Abstract
Aims/hypothesis
The aim of this study was to investigate changes in insulin sensitivity and expression of the gene encoding resistin (Retn) in adipocytes from long-term nitric oxide (NO)-deficient rats.
Methods
Male Sprague–Dawley rats received \( N^{\omega } \)-nitro-l-arginine methyl ester (L-NAME 0.5 mg/ml) in their drinking water for 4 weeks, while control rats received plain drinking water. During the experimental period, changes in plasma glucose, insulin and C-peptide levels were measured. After administration of L-NAME for 4 weeks, insulin sensitivity was evaluated in vivo and in vitro. An insulin binding assay was also performed to determine the number and binding affinity of insulin receptors in adipocytes. Adipocyte Retn mRNA levels were examined using northern blotting.
Results
Successful induction of NO deficiency was demonstrated by an increase in systemic blood pressure. No difference in plasma glucose levels was found between the two groups. Compared with the control rats, plasma insulin and C-peptide levels were significantly decreased in the NO-deficient rats, and insulin sensitivity was significantly increased. Insulin-stimulated glucose uptake and insulin binding capacity, but not binding affinity, were significantly increased in adipocytes isolated from NO-deficient rats. In addition, adipocyte Retn mRNA levels, but not plasma resistin levels, were significantly decreased in NO-deficient rats, and the Retn mRNA levels were negatively correlated with insulin sensitivity.
Conclusions/interpretation
Insulin sensitivity was increased in NO-deficient rats and this was associated with insulin binding capacity and downregulated Retn expression. These findings suggest that NO plays a regulatory role in metabolism. Dysregulation of NO production may result in the development of metabolic disorders.
Similar content being viewed by others
Introduction
Nitric oxide (NO), a pivotal endothelium-derived vasodilator, plays an important role in vascular homeostasis [1]. Impaired production of endothelial NO is associated with hypertension, hypercholesterolaemia, atherosclerosis and diabetes [2–5]. The common underlying abnormality in patients with these metabolic disorders is insulin resistance [6]. It is of interest to know whether NO modulates the metabolic effects of insulin. Conflicting evidence has been presented regarding the role of NO in the regulation of glucose metabolism. An in vitro study demonstrated that the NO donor sodium nitroprusside stimulates glucose transport and metabolism but inhibits insulin-mediated glycogen synthesis in rat skeletal muscle [7]. In differentiated 3T3-L1 adipocytes, acute treatment with sodium nitroprusside increases insulin-stimulated glucose uptake [8]. Moreover, chronic administration of \( N^{\omega } \)-nitro-l-arginine methyl ester (L-NAME), an NO synthase (NOS) inhibitor, in drinking water may decrease glucose tolerance in vivo but increase local insulin-stimulated glucose uptake in skeletal muscle in vitro [9]. Endothelial NOS (eNOS) knockout mice also exhibit insulin resistance compared with their wild-type counterparts [10, 11]. In contrast, supplementation with l-arginine, a precursor of NO, does not improve insulin resistance in diabetic rats [12]. Kapur et al. [13] demonstrated that the NO donors GEA5024 and sodium nitroprusside dose-dependently inhibit insulin-stimulated glucose transport in rat extensor digitorum, longus and soleus muscles, as well as in cultured L6 myotubes. In a clinical euglycaemic hyperinsulinaemic clamp study, systemic inhibition of NO synthesis with N G-monomethyl-l-arginine increased insulin sensitivity in healthy male subjects [14]. These observations all indicate that NO can modulate the action of insulin. However, the effect of NO on the metabolic actions of insulin remains to be fully elucidated.
In addition to acting as an energy storage pool, adipocytes secrete several biological factors called adipocytokines, including TNF-α, IL-6, leptin and adiponectin. These adipocyte-derived factors may influence insulin sensitivity and glucose metabolism [15]. Resistin, a novel adipocyte-secreted hormone, is known to play a critical role linking obesity to diabetes in rodents, and neutralisation of plasma resistin with specific antibodies substantially improves glucose tolerance and insulin action in a mouse model of type 2 diabetes [16]. Acute administration of recombinant resistin impairs glucose tolerance and the action of insulin on hepatic glucose production [16, 17]. Fasting blood glucose concentrations are significantly lower in resistin-deficient mice [18]. Overexpression of the gene encoding resistin (Retn) impairs glucose metabolism and insulin sensitivity in rodents [19]. A genetic epidemiological study of Europid families indicated that single-nucleotide polymorphisms in the Retn gene promoter region may alter the relationship between BMI and the insulin sensitivity index in non-diabetic family members of patients with type 2 diabetes [20]. These results show that resistin is an important regulator of insulin-mediated glucose metabolism, but the correlation between resistin levels and insulin sensitivity is still controversial.
Materials and methods
Materials
2-Deoxy[3H]glucose (2-DG), 125I-labelled insulin, and [32P]dCTP were purchased from Amersham (Aylesbury, UK). The insulin ELISA kit was purchased from Mercodia (Uppsala, Sweden), the C-peptide RIA kit from Linco Research. (St Charles, MO, USA), the triglyceride kit from Merck (Darmstadt, Germany), the NEFA assay kit from Wako Pure Chemical Industries (Osaka, Japan), the Tri Reagent Kit from Molecular Research Center (Cincinnati, OH, USA), the Prime-A-Gene labelling kit from Promega (Madison, WI, USA), the anti-peroxisome proliferator-activated receptor γ (PPARγ), α-tubulin antibodies and horseradish peroxidase-conjugated secondary antibodies from Santa Cruz Biotechnology (Santa Cruz, CA, USA), and the rat resistin ELISA kit from B-Bridge International (Sunnyvale, CA, USA). All other chemicals were from Sigma-Aldrich (St Louis, MO, USA).
Experimental design
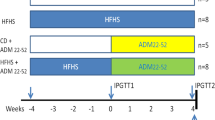
To determine whether NO plays a role in the regulation of insulin sensitivity, we examined whether changes in insulin sensitivity occur in NO-deficient rats. To further elucidate the relationship between resistin and insulin sensitivity, adipocyte Retn expression was also measured in NO-deficient rats. NO deficiency was induced with the addition of L-NAME (0.5 mg/ml) to the drinking water for 4 weeks. Various parameters, including systolic blood pressure and plasma glucose, insulin and C-peptide levels, were examined during the 4-week experimental period. During the last week, insulin sensitivity was determined by OGTT, insulin tolerance test (ITT), and steady-state plasma insulin (SSPI) and steady-state plasma glucose (SSPG) in vivo. At the end of the 4-week period, the rats were killed and glucose uptake, insulin receptor binding and Retn mRNA levels in isolated adipocytes were measured in vitro.
Animal care
Male Sprague–Dawley (200–250 g), Wistar–Kyoto (WKY; 250–300 g), and spontaneously hypertensive (SHR; 250–300 g) rats were supplied by the National Laboratory Animal Breeding and Research Center, Taipei, Taiwan. All animals were housed three to a cage in an air-conditioned room (22±2°C) on a 12-h light/dark cycle (06:00–18:00 h). Except when scheduled for OGTT, ITT, SSPI, SSPG or killing, all animals had free access to food and water. All procedures were carried out in accordance with the Taiwan Government Guide for the Care and Use of Laboratory Animals, and the research protocol was approved by the animal welfare committee of the National Yang-Ming University.
Blood pressure measurement
Narco Bio-Systems Physiograph equipment (Houston, TX, USA) was used to measure blood pressure by the tail-cuff method, as described previously [21].
Blood sample collection
Blood sampling was carried out in a quiet room starting at 10:00 h on sets of control and NO-deficient rats. Blood samples for glucose and insulin measurements (approximately 300 μl) were collected by tail bleeding into a 1.5-ml heparin-coated polyethylene microfuge tube on ice. The plasma was separated by centrifugation and stored at −20°C until assayed. Plasma glucose was measured on a glucose analyser (Model 23A; Yellow Springs Instrument Company, Yellow Springs, OH, USA). Plasma insulin, C-peptide, triglyceride, NEFA and resistin were measured with commercial kits.
OGTT
A 0-min blood sample was taken from each rat, then, without delay, the rats were given glucose solution (concentration 0.2 g/0.1 ml; 0.1 ml/100 g body weight) by gavage, and four further blood samples were collected at 30, 60, 90 and 120 min [21]. The concentrations of plasma insulin, glucose and C-peptide were determined.
Measurement of the insulin resistance indices
The fasting glucose:insulin ratio (G0/I0) was measured as described previously [22]. The homeostasis model assessment of insulin resistance (HOMA-IR) value was calculated as [fasting glucose (mmol/l)×fasting insulin (μIU/l)]/22.5 [23].
ITT
To perform ITT, rats were fasted for 6 h, and then injected i.p. with 0.75 U/kg regular human insulin (Novo Nordisk, Clayton, NC, USA) without anaesthesia, and blood samples were taken before and 15, 30, 60, 90 and 120 min after the injection [24].
SSPI and SSPG
Measurements of SSPG and SSPI were performed as described previously [25].
Preparation of adipocytes
At the end of the experiment, the rats were killed by decapitation after overnight fasting and the epididymal fat pads from each group of rats pooled to isolate adipocytes using the Rodbell method [26] with minor modifications [25].
2-deoxy[3H]glucose uptake
Glucose uptake by adipocytes was determined by measuring 2-DG transport into the cells, as described previously [25].
125I-Labelled insulin binding assay
Binding of insulin to adipocytes was measured as described previously [25]. A Scatchard plot was used to determine the number of insulin binding sites and the dissociation constant.
RNA extraction
Total RNA was extracted from adipocytes isolated from each individual rat using a Tri Reagent kit. The integrity of the RNA was examined by 1% agarose gel electrophoresis, and its concentration determined by the absorbance at 260 nm (Genequant RNA/DNA calculator; Biochrom, Cambridge, UK).
Northern blotting
Northern blotting was carried out according to a standard procedure, as described previously [27]. 32P-labelled full-length rat Retn cDNA and control glyceraldehyde-3-phosphate dehydrogenase (Gapdh) cDNA (1.1 kb; Clontech, Palo Alto, CA, USA) hybridisation probes were prepared using the random priming DNA labelling system (Promega). After hybridisation, the signals were quantified by densitometry and the signals for the two Retn mRNAs (0.8 and 1.4 kb, owing to different sizes of the 3′-untranslated region), summed and normalised to that of the corresponding Gapdh mRNA band.
Western blotting
Adipocytes were lysed with lysis buffer (1% Triton X-100, 150 mmol/l NaCl, 10 mmol/l Tris pH 7.4, 1 mmol/l EDTA, 1 mmol/l EGTA, 0.2 mmol/l PMSF, 0.5% Nonidet P-40), then 100 μg of lysate proteins were separated by SDS-PAGE using a 7.5% polyacrylamide gel and electroblotted onto a poly(vinylidene fluoride) membrane. All western blotting procedures were carried out as previously described [25].
Statistical analysis
All results are expressed as the means±SD. Differences between the two groups were analysed either by the Student’s t-test or by two-way ANOVA with a post hoc t test when multiple measurements were made. Pearson correlation coefficients (r) were calculated to quantify relationships between Retn mRNA levels, fat pad weight and insulin resistance indices, such as the I0, G0/I0 and HOMA-IR. Differences between the two groups were considered statistically significant when the p value was <0.05.
Results
Characteristics of the two groups
As expected (Fig. 1), chronic administration of L-NAME resulted in a significant increase in the systolic blood pressure from 1 week of administration (145±5.0 vs 115±4.2 mmHg for the control rats, p<0.05), and this hypertensive status was maintained to the end of the experiment (166±9.1 vs 123±3.6 mmHg, p<0.05). This hypertensive response shows that an NO-deficient status was successfully induced in the rats by L-NAME administration. Table 1 shows the body weight, epididymal fat pad weight, relative epididymal fat pad weight, fasting glucose and insulin concentrations, the insulin resistance indices, and fasting triglyceride, NEFA and resistin concentrations after the 4-week experimental period. Fasting plasma glucose, triglyceride, NEFA and resistin concentrations were similar in the two groups, but the fasting plasma insulin concentration was significantly lower in the NO-deficient rats than in the control rats. The changes in the G0/I0 and HOMA-IR also indicated that NO-deficient rats were more insulin-sensitive than the control rats. No significant difference was seen in body weight between the two groups.
The epididymal fat pad weight was significantly decreased in the NO-deficient rats compared with the control rats (Table 1). Analysis of adipocyte size revealed that adipocyte diameter was significantly decreased in the NO-deficient rats compared with the control rats (34.9±0.1 vs 42.8±0.1 μm, p<0.05). This result suggested that chronic NO deficiency in the rat caused a clear alteration in adipocyte size. Adipocyte differentiation may contribute to the change in adipocyte size in NO-deficient rats. To address this issue, we measured levels of PPARγ, the essential transcription factor for adipocyte differentiation [28], by western blotting. Results showed that PPARγ levels were significantly increased by 1.5-fold in adipocytes isolated from NO-deficient rats compared with those isolated from the control rats.
Plasma glucose, insulin and C-peptide levels
Figure 2 shows the changes in plasma glucose, insulin and C-peptide levels in the two groups during the 4-week experimental period. There was no difference in plasma glucose between the two groups, but plasma insulin and C-peptide were significantly lower in NO-deficient rats compared with control rats within 1 week of the start of L-NAME administration (79.9±8.3 vs 121.5±9.7 pmol/l, p<0.05 for insulin; 164.0±17.4 vs 268.4±23.7 pmol/l, p<0.05 for C-peptide), and remained significantly lower throughout the experiment.
Insulin sensitivity
The OGTT results obtained for the two groups on day 3 of the last experimental week are shown in Fig. 3a–c and Table 2. Baseline plasma glucose levels were not different in the two groups, and levels in both groups increased similarly after oral glucose loading. The NO-deficient rats had significantly lower baseline plasma insulin and C-peptide levels than the control rats. In response to oral glucose challenge, both the NO-deficient and control rats responded with an increase in plasma insulin and C-peptide levels, but the levels in the NO-deficient rats were significantly lower than those in the control rats. As shown in Table 2, there was no significant difference in the ΔAUCglucose (change in the area under the glucose profile curve during the OGTT) between the NO-deficient and control groups. However, the values for the ΔAUCinsulin (change in the area under the insulin profile curve during the OGTT) and 2-h insulin were significantly decreased in the NO-deficient group, suggesting that the NO-deficient rats were more insulin-sensitive than the control rats. The value for the ΔAUCC-peptide (change in the area under the C-peptide profile curve during the OGTT) in the NO-deficient rats was also significantly decreased, indicating that insulin secretion in the NO-deficient group was suppressed. These results suggest that insulin-stimulated glucose utilisation in insulin target tissues was more sensitive to insulin in the NO-deficient rats than the control rats. Furthermore, the C-peptide response also suggested that insulin secretion was decreased or suppressed after 4 weeks of L-NAME administration.
OGTT and ITT responses in NO-deficient and control rats. Plasma glucose (a), insulin (b) and C-peptide (c) responses to oral glucose challenge, and glucose curves (d) from the ITT in NO-deficient (filled circles) and control rats (empty circles). In the ITT assay, plasma glucose levels were normalised to those at t=0 min in each group (100%). The values are the means±SD for eight rats. *p<0.05 vs the untreated control group at the corresponding time point
Further data on the effect of chronic NO deficiency on insulin sensitivity in vivo are provided in Figs 3d and 4. The results of the ITT indicated that the overall insulin sensitivity was significantly increased in the NO-deficient rats. Thus, the glucose-lowering effect of insulin was significantly increased in the NO-deficient rats compared with the control rats at 30, 60, 90 and 120 min (p<0.05) (Fig. 3d). Furthermore, no significant difference in SSPI was found between control and NO-deficient rats (Fig. 4a). However, SSPG was significantly lower in NO-deficient rats than in control rats (3.53±0.09 vs 5.52±0.05 mmol/l, p<0.05) (Fig. 4b). Consistent with our OGTT data, the ITT, SSPG and SSPI results indicated that the NO-deficient rats were more insulin-sensitive than the control rats.
Effect of chronic NO deficiency on SSPI (a) and SSPG (b). Rats were pre-infused with somatostatin for 30 min, after which time they were co-infused with the mixed solution of somatostatin, insulin and glucose for 180 min. The mean plasma insulin and glucose levels during the 135–180-min period were designated as SSPI and SSPG. The values are the means±SD for eight rats. *p<0.05 vs control rats
Glucose uptake and insulin receptor characteristics of isolated adipocytes
To further clarify the changes in cellular insulin sensitivity in NO-deficient rats, we measured basal and insulin-stimulated glucose uptake by adipocytes isolated from NO-deficient rats and control rats. As shown in Fig. 5, basal 2-DG uptake by adipocytes was similar in the two groups (66.4±3.5 vs 63.6±7.4 fmol/105 cells/3 min). However, physiological (10−10 mol/l) and pharmacological (10−7 mol/l) doses of insulin stimulated more glucose uptake by adipocytes isolated from NO-deficient rats than by control adipocytes (10−10 mol/l insulin: 139.7±10.5 vs 100.4±10.5 fmol/105 cells/3 min, p<0.05; 10−7 mol/l insulin: 204.3±12.3 vs 136.6±16.1 fmol/105 cells/3 min, p<0.05). These data show that cellular insulin sensitivity was significantly increased in the NO-deficient rats.
2-DG uptake by adipocytes isolated from NO-deficient (filled bars) and control (empty bars) rats. The adipocytes were pre-incubated for 30 min at 37°C with vehicle or a physiological (10−10 mol/l) or pharmacological (10−7 mol/l) dose of insulin, then glucose uptake was determined as described in the Materials and methods section. The values are the means±SD of four separate experiments. *p<0.05 vs the corresponding untreated controls
To determine the mechanism responsible for the increased insulin-stimulated glucose uptake in isolated adipocytes from NO-deficient rats, we examined whether insulin binding to adipocytes was altered. As shown in Fig. 6, insulin binding was significantly increased in adipocytes isolated from NO-deficient rats compared with those isolated from control rats. Scatchard analysis (Table 3) showed that there was no difference in the dissociation constant for insulin between the two groups, but that the insulin binding capacity was significantly increased in the adipocytes isolated from NO-deficient rats. This suggests that the enhanced insulin-sensitised response in adipocytes isolated from NO-deficient rats results from the increase in the number of insulin receptors.
Analysis of binding of insulin to adipocytes. Competitive binding curve (a) and Scatchard plot (b) of insulin binding to adipocytes isolated from NO-deficient (filled circles) or control (empty circles) rats. The adipocytes were incubated with 125I-labelled insulin plus various concentrations of unlabelled insulin. Binding assays were performed as described in the Materials and methods section. The values are the means±SD of four separate experiments. *p<0.05 vs the corresponding untreated controls
Retn gene expression in isolated adipocytes
Adipocyte Retn mRNA levels in the L-NAME-treated and control groups were evaluated by northern blotting. Figure 7a shows the results of a representative northern blot using a Retn-specific probe. Two transcripts 0.8 and 1.4 kb in length were seen, the same sizes as reported previously for rat Retn [29]. Retn mRNA levels were significantly lower in the adipocytes isolated from NO-deficient rats than in those from control rats (Fig. 7c, p<0.05). Furthermore, the adipocyte Retn mRNA levels showed positive correlations with fat pad weight and the insulin resistance indices (Table 4).
Retn mRNA levels in adipocytes from NO-deficient and control rats, and from Wistar–Kyoto (WKY) and SHR rats. Total RNA isolated from adipocytes from control or NO-deficient rats was subjected to northern blotting (15 μg RNA per lane) using rat Retn and Gapdh probes. a, b Representative northern blot showing the two rat Retn mRNAs with sizes of 1.4 and 0.8 kb owing to differences in the 3′ untranslated region. c, d Results of the densitometric analysis normalised to the Gapdh mRNA levels. The values are the means±SD for eight rats. *p<0.05 vs the control group
Furthermore, to clarify the hypertensive effect on adipose Retn expression, we studied adipose Retn expression in SHR (body weight: 317.2±10.9 g; systolic blood pressure: 185.9±5.6 mmHg) and normotensive WKY (body weight: 310.9±7.1 g; systolic blood pressure: 133.4±3.8 mmHg) rats. Our data showed that adipose Retn mRNA expression was very similar in these two groups (Fig. 7b,d). The results also suggested that high blood pressure cannot regulate adipose Retn gene expression.
Discussion
In the present study we found that insulin sensitivity was increased in rats rendered NO-deficient by the chronic administration of L-NAME in drinking water. Further exploration of the effects of insulin on adipocytes revealed that insulin-stimulated glucose uptake was significantly increased in adipocytes isolated from NO-deficient rats, and that this was associated with an increase in the number of insulin receptors. These findings are consistent with the clinical observation that systemic inhibition of NOS increases insulin sensitivity in man [14] and the finding that intravenous administration of an NO donor causes decreased glucose tolerance in dogs [30]. However, some conflicting results have been reported. For example, acute administration of L-NAME does not result in glucose tolerance in vivo or in decreased muscle glucose uptake in vitro [31]; the discrepancy between the lack of effect on insulin sensitivity in this study and the effect seen in the present study may be due to differences in the experimental conditions, such as differences in the dose, delivery route and duration of L-NAME administration. Balon et al. [9] found that chronic NOS inhibition decreases glucose tolerance in rats as a result of insufficient insulin secretion, and, on further evaluating the change in cellular insulin sensitivity, found that insulin-stimulated glucose transport in skeletal muscle was increased by chronic NOS inhibition. This finding is consistent with our data for adipocytes isolated from NO-deficient rats.
Balon’s study [9] showed that the insulin secretion response to glucose challenge is decreased in NO-deficient rats. In the present study, we found that basal plasma insulin and C-peptide levels were significantly lower in NO-deficient rats than in control rats (Fig. 2). The results of the OGTT showed that the ΔAUCinsulin and ΔAUCC-peptide were also decreased in NO-deficient rats (Fig. 3b,c and Table 2). These observations show that insulin secretion is decreased in the NO-deficient state. The study by Pueyo et al. [32] showed that chronic NOS blockade does not alter insulin secretion in response to several secretagogues, including d-glucose, l-arginine and d-arginine. According to their findings, insulin hyposecretion in NO-deficient rats may be a compensatory response to the increased insulin sensitivity. However, we cannot fully exclude an influence of NO on regulation of insulin secretion. A different study has shown that NO has a dual effect on regulation of insulin secretion in rat pancreatic beta cells, facilitating insulin secretion in a cGMP-dependent manner at low concentrations and inhibiting it in a cGMP-independent manner at high concentrations [33]. Thus, the regulatory role of NO in pancreatic insulin secretion in NO-deficient rats needed to be further explored.
Our in vitro study showed that insulin-stimulated glucose uptake by adipocytes isolated from NO-deficient rats was significantly increased (Fig. 5). A similar result was obtained in Balon’s study [9]. In addition, Kapur et al. [13] reported that NO donors induce dose-dependent inhibition of maximal insulin-stimulated glucose transport in L6 muscle cells. These findings strongly suggest that NO may decrease the metabolic action of insulin. Furthermore, the number of insulin binding sites was significantly increased in adipocytes isolated from NO-deficient rats (Fig. 6 and Table 3). The influence of NO on insulin receptor number has also been explored by Ragoobirsingh and colleagues, who found that NO donor administration results in the decreased binding of insulin to its receptor on the cell membrane of mononuclear leucocytes in dogs [34]. These data support the hypothesis that NO inhibits insulin action by modulating insulin binding to its receptor.
In biological systems, NO is synthesised from l-arginine by NOSs. Three NOS isozymes are responsible for NO formation: the constitutively expressed neuronal NOS (nNOS) [35], eNOS [36], and cytokine-inducible NOS (iNOS) [37]. The contribution of these three NOSs to the regulation of the metabolic actions of insulin has been extensively explored. Human genetic epidemiological studies have shown that eNOS polymorphisms are associated with insulin resistance [38–40]. Mice with complete disruption of the gene encoding eNOS (Nos3) exhibit insulin resistance [10, 11]. Furthermore, although partial deletion of the Nos3 gene does not alter insulin sensitivity in mice, the animals develop insulin resistance when fed a high-fat diet, providing further evidence of the importance of this gene in metabolic disorders [41]. The role of nNOS in the regulation of glucose homeostasis is not clear, and there is little evidence that it modulates insulin sensitivity. On the other hand, stimulation of iNOS and subsequent NO overproduction can cause insulin resistance. For example, injection of rats with lipopolysaccharide (LPS) leads to hyperglycaemia, insulin resistance and increased iNOS protein expression and activity [42], and aminoguanidine (a specific iNOS inhibitor) ameliorates LPS-induced hyperglycaemia and insulin resistance [42]. These data indicate that iNOS plays a regulatory role in the metabolic actions of insulin. Moreover, mice with complete disruption of the iNOS gene are protected from high-fat-induced insulin resistance [43]. These findings provide evidence that iNOS is involved in the development of insulin resistance in diet-induced obesity. In the present study, L-NAME was used to inhibit all NOS isoforms and was found to enhance insulin sensitivity in rats. It was very difficult to clarify which NOS isoform was the major contributor in the NO-deficient rats. To address this question, further investigations using specific eNOS or iNOS inhibitors in rats are needed to elucidate the precise roles of eNOS and iNOS in insulin sensitivity.
The physiological role of NO in adipocytes remains unclear. Clinical observation showed that increases in circulating NO levels correlated strongly with body fat in obesity, an insulin resistant status [44]. In the present study, chronic NO deficiency caused a significant decrease in fat pad weight (Table 1) and a significant increase in insulin sensitivity in rats (Figs 3, 4 and Table 2). These findings strongly support the hypothesis that increased NO production may impair insulin sensitivity and increase lipid storage in adipose tissues.
In addition, eNOS and iNOS can be detected in rat white adipose tissue [45] and human adipocytes [46], suggesting that NO may be involved in the regulation of energy metabolism. Furthermore, expression of the eNOS and iNOS genes in adipocytes is significantly increased in obesity [46], a chronic inflammatory state. Expression of iNOS, but not that of eNOS, is significantly increased during adipocyte differentiation [46, 47], and NO has been shown to be involved in the positive modulation of pre-adipocyte differentiation [47]. Collectively, these data show that the homeostasis of eNOS and iNOS expression is important in metabolism, i.e. constitutive expression of eNOS seems to be necessary to maintain normal insulin sensitivity, while activation of iNOS might contribute to impairment of insulin sensitivity.
In the present study we also found that Retn gene expression in adipocytes was significantly decreased in NO-deficient rats. Furthermore, adipocyte Retn mRNA levels correlated with fat pad weight and the insulin resistance indices. These results are in agreement with previous reports [16–20]. Our findings also evoke the possibility that NO may regulate Retn expression in adipocytes. Some indirect evidence also supports the role of NO in Retn expression. For example, LPS, which is thought to increase iNOS activity and subsequent NO production [42], increases Retn mRNA levels in 3T3-L1 adipocytes [48]. In addition, TNF-α increases iNOS activity in adipocytes [49] and also increases adipocyte Retn mRNA levels [50]. However, the precise mechanism by which NO regulates resistin expression in adipocytes needs further investigation.
In conclusion, our in vitro and in vivo findings show that insulin sensitivity is enhanced in both isolated adipocytes and conscious rats in the chronic NO-deficient state. Since we observed similar effects in vivo and in vitro, we believe that our findings provide an accurate picture of the chronic effect of NO deficiency on insulin sensitivity. These results also support the concept that NO plays a pivotal role in modulating energy metabolism in both physiological and pathological conditions. Overproduction of NO, through eNOS or iNOS activation, may impair insulin-stimulated glucose uptake in insulin target cells, including adipocytes. However, this hypothesis requires further testing.
Abbreviations
- 2-DG:
-
2-deoxy[3H]glucose
- eNOS:
-
endothelial nitric oxide synthase
- HOMA-IR:
-
homeostasis model assessment of insulin resistance
- iNOS:
-
inducible nitric oxide synthase
- ITT:
-
insulin tolerance test
- L-NAME:
-
\( N^{\omega } \)-nitro-l-arginine methyl ester
- LPS:
-
lipopolysaccharide
- nNOS:
-
neuronal nitric oxide synthase
- NO:
-
nitric oxide
- PPARγ:
-
peroxisome proliferator-activated receptor γ
- SHR:
-
spontaneously hypertensive rat
- SSPG:
-
steady-state plasma glucose
- SSPI:
-
steady-state plasma insulin
References
Dominiczak AF, Bohr DF (1995) Nitric oxide and its putative role in hypertension. Hypertension 25:1202–1211
Ceravolo R, Maio R, Pujia A et al (2003) Pulse pressure and endothelial dysfunction in never-treated hypertensive patients. J Am Coll Cardiol 41:1753–1758
John S, Schmieder RE (2003) Potential mechanisms of impaired endothelial function in arterial hypertension and hypercholesterolemia. Curr Hypertens Rep 5:199–207
Kawashima S (2004) Malfunction of vascular control in lifestyle-related diseases: endothelial nitric oxide (NO) synthase/NO system in atherosclerosis. J Pharmacol Sci 96:411–419
Caballero AE (2004) Endothelial dysfunction, inflammation, and insulin resistance: a focus on subjects at risk for type 2 diabetes. Curr Diab Rep 4:237–246
Reaven GM (1988) Role of insulin resistance in human disease. Diabetes 37:1595–1607
Young ME, Radda GK, Leighton B (1997) Nitric oxide stimulates glucose transport and metabolism in rat skeletal muscle in vitro. Biochem J 322:223–228
Tanaka T, Nakatani K, Morioka K et al (2003) Nitric oxide stimulates glucose transport through insulin-independent GLUT4 translocation in 3T3-L1 adipocytes. Eur J Endocrinol 149:61–67
Balon TW, Jasman AP, Young JC (1999) Effects of chronic \( N^{\omega } \)-nitro-l-arginine methyl ester administration on glucose tolerance and skeletal muscle glucose transport in the rat. Nitric Oxide 3:312–320
Duplain H, Burcelin R, Sartori C et al (2001) Insulin resistance, hyperlipidemia, and hypertension in mice lacking endothelial nitric oxide synthase. Circulation 104:342–345
Shankar RR, Wu Y, Shen HQ, Zhu JS, Baron AD (2000) Mice with gene disruption of both endothelial and neuronal nitric oxide synthase exhibit insulin resistance. Diabetes 49:684–687
Kawano T, Nomura M, Nisikado A, Nakaya Y, Ito S (2003) Supplementation of l-arginine improves hypertension and lipid metabolism but not insulin resistance in diabetic rats. Life Sci 73:3017–3026
Kapur S, Bedard S, Marcotte B, Cote CH, Marette A (1997) Expression of nitric oxide synthase in skeletal muscle: a novel role for nitric oxide as a modulator of insulin action. Diabetes 46:1691–1700
Butler R, Morris AD, Struthers AD (1998) Systemic nitric oxide synthase inhibition increases insulin sensitivity in man. Clin Sci (Lond) 94:175–180
Spiegelman BM, Flier JS (1996) Adipogenesis and obesity: rounding out the big picture. Cell 87:377–389
Steppan CM, Bailey ST, Bhat S et al (2001) The hormone resistin links obesity to diabetes. Nature 409:307–312
Muse ED, Obici S, Bhanot S et al (2004) Role of resistin in diet-induced hepatic insulin resistance. J Clin Invest 114:232–239
Banerjee RR, Rangwala SM, Shapiro JS et al (2004) Regulation of fasted blood glucose by resistin. Science 303:1195–1198
Satoh H, Nguyen MT, Miles PD, Imamura T, Usui I, Olefsky JM (2004) Adenovirus-mediated chronic “hyper-resistinemia” leads to in vivo insulin resistance in normal rats. J Clin Invest 114:224–231
Wang H, Chu WS, Hemphill C, Elbein SC (2002) Human resistin gene: molecular scanning and evaluation of association with insulin sensitivity and type 2 diabetes in Caucasians. J Clin Endocrinol Metab 87:2520–2524
Juan CC, Shen YW, Chien Y, Lin YJ, Chang SF, Ho LT (2004) Insulin infusion induces endothelin-1-dependent hypertension in rats. Am J Physiol Endocrinol Metab 287:E948–E954
Legro RS, Driscoll D, Strauss JF III, Fox J, Dunaif A (1998) Evidence for a genetic basis for hyperandrogenemia in polycystic ovary syndrome. Proc Natl Acad Sci U S A 95:14956–14960
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Satoh H, Nguyen MT, Trujillo M et al (2005) Adenovirus-mediated adiponectin expression augments skeletal muscle insulin sensitivity in male Wistar rats. Diabetes 54:1304-1313
Juan CC, Chien Y, Wu LY et al (2005) Angiotensin II enhances insulin sensitivity in vitro and in vivo. Endocrinology 146:2246–2254
Rodbell M (1964) Metabolism of isolated fat cells. I. Effects of hormones on glucose metabolism and lipolysis. J Biol Chem 239:375–380
Huang SW, Seow KM, Ho LT et al (2005) Resistin mRNA levels are downregulated by estrogen in vivo and in vitro. FEBS Lett 579:449–454
Rosen ED, Sarraf P, Troy AE et al (1999) PPAR gamma is required for the differentiation of adipose tissue in vivo and in vitro. Mol Cell 4:611–617
Kim KH, Lee K, Moon YS, Sul HS (2001) A cysteine-rich adipose tissue-specific secretory factor inhibits adipocyte differentiation. J Biol Chem 276:11252–11256
McGrowder D, Ragoobirsingh D, Dasgupta T (2001) Effects of S-nitroso-N-acetyl-penicillamine administration on glucose tolerance and plasma levels of insulin and glucagon in the dog. Nitric Oxide 5:402–412
Bursztyn M, Raz I, Mekler J, Ben-Ishay D (1997) Effect of acute N-nitro-l-arginine methyl ester (L-NAME) hypertension on glucose tolerance, insulin levels, and [3H]-deoxyglucose muscle uptake. Am J Hypertens 10:683–686
Pueyo ME, Gonzalez W, Pussard E, Arnal JF (1994) Insulin secretion in rats with chronic nitric oxide synthase blockade. Diabetologia 37:879–884
Kaneko Y, Ishikawa T, Amano S, Nakayama K (2003) Dual effect of nitric oxide on cytosolic Ca2+ concentration and insulin secretion in rat pancreatic beta-cells. Am J Physiol Cell Physiol 284:C1215–C1222
Ragoobirsingh D, McGrowder D, Dasgupta T, Brown P (2004) The effect of nitric oxide on glucose metabolism. Mol Cell Biochem 263:29–34
Bredt DS, Hwang PM, Snyder SH (1990) Localization of nitric oxide synthase indicating a neural role for nitric oxide. Nature 347:768–770
Moncada S, Radomski MW, Palmer RM (1988) Endothelium-derived relaxing factor. Identification as nitric oxide and role in the control of vascular tone and platelet function. Biochem Pharmacol 37:2495–2501
Nathan CF, Hibbs JB Jr (1991) Role of nitric oxide synthesis in macrophage antimicrobial activity. Curr Opin Immunol 3:65–70
Ohtoshi K, Yamasaki Y, Gorogawa S et al (2002) Association of (−)786T-C mutation of endothelial nitric oxide synthase gene with insulin resistance. Diabetologia 45:1594–1601
Monti LD, Barlassina C, Citterio L et al (2003) Endothelial nitric oxide synthase polymorphisms are associated with type 2 diabetes and the insulin resistance syndrome. Diabetes 52:1270–1275
Yoshimura T, Hisatomi A, Kajihara S et al (2003) The relationship between insulin resistance and polymorphisms of the endothelial nitric oxide synthase gene in patients with coronary artery disease. J Atheroscler Thromb 10:43–47
Cook S, Hugli O, Egli M et al (2004) Partial gene deletion of endothelial nitric oxide synthase predisposes to exaggerated high-fat diet-induced insulin resistance and arterial hypertension. Diabetes 53:2067–2072
Sugita H, Kaneki M, Tokunaga E et al (2002) Inducible nitric oxide synthase plays a role in LPS-induced hyperglycaemia and insulin resistance. Am J Physiol Endocrinol Metab 282:E386–E394
Perreault M, Marette A (2001) Targeted disruption of inducible nitric oxide synthase protects against obesity-linked insulin resistance in muscle. Nat Med 7:1138–1143
Choi JW, Pai SH, Kim SK, Ito M, Park CS, Cha YN (2001) Increases in nitric oxide concentrations correlate strongly with body fat in obese humans. Clin Chem 47:1106–1109
Ribiere C, Jaubert AM, Gaudiot N et al (1996) White adipose tissue nitric oxide synthase: a potential source for NO production. Biochem Biophys Res Commun 222:706–712
Engeli S, Janke J, Gorzelniak K et al (2004) Regulation of the nitric oxide system in human adipose tissue. J Lipid Res 45:1640–1648
Yan H, Aziz E, Shillabeer G et al (2002) Nitric oxide promotes differentiation of rat white preadipocytes in culture. J Lipid Res 43:2123–2129
Lu SC, Shieh WY, Chen CY, Hsu SC, Chen HL (2002) Lipopolysaccharide increases resistin gene expression in vivo and in vitro. FEBS Lett 530:158–162
Merial C, Bouloumie A, Trocheris V, Lafontan M, Galitzky J (2000) Nitric oxide-dependent downregulation of adipocyte UCP-2 expression by tumor necrosis factor-alpha. Am J Physiol Cell Physiol 279:C1100–C1106
Lin SY, Sheu WH, Chen WY, Lee FY, Huang CJ (2005) Stimulated resistin expression in white adipose of rats with bile duct ligation-induced liver cirrhosis: relationship to cirrhotic hyperinsulinemia and increased tumor necrosis factor-alpha. Mol Cell Endocrinol 232:1–8
Acknowledgements
This work was supported by research grants from the Yen Tjing Ling Medical Foundation (CI-95-2), the National Science Council of Taiwan (NSC93-2314-B-010-031), the Veterans General Hospitals University System of Taiwan (VGHUST94-P7-49), and a grant from the Ministry of Education, Aim for the Top University Plan.
Duality of interest The authors declare that they have no duality of interest relating to this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Juan, C.C., Chang, C.L., Chuang, T.Y. et al. Insulin sensitivity and resistin expression in nitric oxide-deficient rats. Diabetologia 49, 3017–3026 (2006). https://doi.org/10.1007/s00125-006-0403-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-006-0403-4