HR, using T0901317 as agonist.
To correlate the data on glucose uptake with SLC2A4 translocation to the plasma membrane, subcellular fractionation was performed and SLC2A4 protein was detected (Fig. 2a,b). Incubation of brown adipocytes with insulin for 30 min or with T0901317 for 24 h increased SLC2A4 protein content in plasma membrane (200% and 50%, respectively), which is consistent with the data on glucose uptake. In addition, the redistribution of SLC2A4 in the presence of insulin was precluded after TNFα treatment for 24 h, in agreement with our previous work [22]. Moreover, in these TNFα-induced insulin-resistant conditions pretreatment with T0901317 completely restored SLC2A4 translocation by insulin. No sensitising effect of T0901317 was observed either on insulin-stimulated SLC2A4 translocation (Fig. 2a,b) or on glucose uptake (Fig. 1a). Regarding production of the ubiquitous glucose transporter SLC2A1, we confirmed that TNFα increased SLC2A1 protein content at the plasma membrane (Fig. 2a,c), contributing to the increase observed in basal glucose uptake [22]. However, the NR1HR agonist did not modify SLC2A1 levels. Caveolin-1, used as a marker protein of the plasma membrane, remained essentially unaltered under the different treatments. The increase in glucose uptake and in SLC2A4 protein amount on plasma membrane detected in the presence of T0901317 led us to investigate whether this NR1HR agonist might regulate total SLC2A4 production in brown adipose tissue, as already reported for epididymal white adipose tissue [13]. Brown adipocytes, after treatment for 24 with T0901317, showed a 2.5-fold increase in the amount of Slc2a4 mRNA detected either by real-time quantitative RT-PCR (Fig. 2d) or northern blot (Fig. 2e). Moreover, double the amount of total SLC2A4 protein was observed under treatment with T0901317 (Fig. 2f). However, treatment with T0901317 did not affect Slc2a1 mRNA or protein content (Fig. 2e,f).
T0901317 induces SLC2A4 translocation to plasma membrane under basal and insulin-resistant conditions. a–c Rat fetal brown adipocytes were cultured for 24 h either in the absence or presence of TNFα and/or T0901317 (T1317) prior to stimulation for 30 min with insulin (Ins), at the doses described in Fig. 1. Cells were collected and submitted to subcellular fractionation. Plasma membrane proteins (10 μg) were subjected to SDS-PAGE and analysed by western blotting with antibodies against SLC2A4, SLC2A1 and caveolin-1. Representative immunoblots (a) and densitometric analysis (b, c) of three independent experiments are shown. Statistical significance, see Fig. 1. d Brown adipocytes were cultured for 24 h in the absence or presence of 3 μmol/l T0901317. Total RNA (1 μg) was submitted to real-time quantitative RT-PCR, and data are expressed as percentage over the mRNA detected from untreated cells (100%). Results are means ± SEM of three independent experiments; statistical analysis, see Fig. 1c. e Total RNA (10 μg) was submitted to northern blot analysis and hybridised with labelled Slc2a4 and Slc2a1 cDNAs. A final hybridisation with the 18S rRNA cDNA was performed for normalisation. f Total protein (30 μg) was submitted to western blotting with anti-SLC2A4 and anti-SLC2A1 antibodies. β-Actin was used as loading control. Representative autoradiograms are shown
T0901317 ameliorates the insulin resistance induced by TNFα by restoring the insulin signalling cascade in brown adipocytes
Since TNFα interferes with the insulin signalling cascade at the level of IRS-2/PI3-kinase/PKB in brown adipocytes [23], we analysed at which molecular level T0901317 acts to normalise glucose uptake. The initial steps within the insulin cascade were determined in Fig. 3. Insulin induced Tyr phosphorylation of insulin receptor β-chain and IRS-2, an effect that was impaired by pretreatment with TNFα. However, when cells were cultured in the presence of T0901317 and TNFα, phosphorylation of the insulin receptor by insulin was almost normalised (Fig. 3a,b). Moreover, T0901317 completely restored insulin-stimulated IRS-2 Tyr phosphorylation in the presence of TNFα (Fig. 3a,c). No significant effect was observed between cells treated with T0901317 plus insulin and those treated with insulin. In addition, TNFα impaired insulin-induced PI3-kinase activity in IRS-2 immunoprecipitates, but this inhibitory effect was not produced in the presence of T0901317 (Fig. 3a,d). TNFα has a smaller inhibitory effect on insulin signalling at the level of IRS-1 than that of IRS-2, its phosphorylation and PI3-kinase-associated activity being completely normalised after treatments with T0901317 (data not shown).
T0901317 restores insulin receptor/IRS-2/ phosphatidylinositol 3-kinase cascade in the presence of TNFα. Rat fetal brown adipocytes were cultured for 24 h either in the absence or presence of TNFα and/or T0901317 (T1317) and stimulated or not for 5 min with insulin (Ins) at the doses described in Fig. 1. Cells were lysed and total protein (1 mg) was immunoprecipitated with anti-insulin receptor (IR) β-chain or anti-IRS-2 antibodies. The resulting immune complexes were analysed (a) by western blot with antibodies against protein Tyr (P-Tyr), IR or IRS-2. Cell lysates of IRS-2 immunoprecipitates were used for an in vitro phosphatidylinositol (PI)3-kinase activity assay. The conversion of PI to PI phosphate (PIP) in the presence of γ32-P-labelled ATP was analysed by thin layer chromatography. The autoradiograms were quantified by scanning densitometry. The results shown are representative of at least three independent experiments. Histograms from densitometric analysis (b–d) are the mean ± SEM. For details of statistical significance, see Fig. 1
Next, we investigated in the downstream PI3-kinase pathways the role of PKB and PKCζ, which have been proposed to mediate glucose uptake in brown adipocytes [15, 16], as shown in Fig. 4. Insulin produced phosphorylation of PKB at both regulatory residues Ser 473 and Thr 308, an effect that was impaired in the presence of TNFα (Fig. 4a,b). Accordingly, we observed that T0901317 restored insulin stimulation of PKB phosphorylation in the presence of TNFα in parallel to the insulin cascade IRS-2/PI 3-kinase. In the presence of the cytokine, we detected an inhibitory effect of the PKCζ phosphorylation induced by insulin; this effect was not reversed by T0901317 (Fig. 4a,c). However, this compound produced in itself a significant level of PKCζ phosphorylation, which might be responsible for the stimulation on glucose uptake and SLC2A4 translocation observed in Figs. 1 and 2a,b, respectively. Finally, we also analysed (Fig. 4a,d) the modulation of the insulin ERK1/2 pathway. TNFα did not modify insulin-induced ERK1/2 phosphorylation although we detected some activation of ERK1/2 by T0901317.
T0901317 allows insulin activation of PKB in the presence of TNFα. Rat fetal brown adipocytes were cultured as in Fig. 3. Cells were lysed and total protein (30 μg) was submitted to western blotting (a) with antibodies against phosphorylated (P) or total PKB, ERK1/2 and PKCζ. The immunoblots shown are representative of at least three independent experiments. Histograms (b–d) from densitometric analysis are the mean ± SEM from three independent experiments. For details of statistical significance, see Fig. 1
T09013127 downregulates the PTPN1 protein production induced by TNFα
The fact that NR1HR activation ameliorates insulin resistance by restoring the insulin receptor/IRS-2/PI3-kinase/PKB cascade suggests that TNFα and T0901317 might modulate insulin signalling by alternating production and/or activity of some phosphatase. In this regard, we decided to explore the expression of PTPN1, as well as of such other lipid and Ser/Thr phosphatases as SHIP2, PTEN or PP2A, all known to be present in brown adipocytes [19]. Therefore, cells were cultured in the absence or presence of TNFα with or without T0910317 for 24 h, and different phosphatases were analysed by western blot (Fig. 5a). Treatment of brown adipocytes with TNFα significantly increased PTPN1 protein production, but cotreatment with T0901317 prevented this increase. However, the amount of SHIP2, PTEN or PP2A remained unaltered. Subsequently we measured PTPN1 activity (Fig. 5b) and found it to be increased in brown adipocytes treated with TNFα, in line with the increase in PTPN1 protein production. Moreover, this increase in phosphatase activity was prevented by treatment with T0901317. In order to investigate whether this regulation of PTPN1 protein was the consequence of changes at the mRNA level we analysed mRNA expression by real-time quantitative RT-PCR (Fig. 5c). The accumulation of Ptpn1 mRNA induced by TNFα was not detected in the presence of the NR1HR ligand.
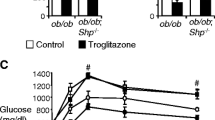
T0901317 prevents the modulation of PTPN1 induced by TNFα in murine brown adipocytes. Rat fetal brown adipocytes were cultured for 24 h with 2 nmol/l TNFα and/or 3 μmol/l T0901317 (T1317). a PTPN1, SHIP2, PP2A and PTEN protein content were monitored by western blotting, using β-actin as loading control. Representative immunoblots of three independent experiments are shown. b PTPN1 activity was measured at the end of culture time. Results are the mean ± SEM from three independent experiments. Data are expressed as a percentage of stimulation of phosphatase activity compared with control cells. *p < 0.01 for difference vs control; Δp < 0.01 for difference vs. TNFα. c Total RNA (1 μg) was submitted to real-time quantitative RT-PCR. Data are expressed as percentage over the mRNA detected from untreated cells (100%). Statistical significance as above (b). d Primary cultures of neonatal brown adipocytes were obtained from wild-type and Ptpn1-deficient mice. Cells were cultured for 24 h with 2 nmol/l TNFα prior to stimulation or not for 30 min with 10 nmol/l insulin (Ins). Glucose uptake was measured during the last 10 min of culture by incorporation of labelled 2-deoxy-glucose. Results are expressed as percentage of stimulation over basal glucose uptake in the absence of insulin, and are the mean ± SEM of triplicate measurements made in three independent cultures. Δp < 0.01 for difference between TNFα plus insulin versus insulin alone. e Mouse neonatal brown adipocytes were cultured with TNFα prior to stimulation for 5 min with insulin. Cells were lysed and total protein (30 μg) was submitted to western blotting and immunodetected with antibodies against phosphorylated (P) or total PKB and PTPN1. Representative immunoblots from three independent experiments are shown
Since TNFα increased PTPN1 content, we decided to explore whether lack of PTPN1 might confer protection against TNFα-induced insulin resistance (Fig. 5d). Primary cultures of brown adipocytes from Ptpn1-deficient mice neonates and from the corresponding wild-type neonates were grown, and cells were then cultured with TNFα prior to stimulation with insulin. When glucose uptake was determined, insulin fully stimulated glucose uptake in Ptpn1-deficient cells regardless of whether TNFα was present (Fig. 5d), an effect that was not produced in wild-type mice brown adipocytes in accordance with data on rat brown adipocytes (Fig. 1c). Moreover, the increase in PTPN1 protein that was induced by TNFα in rat brown adipocytes was also detected in wild-type mice brown adipocytes (Fig. 5e). Lack of PTPN1 protected against impairment of insulin activation of PKB by TNFα (Fig. 5e), in agreement with the observed protection against insulin resistance on glucose uptake.
Discussion
The close association between obesity and insulin resistance and their progression to type 2 diabetes is a severe health problem. In recent years our laboratory has established that fetal brown adipocytes constitute an ideal system for studying molecular mechanisms of insulin resistance and for testing novel approaches to overcome or bypass such resistance. One such approach is ligand activation of nuclear receptors, which can regulate glucose metabolism in multiple tissues including adipose tissue [3–5]. Accordingly, we decided to explore and compare the effect of nuclear receptor agonists on glucose uptake in brown adipocytes. Thus, this study has revealed that PPARγ-, NR1HR-, RAR- and RXR- selective agonists differ in their effects. We observed, for the first time, that the synthetic NR1HR agonists T0901317 and GW3965 increased basal glucose uptake in brown adipocytes and, more importantly, restored insulin-stimulated glucose uptake in insulin-resistant conditions such as the presence of TNFα. Another NR1HR agonist, the natural ligand (22R)-hydroxycholesterol, also ameliorates TNFα-induced insulin resistance on glucose uptake, while the negative control (22S)-hydroxycholesterol does not. The fact that three unrelated ligands produced similar restoration of glucose uptake seems to indicate that their effects are dependent on NR1HR. Moreover, RAR activation also restored insulin sensitivity in the presence of the cytokine, while the PPARγ agonist rosiglitazone stimulated glucose uptake under basal conditions and produced insulin sensitisation regardless of whether TNFα was present or not, in agreement with previous findings in this cellular model [19, 22]. In contrast, RXR activation failed to regulate glucose uptake in all the experimental conditions tested. These results indicate that the effect on glucose uptake is not due to RXR activation, the common partner of these nuclear receptors. The differences between these nuclear receptors have been previously observed, for instance, adipogenesis was inhibited by an RAR-mediated event [29, 30], whereas RXR-specific agonists promoted adipocyte differentiation [27].
In this work we found that NR1HR agonists increased basal glucose uptake in brown adipocytes in a dose-dependent manner, in agreement with the results obtained in 3T3-L1 adipocytes [8]. This effect is the result of changes of SLC2A4 in the plasma membrane, and could be attributed to the activation of PKCζ and/or the increase in Slc2a4 expression produced by T0901317. It is well known that the biological effects of nuclear receptors are characterised by nuclear transcriptional regulation of gene expression as well as non-genomic effects. We have recently proposed that rosiglitazone activates basal glucose uptake in a manner dependent on p38MAPK [19], and in some cellular systems PKC phosphorylation has been found to be increased by other nuclear receptor agonists such as vitamin D analogues [31]. The effect of NR1HR agonists on Slc2a4 expression in rat brown adipocytes is in agreement with the up-regulation of Slc2a4 detected in murine and human adipocytes, where the Slc2a4 promoter is a direct transcriptional target for the NR1HR/RXR heterodimer [8, 13]. On the other hand, T0901317 treatment did not produce insulin sensitisation, either on glucose uptake, or in the insulin signalling cascade, an effect clearly different from that observed for rosiglitazone in our previous work [19] and in studies performed in murine adipocytes [8]. Differential effects of pharmacological NR1HR activation on insulin sensitivity in normal or insulin-resistant conditions have also been detected in other studies. For instance, NR1HR agonists lowered blood glucose levels and improved whole-body insulin sensitivity in ob/ob mice, but not in lean mice [32]. However, recent studies have shown that NR1HR agonists may lead to increased utilisation of lipids and glucose in human skeletal muscle cells, without affecting the mechanism of action of insulin [33].
This is the first time that the ability of NR1HR agonists to ameliorate the insulin resistance induced by TNFα has been documented. We found that chronic exposure to T0901317 completely restored insulin-induced glucose uptake and SLC2A4 translocation in the presence of TNFα. This effect is parallel to the recovery of the insulin cascade insulin receptor/IRS-2/PI3-kinase/PKB, as observed previously in the case of rosiglitazone [22]. However, another insulin pathway, namely that involving PKCζ, is also involved in translocation of SLC2A4 [16]; it was inhibited in the presence of TNFα, but was not restored by T0901317. Accordingly, synthetic NR1HR agonists have been reported to improve glucose tolerance in genetic and dietary models of type 2 diabetes [6, 8] and to increase glucose-induced insulin secretion by islets [7], very similar effects to those elicited by thiazolidinediones [34] and synthetic activators of RXR [35]. Moreover, NR1HR agonist treatment suppresses hepatic gluconeogenesis [6], inhibits synthesis of proinflammatory cytokines [36] and induces desirable changes in cholesterol metabolism [37], favourable features for a potential drug against diabetes.
The fact that NR1HR activation ameliorates insulin resistance by restoring the insulin receptor/IRS-2 cascade suggests that TNFα and T0901317 might modulate insulin signalling by altering the activity of some phosphatase. In this work we detected for the first time a significant enlargement of Ptpn1 mRNA and protein expression in brown adipocytes treated with TNFα, as well as an increase in phosphatase activity. Numerous sources of evidence suggest that phosphatases are used by TNFα to block insulin signalling at different levels [38–40]. Moreover, studies with obese rats have shown that expression of leucocyte common antigen-related protein tyrosine phosphatase in liver is downregulated after TNFα blockade [41], and in rat hepatoma cells TNFα increased SHIP2 production. Overactivation of phosphatases is one way in which insulin signalling becomes blocked, and PTPN1, which dephosphorylates the activated insulin receptors and their substrates, has been shown to play a major role in both insulin resistance and type 2 diabetes [42, 43]. We therefore decided to check whether lack of PTPN1 in brown adipocytes might confer protection against TNFα-induced insulin resistance. As expected, TNFα did not produce insulin resistance, either on glucose uptake, or in insulin signalling in Ptpn1-deficient primary brown adipocytes. This novel finding indicates that part at least of the effects of TNFα may be exerted through the dynamic modulation of PTPN1 production. Moreover, the increase in PTPN1 production and activity induced by TNFα was completely prevented by T0901317. The mechanisms of this inhibitory action are unknown, and so far no NR1HR response elements have being identified on the Ptpn1 promoter, although the induction by cytokines of the expression of other genes, such as that encoding matrix metalloproteinase-9 in macrophages, was repressed by NR1HR activation [44]. One group has identified on the Ptpn1 promoter two regulatory elements that recognise Y box-binding protein-1 and Sp family transcription factors, both of which are required for optimal promoter activity [45]. Whether or not NR1HR can modulate the expression of these transcription factors or compete with them for recruitment of activators and repressors remains to be established. Similar results have been reported with different PTPs in other cell systems. Thus, production of LAR in liver is up-regulated by a high-fat diet and profoundly downregulated by PPARα agonists [46]. Increased availability of NEFA has also been shown to promote the production of PTPN1, as well as insulin resistance in rat skeletal muscle and hepatic cells [47]. Moreover, recent studies with diabetic rats have demonstrated enhanced levels and activities of PTPN1 in skeletal muscle and liver whereas rosiglitazone treatment decreases this increase in muscle but not in liver [48]. Accordingly, modulation of genes such as that encoding PTPN1 might contribute to the pathogenesis of TNFα-induced insulin resistance in brown adipocytes. In agreement with our previous results, this cytokine induces insulin resistance through multiple mechanisms: decrease of IRS-2 Tyr phosphorylation through a MAPK-dependent mechanism [22], generation of ceramide and activation of PP2A [23], and modulation of PTPN1 protein production and activity (this study).
In conclusion, the synthetic NR1HR agonist T0901317 ameliorates TNFα-induced insulin resistance in brown adipocytes restoring completely insulin-stimulated glucose uptake possibly by ameliorating abnormal levels of PTPN1. These new results support the hypothesis that nuclear receptor NR1HR is an interesting target for drug treatment of insulin resistance.
Abbreviations
- PKB:
-
protein kinase B
- ERK:
-
extracellular signal-regulated kinase
- IRS:
-
IR substrate
- MAPK:
-
mitogen-activated protein kinase
- NR1HR:
-
nuclear receptor subfamily 1, group H, member 3 (also known as liver X receptor [LXR])
- PI:
-
phosphatidylinositol
- PKC:
-
protein kinase C
- PP2A:
-
protein phosphatase 2A
- PPAR:
-
peroxisome proliferator-activated receptor
- PTEN:
-
phosphatase and tensin homolog deleted on chromosome 10
- PTPN1:
-
protein tyrosine phosphatase-1B
- RAR:
-
retinoic acid receptor
- RXR:
-
retinoid X receptor
- SHIP:
-
SH-2 containing inositol 5′-phosphatase
- SLC2A1:
-
solute carrier family 2 (facilitated glucose transporter), member 1
- SLC2A4:
-
solute carrier family 2 (facilitated glucose transporter), member 4
- TTNPB:
-
4-[(E)-2-(5,6,7,8,-tetrahydro-5,5,8,8-tetramethyl-2-naphthalenyl)-1-propenyl]benzoic acid
References
Janowski BA, Willy PJ, Devi TR, Falck JR, Mangelsdorf DJ (1996) An oxysterol signalling pathway mediated by the nuclear receptor LXR alpha. Nature 383:728–731
Schultz JR, Tu H, Luk A et al (2000) Role of LXRs in control of lipogenesis. Genes Dev 14:2831–2838
Li AC, Binder CJ, Gutierrez A et al (2004) Differential inhibition of macrophage foam-cell formation and atherosclerosis in mice by PPARalpha, beta/delta, and gamma. J Clin Invest 114:1564–1576
Steffensen KR, Gustafsson JA (2004) Putative metabolic effects of the liver X receptor (LXR). Diabetes 53(Suppl 1):S36–S42
Tontonoz P, Mangelsdorf DJ (2003) Liver X receptor signaling pathways in cardiovascular disease. Mol Endocrinol 17:985–993
Cao G, Liang Y, Broderick CL et al (2003) Antidiabetic action of a liver x receptor agonist mediated by inhibition of hepatic gluconeogenesis. J Biol Chem 278:1131–1136
Efanov AM, Sewing S, Bokvist K, Gromada J (2004) Liver X receptor activation stimulates insulin secretion via modulation of glucose and lipid metabolism in pancreatic beta-cells. Diabetes 53(Suppl 3):S75–S78
Laffitte BA, Chao LC, Li J et al (2003) Activation of liver X receptor improves glucose tolerance through coordinate regulation of glucose metabolism in liver and adipose tissue. Proc Natl Acad Sci USA 100:5419–5424
Steffensen KR, Nilsson M, Schuster GU, Stulnig TM, Dahlman-Wright K, Gustafsson JA (2003) Gene expression profiling in adipose tissue indicates different transcriptional mechanisms of liver X receptors alpha and beta, respectively. Biochem Biophys Res Commun 310:589–593
Chawla A, Boisvert WA, Lee CH et al (2001) A PPAR gamma-LXR–ABCA1 pathway in macrophages is involved in cholesterol efflux and atherogenesis. Mol Cell 7:161–171
Soukas A, Socci ND, Saatkamp BD, Novelli S, Friedman JM (2001) Distinct transcriptional profiles of adipogenesis in vivo and in vitro. J Biol Chem 276:34167–34174
Juvet LK, Andresen SM, Schuster GU et al (2003) On the role of liver X receptors in lipid accumulation in adipocytes. Mol Endocrinol 17:172–182
Dalen KT, Ulven SM, Bamberg K, Gustafsson JA, Nebb HI (2003) Expression of the insulin-responsive glucose transporter GLUT4 in adipocytes is dependent on liver X receptor alpha. J Biol Chem 278:48283–48291
Valverde AM, Benito M, Lorenzo M (2005) The brown adipose cell: a model for understanding the molecular mechanisms of insulin resistance. Acta Physiol Scand 183:59–73
Hernandez R, Teruel T, Lorenzo M (2001) Akt mediates insulin induction of glucose uptake and up-regulation of GLUT4 gene expression in brown adipocytes. FEBS Lett 494:225–231
Lorenzo M, Teruel T, Hernandez R, Kayali AG, Webster NJ (2002) PLCgamma participates in insulin stimulation of glucose uptake through activation of PKCzeta in brown adipocytes. Exp Cell Res 278:146–157
Escher P, Braissant O, Basu-Modak S, Michalik L, Wahli W, Desvergne B (2001) Rat PPARs: quantitative analysis in adult rat tissues and regulation in fasting and refeeding. Endocrinology 142:4195–4202
Teruel T, Hernandez R, Rial E, Martin-Hidalgo A, Lorenzo M (2005) Rosiglitazone up-regulates lipoprotein lipase, hormone-sensitive lipase and uncoupling protein-1, and down-regulates insulin-induced fatty acid synthase gene expression in brown adipocytes of Wistar rats. Diabetologia 48:1180–1188
Hernandez R, Teruel T, Lorenzo M (2003) Rosiglitazone produces insulin sensitisation by increasing expression of the insulin receptor and its tyrosine kinase activity in brown adipocytes. Diabetologia 46:1618–1628
Hotamisligil GS, Shargill NS, Spiegelman BM (1993) Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science 259:87–91
Hotamisligil GS (1999) Mechanisms of TNF-alpha-induced insulin resistance. Exp Clin Endocrinol Diabetes 107:119–125
Hernandez R, Teruel T, de Alvaro C, Lorenzo M (2004) Rosiglitazone ameliorates insulin resistance in brown adipocytes of Wistar rats by impairing TNF-alpha induction of p38 and p42/p44 mitogen-activated protein kinases. Diabetologia 47:1615–1624
Teruel T, Hernandez R, Lorenzo M (2001) Ceramide mediates insulin resistance by tumor necrosis factor-alpha in brown adipocytes by maintaining Akt in an inactive dephosphorylated state. Diabetes 50:2563–2571
Olefsky JM (2000) Treatment of insulin resistance with peroxisome proliferator-activated receptor gamma agonists. J Clin Invest 106:467–472
Malinowski JM, Bolesta S (2000) Rosiglitazone in the treatment of type 2 diabetes mellitus: a critical review. Clin Ther 22:1151–1168
Fernandez-Veledo S, Hernandez R, Teruel T, Mas JA, Ros M, Lorenzo M (2006) Ceramide mediates TNF-alpha-induced insulin resistance on GLUT4 gene expression in brown adipocytes. Arch Physiol Biochem 112:13–22
Schluter A, Barbera MJ, Iglesias R, Giralt M, Villarroya F (2002) Phytanic acid, a novel activator of uncoupling protein-1 gene transcription and brown adipocyte differentiation. Biochem J 362:61–69
Albers M, Blume B, Schlueter T et al (2006) A novel principle for partial agonism of liver X receptor ligands. Competitive recruitment of activators and repressors. J Biol Chem 281:4920–4930
Kamei Y, Kawada T, Mizukami J, Sugimoto E (1994) The prevention of adipose differentiation of 3T3-L1 cells caused by retinoic acid is elicited through retinoic acid receptor alpha. Life Sci 55:L307–L312
Xue JC, Schwarz EJ, Chawla A, Lazar MA (1996) Distinct stages in adipogenesis revealed by retinoid inhibition of differentiation after induction of PPARgamma. Mol Cell Biol 16:1567–1575
Wali RK, Kong J, Sitrin MD, Bissonnette M, Li YC (2003) Vitamin D receptor is not required for the rapid actions of 1,25-dihydroxyvitamin D3 to increase intracellular calcium and activate protein kinase C in mouse osteoblasts. J Cell Biochem 88:794–801
Grefhorst A, van Dijk TH, Hammer A et al (2005) Differential effects of pharmacological liver X receptor activation on hepatic and peripheral insulin sensitivity in lean and ob/ob mice. Am J Physiol Endocrinol Metab 289:E829–E838
Cozzone D, Debard C, Dif N et al (2006) Activation of liver X receptors promotes lipid accumulation but does not alter insulin action in human skeletal muscle cells. Diabetologia 49:990–999
Giannini S, Serio M, Galli A (2004) Pleiotropic effects of thiazolidinediones: taking a look beyond antidiabetic activity. J Endocrinol Invest 27:982–991
Leibowitz MD, Ardecky RJ, Boehm MF et al (2006) Biological characterization of a heterodimer-selective retinoid X receptor modulator: potential benefits for the treatment of type 2 diabetes. Endocrinology 147:1044–1053
Walcher D, Kummel A, Kehrle B et al (2006) LXR activation reduces proinflammatory cytokine expression in human CD4-positive lymphocytes. Arterioscler Thromb Vasc Biol 26:1022–1028
Bruemmer D, Law RE (2005) Liver x receptors: potential novel targets in cardiovascular diseases. Curr Drug Targets Cardiovasc Haematol Disord 5:533–540
Ahmad F, Goldstein BJ (1997) Effect of tumor necrosis factor-alpha on the phosphorylation of tyrosine kinase receptors is associated with dynamic alterations in specific protein–tyrosine phosphatases. J Cell Biochem 64:117–127
Kroder G, Bossenmaier B, Kellerer M et al (1996) Tumor necrosis factor-alpha- and hyperglycemia-induced insulin resistance. Evidence for different mechanisms and different effects on insulin signaling. J Clin Invest 97:1471–1477
Ozes ON, Akca H, Mayo LD et al (2001) A phosphatidylinositol 3-kinase/Akt/mTOR pathway mediates and PTEN antagonizes tumor necrosis factor inhibition of insulin signaling through insulin receptor substrate-1. Proc Natl Acad Sci USA 98:4640–4645
Cheung AT, Wang J, Ree D, Kolls JK, Bryer-Ash M (2000) Tumor necrosis factor-alpha induces hepatic insulin resistance in obese Zucker (fa/fa) rats via interaction of leukocyte antigen-related tyrosine phosphatase with focal adhesion kinase. Diabetes 49:810–819
Zinker BA, Rondinone CM, Trevillyan JM et al (2002) PTP1B antisense oligonucleotide lowers PTP1B protein, normalizes blood glucose, and improves insulin sensitivity in diabetic mice. Proc Natl Acad Sci USA 99:11357–11362
Gum RJ, Gaede LL, Koterski SL et al (2003) Reduction of protein tyrosine phosphatase 1B increases insulin-dependent signaling in ob/ob mice. Diabetes 52:21–28
Castrillo A, Joseph SB, Marathe C, Mangelsdorf DJ, Tontonoz P (2003) Liver X receptor-dependent repression of matrix metalloproteinase-9 expression in macrophages. J Biol Chem 278:10443–10449
Fukada T, Tonks NK (2003) Identification of YB-1 as a regulator of PTP1B expression: implications for regulation of insulin and cytokine signaling. EMBO J 22:479–493
Frederiksen KS, Wulf EM, Wassermann K, Sauerberg P, Fleckner J (2003) Identification of hepatic transcriptional changes in insulin-resistant rats treated with peroxisome proliferator activated receptor-alpha agonists. J Mol Endocrinol 30:317–329
Shao J, Gao Y, Yuan Z (1998) [Free fatty acids promoting PTP1B expression in rat skeletal muscle and hepatic cells]. Zhonghua Yi Xue Za Zhi 78:753–755
Wu Y, Ouyang JP, Wu K, Wang SS, Wen CY, Xia ZY (2005) Rosiglitazone ameliorates abnormal expression and activity of protein tyrosine phosphatase 1B in the skeletal muscle of fat-fed, streptozotocin-treated diabetic rats. Br J Pharmacol 146:234–243
Acknowledgements
S. Fernández-Veledo was a recipient of a post-doctoral contract Juan de la Cierva and I. Nieto-Vazquez was a recipient of a pre-doctoral fellowship from Ministry of Education and Science, Spain. This work was supported by grant BFU2005-03054 from Ministry of Education and Science, Spain. We thank S. A. Smith (Glaxo SmithKline, Harlow, UK) for kindly providing rosiglitazone and M. A. Moro (Universidad Complutense, Madrid, Spain) for kindly providing GW3965.
Duality of interest
C. Rondinone was formerly employed by Abbott Laboratories. There was no duality of interest for the use of any of the nuclear receptor agonists, which are published reference molecules and commercially available. The authors are not aware of any duality of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fernández-Veledo, S., Nieto-Vazquez, I., Rondinone, C.M. et al. Liver X receptor agonists ameliorate TNFα-induced insulin resistance in murine brown adipocytes by downregulating protein tyrosine phosphatase-1B gene expression. Diabetologia 49, 3038–3048 (2006). https://doi.org/10.1007/s00125-006-0472-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-006-0472-4