Abstract
Aims/hypothesis
Pharmacokinetics of s.c. administered insulin preparations have been widely studied, mostly using descriptive measures such as AUC, time to peak, or the peak plasma concentration. Several compartmental modelling studies of single-bolus s.c. insulin pharmacokinetics have also appeared, with contrasting results regarding the feasibility of insulin pharmacokinetics modelling and the appropriate level of detail for such models. In this paper, we used compartmental models to study the pharmacokinetics of biphasic insulin aspart administered by multiple s.c. injections. The main objective was to assess the magnitude of the inter-and intra-subject variation in the kinetics.
Materials and methods
Analyses were performed on 24-h serum insulin concentrations measured in 20 type 1 diabetes subjects given three daily s.c. injections of biphasic insulin aspart.
Results
Preliminary analysis of the AUC:dose ratio showed that the apparent kinetics are not constant throughout the three daily injections of the compound. A simple and robust compartmental model was shown to be appropriate for interpreting the observations, provided that one of its parameters (the first-order rate constant for transfer from the s.c. depot to plasma) is allowed to vary between injections.
Conclusions/interpretation
Population estimates of the chosen model show that intra-subject variations between injections is of the same order of magnitude as inter-subject variation, partially explaining the difficulties encountered when individually tailoring intensified insulin therapy. We conclude that the explicit consideration of a rather simple kinetic model will allow better experimental designs in the future study of s.c. insulin preparations.
Similar content being viewed by others
Introduction
In subjects with type 1 diabetes, exogenous insulin is necessary for regulation of glycaemia. Patients achieve better blood glucose control through intensified insulin therapy designed to mimic the endogenous insulin secretion of healthy subjects. Optimal control would reduce hyperglycaemia, which may cause long-term microvascular damage, blindness, renal impairment and peripheral neuropathy; it would also reduce the risk of life-threatening hypoglycaemia. Large randomised long-term clinical trials such as the Diabetes Control and Complications Trial (DCCT) [1] have shown that the incidence of severe late complications can be reduced significantly by intensifying treatment, an approach, however, which also carries an increased risk of hypoglycaemic episodes. A better understanding of the pharmacokinetics of s.c. injected insulin is instrumental for improving the design of intensified insulin treatment. However, insulin pharmacokinetics shows considerable variation not only between patients, but also within the same patient over multiple injections. In order to individualise and optimise insulin treatment, it is therefore essential to assess the source of such variation.
In this paper, we studied the pharmacokinetics of a biphasic pre-mixed insulin analogue after multiple meal-time s.c. bolus injections in type 1 diabetes subjects. The rationale behind the development of this insulin preparation was that the soluble fraction of the biphasic mixture should provide rapid increases in circulating insulin after meals, while the protamine fraction should provide a basal level, mimicking the insulin concentration time-course seen in normal subjects [2].
Standard intensified insulin therapy for type 1 diabetes patients requires daily multiple meal-time and daily basal bolus s.c. insulin injections. The pre-mixed insulin preparation aims to obviate the need for basal insulin injections. Indeed, it is thought that administration of the slow component in multiple doses along with the rapid component might produce a more stable basal insulin concentration.
Most published studies on insulin pharmacokinetics are either based on descriptive characteristic measures such as AUC, the maximum concentration (Cmax), and the time to Cmax (Tmax), or on compartmental modelling of the mean time-course of insulin concentration after a single s.c. bolus injection of the hormone [3, 4].
In this paper, we investigate the pharmacokinetics of biphasic insulin mixture through compartmental modelling, considering specifically the variation of the kinetics after multiple s.c. injections, since this variation is an important limiting factor in tailoring intensified insulin therapy. We analyse observed insulin concentrations using a nonlinear mixed effects compartment model with nested random effects, including between- and within-subject variations that affect the absorption rate of the insulin. A simplified model, including between-subject variation only, was also studied. Besides identifying an appropriate mathematical representation for describing time–concentration insulin data, the aim of the present work was to quantify intra-subject variability in kinetics, and compare its magnitude with that of inter-subject variability.
Materials and methods
Experimental procedure
The data came from a previously published study of a biphasic insulin aspart (IAsp) preparation [5]. The complete 24-h serum insulin concentrations measured in the 20 type 1 diabetes subjects, who were given three daily s.c. injections at different sites within the abdominal region, are presented in Fig. 1. The biphasic IAsp is composed of 30% fast-acting (soluble) IAsp and 70% prolonged-acting (protamine) IAsp crystals. The amino acid proline at position 28 in the B-chain of human insulin is replaced by aspartic acid in IAsp. This reduces its tendency to self-association [6, 7] and increases the rate of absorption after s.c. injection leading to shorter Tmax and higher Cmax than achieved with human insulin [2]. Similar results are observed when the pharmacokinetics of biphasic IAsp is compared with biphasic human insulin [8].
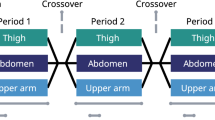
The study was designed as a randomised, double-blinded, two-period crossover protocol with a washout period of 2 to 8 weeks. Insulin was administered s.c. in the abdominal region three times daily at 08.00, 13.00 and 18.00 h just before standardised meals, in ratios of 30:30:40% with respect to the total previous daily dose. A conversion factor of 6 nmol to 1 U was applied throughout [9]. The protocol’s endpoints did not include modelling of the pharmacokinetics.
For each subject, 44 venous blood samples were collected at 15-min intervals during the first 90 min after the injection, followed by 30-min intervals for the next hour, and by hourly intervals thereafter. Serum IAsp was assayed at Nova Medical Medi-Lab (Copenhagen, Denmark), using a validated immunoassay specific for IAsp (Novo Nordisk, Bagsvaerd, Denmark). The lower limit of quantification (LLoQ) for the assay was 13 pmol/l. Of the 873 insulin concentrations measured, 70 were reported to be below the LLoQ and 16 came from haemolysed blood samples.
Modelling
The pharmacokinetics models considered are based on descriptions of the absorption, distribution and elimination of injected insulin. It is assumed that the soluble IAsp in the preparation is immediately available for absorption, while the protamine IAsp crystals must first dissolve before sharing the same pharmacokinetics as the soluble IAsp component. Thus, it is the net dissolution process that is modelled, since the backward process is considered negligible. IAsp, absorbed into the blood circulation from the injection site, is then eliminated from plasma with a first-order kinetics. The models are illustrated in Fig. 2 and are specified by the following equations:
where I cj is the amount of protamine IAsp crystals in the s.c. depot injected at meal j=1, 2, 3, and I sj is the corresponding amount of soluble IAsp, I p is the plasma insulin concentration, K c is the net rate constant for the dissolution of the IAsp crystals, K a is the absorption rate from the soluble IAsp to plasma, K x is the elimination rate from plasma, V is the volume of distribution, D j is the dose injected at meal j, t j is the time when injection at meal j is administered, α is the fraction of fast-acting insulin (0.3 in this case), and δ is the Dirac delta, making it possible to represent a succession of insulin injections within the framework of the differential equation associated with the receiving compartment. The general equations actually specify two different kinetic models depending on whether we consider K a1=K a2=K a3=K a (‘fixed kinetics model’, Model 1, Fig. 2a) or whether we allow the three rate constants, associated with the absorption of the soluble IAsp after the three injections, to differ from one another (‘varying kinetics model’, Model 2, Fig. 2b).
Illustration of the two compartmental models, Model 1 (a) and Model 2 (b), with protamine IAsp crystals (Ic) and soluble IAsp (Is) in the s.c. depot, and plasma IAsp (Ip). α is the fraction of Is (0.3 in this case), D is the dose injected, K c is the net dissolution rate, K a is the absorption rate of IAsp from the injection site to plasma insulin, K x is the elimination rate from plasma insulin and V is the apparent volume of distribution of the plasma insulin. Model 1 is a simplified version of Model 2, which allows different rates of absorption between the three daily injections within patients
Model 1 was extended to Model 2 as proposed, because it is reasonable to suppose, and has been reported [10], that the lack of homogeneity in injection site characteristics (e.g. blood supply to site, thickness of local adipose tissue layer, depth of injection, volume injected, etc.) is responsible for variable absorption rates. Since the net dissolution from protamine IAsp crystals to soluble IAsp is a chemical process believed to be relatively independent of injection site characteristics, it is assumed that the coefficient K c does not vary within the same subject. It is also assumed that the kinetics is not influenced by subsequent insulin injections into neighbouring sites and that the insulin elimination rate does not vary throughout the day within subjects. The model is expressed in such a way that the transfer of the IAsp crystals to plasma is restricted to be slower than the transfer of soluble IAsp to plasma without any artificial imposition of limits on K c or K a.
Statistical analysis
Data from haemolysed samples were excluded from the analysis since the destruction of erythrocytes in the blood sample may cause bias in the insulin assay [11]. All parameters were log-transformed to ensure positive parameter values; the results were expressed in both the log-scale and in the original scale.
Non-compartmental AUC analysis
The data were first analysed non-compartmentally to assess the between-meal variation by ANOVA of the log (AUC:dose). The AUC of serum IAsp concentration over the 5 h after injection was calculated for each injection using the trapezoidal rule. The 5-h AUCs corresponding to the second and third injections were ‘corrected’ by subtracting the estimated residual AUC from the previous injection. This residual ‘tail’ was computed by first estimating the exponential decay of the very last 11 h of data (presumed to reflect the terminal disappearance), and then by applying this exponential decay rate, starting from the last-measured concentration relative to the previous injection. The data were analysed using proc mixed in SAS for Windows, version 8.2 [12] to compare the difference between meals. The model is as follows:
where AUC ij is the AUC for meal i and subject j, μ is the intercept, Meal i is the fixed coefficient of meal i, Subject j is the between-subject random effect and ε ij is the residuals.
Compartmental modelling
For all the following model analyses, the problem of the bias introduced by left-censoring when data below the LLoQ are not reported was solved by applying a previously described method [13].
Single-subject model estimation
Both Model 1 (‘fixed kinetics’, corresponding to Eqs. (1), (2), (3) with K a1=K a2=K a3=K a) and Model 2 (‘varying kinetics’, Eqs. (1), (2), (3)) were fitted individually on single-patient observations by nonlinear ordinary least squares. Starting values for the parameters were obtained in each case by a preliminary round of genetic algorithm generations [14]; the best value found was used as a starting point for local optimisation, performed with the nls (nonlinear least squares) procedure [15] from the R package [16]. Individual parameter estimates were averaged and their sample variance and standard deviation were computed.
Population model estimation
The data from all 20 subjects were analysed together using the original code written for the R package, when population parameter estimation via nonlinear mixed effects models was performed. A Laplacian approximated maximum likelihood estimation method was applied, as previously described [13].
For Model 1 (‘fixed kinetics’), all structural model parameters (K c, K a, K x, V) were considered to be the sum of a fixed effect (population mean) and an individually varying random effect, i.e. for a generic parameter θ,
where i=1, 2, ..., 20 refers to patient number i, \( \log \hat{\theta } \) is the estimated population mean in log-scale, and \(b_{i} \sim N{\left( {0,\sigma ^{2}_{{\log \theta }} } \right)}\), assumed to be independent for different i, is the corresponding random deviation of patient i from the population mean in log-scale.
For Model 2 (‘varying kinetics’), parameters K c, K x and V were treated as in Model 1, whereas for parameter K a, a second (nested) level of random effects was introduced to account for intra-individual variation of its value, depending on the injection:
where i=1, 2, …, 20 refers to patient number i, \( \log \widehat{K}_{{\text{a}}} \) is the estimated population mean in log-scale, \(b_{i} \sim N{\left( {0,\sigma ^{2}_{{\log K_{{{\text{a}},1}} }} } \right)}\), assumed to be independent for different i, is the (between-individual) random variation of patient i from the population mean in log-scale, and \(b_{{i,j}} \sim N{\left( {0,\sigma ^{2}_{{\log K_{{{\text{a}},2}} }} } \right)}\), assumed to be independent for different i or j and to be independent of b i , is the (within-individual) deviation for injection j=1, 2, 3 from the patient’s mean level in log-scale.
Results
The estimates for the non-compartmental data analysis, based on the log (AUC:dose) for different injections are presented in Table 1. The F-test shows that these ratios were significantly different between injections (p<0.0001), where the ratio from the third (dinner) injection is almost twice the ratio from the first (breakfast) injection.
Table 2 reports the summary statistics for single-subject fitting: both Model 1 (‘fixed kinetics’) and Model 2 (‘varying kinetics’) converged successfully for all subjects. The estimated absorption rates K a1, K a2 and K a3 from Model 2 do not differ substantially from the absorption rate K a in Model 1. The estimates of the K c differ markedly between the two models, which means that with regard to this parameter, model choice plays an important role. The estimates of K x and V are similar. The clearance is derived from the product of the estimated K x and V.
Table 3 reports the estimates of single-subject fitting for subjects 104 and 106, given to illustrate the differences between Models 1 and 2. While for subject 104 the three values of K a in Model 2 are markedly different (K a2>2K a1), for subject 106 the corresponding three K a values are rather similar. This translates into a poor fitting for Model 1 and subject 104 (Fig. 3a) and a better fitting for Model 1 and subject 106 (Fig. 3b).
Estimated curves from single-subject analysis for subject 104 (a, b) and subject 106 (c, d). Dashed lines, fixed K a throughout the three different meals; solid line, varied K a. In subject 106, both models fit the data well. Only Model 2 fits the data for subject 104. The parameter estimates for these two subjects are presented in Table 3
Tables 4 and 5 present the population parameter estimates for Model 1 and Model 2, respectively. The extra column in Table 5 contains the estimates of the nested standard deviation of the within-subject variation of log K a. A likelihood ratio test between Model 1 and Model 2 was highly significant (p<0.0001) and supports the improvement in goodness of fit obtained by adding a further level of random effects. For both population models, estimates of K a are close to those seen in tracer studies of the disappearance of 125I-labelled IAsp from the injection site [2, 17].
It should be noted that the within-subject variation on K a in Table 5 is only slightly smaller than the corresponding between-subject variation. This indicates that there is substantial variability of entry of IAsp insulin into plasma between different injections in the same subject.
The residuals plots, the normal Q–Q plot and the pairs plot for the random effects of the population Model 2 are shown in Fig. 4. The residuals plot does not show any systematic pattern except for the subset of below LLoQ observations. For data reported below LLoQ, pseudo-residuals were calculated using a previously described method [13]. When the predicted values were smaller than the LLoQ, both positive and negative standardised pseudo-residuals were plotted, since the sign of the difference (observed–predicted) is unknown. When the predicted values were larger than LLoQ, only the negative standardised pseudo-residuals were plotted. Apart from a few outliers, the normal Q–Q plot shows a very good adaptation of the measured residuals to a normal distribution.
The random effects were all assumed to be independent of each other. Each pairs plot shows the scatter of the random effects of one parameter versus the random effects of another parameter. For most pairs of random effects, there is no indication of correlation between the parameters, even though the lack of correlation between K c and K x could arguably be due to the presence of two outliers.
Discussion
In the past the most frequently used approach to the study of the pharmacokinetics of s.c. insulin preparations has been based on AUC, Tmax and Cmax [3, 4]. More recently, compartmental models have also been used to interpret time–serum concentration data [18–21]. Confidence in the ability of such models to represent and explain observed data varies. Thus after studying several models, it was concluded [18] that the insulin absorption process from s.c. depots depends to such a high degree on external factors that no simple model may be employed to compare different preparations. Conversely, the analysis of s.c. injection and s.c. infusion data [19] supported a very detailed model of insulin absorption, including delay, saturation process and dimers–monomers equilibrium. Previous modelling work, however, only considered a single injection for each subject. Common clinical experience, however, is that multiple injections on the same subject often exhibit varying effects (between-day as well as within-day), possibly depending on the time of the day or on the site of injection. The approach followed in the present paper has been to hypothesise a single, robust structural kinetic model, extended to allow the kinetic parameters to vary with multiple injections within the same subject.
The preliminary analysis of AUC:dose ratios indicated that they were different between injections. If the pharmacokinetics of s.c. injected insulin were approximately constant for multiple injections within each subject, the log (AUC:dose) would also be relatively constant. It is to be noticed that bioavailability does not appear to be inversely proportional to the dose, since AUC from the third (evening) injection is more than twice the AUC from the first (morning) injection, while the ratio between the doses is 4:3. It is therefore appropriate that modelling of multiple injections should take this variability into account.
As a reference model, we studied Model 1 as detailed in Eqs. (1), (2), (3). Since K c expresses a chemical process at the site of injection, and K x expresses whole-body insulin elimination rate, the transfer rate constant that we hypothesised to be most likely to vary was K a, the absorption rate of soluble insulin from the s.c. depot. In order to express intra-subject variability in the kinetics that was due to changes in K a, two alternative representations could be used. Firstly, it could be supposed that, due to life-style (physical activity or other) changes throughout the day or to other circadian influences, K a actually depends merely on the time of the day, irrespective of injection site. Secondly, it could be supposed that the determining factor for the differences in kinetics is the site of injection, irrespective of time. The difference between these two approaches lies essentially in the K a attributed to the ‘tail’ of insulin absorption from previous injections: in the first case, at any given time, all insulin from all remaining depots is absorbed at the same (time-dependent) rate; in the second, insulin coming from a given s.c. depot is absorbed at a rate depending on the site of injection, irrespective of time. Clearly, a very substantial confounding effect is present, since each site is, for most of the insulin it delivers, associated with a given time of injection (morning, afternoon or evening). Both representations above were actually implemented and fitted to data for single subjects. A comparison of the residual sums of squares using the Wilcoxon sign-rank test revealed no significant difference. Although it cannot be ruled out that the variation is due to the time of the day, many investigations of the disappearance of insulin at the injection site have shown that it is affected by factors such as the thickness of the adipose tissue at the injection site, volume injected, blood flow, depth of the injection, etc [10]. In theory, plasma clearance could vary, but this is considered less likely than variations in absorption.
Slightly more complicated models have also been considered, with elimination rates from the protamine insulin crystals and/or the soluble insulin compartments. These models allow less than 100% relative bioavailability of the crystallised versus the soluble component, but their parameters are not simultaneously identifiable due to over-parameterisation with respect to the available data set. Data from experiments including both s.c. and intravenous injections are needed to quantify absolute bioavailability, including local degradation.
In the end, therefore, Model 2, which considers variability between sites, was applied. The model fit for all subjects was good, with acceptably low coefficients of variation of the estimates for all parameters for all subjects. Individual graphs for individuals 104 and 106 (Fig. 3) illustrate the difference between the models. Population parameter estimates were obtained for Model 1 (Table 4) and Model 2 (Table 5), and the latter resulted in a significantly better fit to the observations. Moreover, the very small estimate of K c with Model 1 (~T 1/2=20–30 h) indicates model misspecification.
The disappearance rates for IAsp (K x) presented in Tables 2, 4 and 5 are very low, but these estimates should be judged together with the very large estimates for the apparent volume of distribution. The clearance rates (V K x) reported are close to those reported for human insulin and IAsp [3, 22]. The reason for the poor separate estimation of K x and V is probably due to the relatively slow variation in insulin appearance, compared to the well-known short half-life of insulin in plasma.
Insulin antibodies will presumably be present in the majority of patients treated with human insulin or IAsp [23]. However, the antibody-bound fraction appears to be relatively small (10–20%), and it is an open question how this binding influences the ELISA measurements of IAsp. The modelling describes the kinetics of the IAsp measured by the assay, which, in addition to free IAsp, may also include a variable fraction of the bound IAsp. Thus part of the variability in the kinetics between patients might be due to the variability in antibody binding. This would also cover possible effects on absorption due to insulin antibodies.
The population parameter estimates are consistent with what was observed in other published series [3, 24], e.g. K a in Table 5 is of the same magnitude as the disappearance rate of 125I-labelled IAsp after s.c. injection in normal volunteers in [17]. The importance of the present study is that the within-subject variability of the absorption rate (K a) was quantified and appears to be of the same order of magnitude as the between-subject variability (\(\sigma _{{\log K_{{{\text{a}},1}} }}\) [between]=0.6; \(\sigma _{{\log K_{{{\text{a}},2}} }}\) [within]=0.4; see Table 5).
An exploratory analysis, which considered fixed effects for the injection and random effects for subjects, showed population estimates (K a1=0.0065; K a2=0.0083; K a3=0.0087) that are consistent with the observed disparity in log (AUC:dose). These results, if confirmed by a suitably designed experiment, could explain the widespread clinical impression of a relatively high level of insulin resistance in the morning [25, 26] as (partly) due to a reduced absorption rate. Also, it is to be noted that such a phenomenon does not appear to be due to reduced clearance, since a smaller AUC is observed in the morning.
In comparison with the usual basal/bolus insulin regimen, where a single evening injection of long-acting insulin is given together with meal-time injection of fast-acting insulin, it is conceivable that meal-time injections of biphasic insulin may exhibit less variability due to the smoothing of absorption of the long-acting component from the different sites. A disadvantage might be that the ratio between slow-acting and fast-acting insulin is fixed to the mixture ratio. However, simulation studies [2] have shown that meal-time injection of the 30/70 mixture of IAsp was able to mimic the insulin profiles seen in normal subjects.
The novel result of this study is that within-subject variation in the kinetics of s.c. administered insulin is far more substantial than hitherto thought, and may not simply be explained as measurement error. It is important to quantify the variation within patients in order to assess the (unavoidable) variability associated with various intensified injection regimens. This could be one explanation for the difficulty of tailoring intensified insulin therapy to the individual patient. Once this effect has been accounted for, it will be possible to design more powerful experiments for the future study of insulin preparations and injection regimens in order to achieve better blood glucose control.
Abbreviations
- Cmax :
-
maximum concentration
- IAsp:
-
insulin aspart
- LLoQ:
-
lower limit of quantification
- Tmax :
-
time to Cmax
References
The diabetes control and complications trial research group (1993) The effect of intensive treatment of diabetes on the development and progression of long term complications in insulin-dependent diabetes mellitus. N Engl J Med 329:977–986
Brange J, Vølund A (1999) Insulin analogs with improved pharmacokinetic profiles. Adv Drug Deliv Rev 35:307–335
Lindholm A, Jacobsen JV (2001) Clinical pharmacokinetics and pharmacodynamics of insulin aspart. Clin Pharmacokinet 40:641–659
Kaku K, Matsuda M, Urae A, Irie S (2000) Pharmacokinetics and pharmacodynamics of insulin aspart a rapid-acting analog of human insulin in healthy Japanese volunteers. Diabet Res Clin Pract 49:119–126
Chen J-W, Lauritsen T, Christiansen JJ, Jensen LH, Clausen WHO, Christiansen JS (2005) Pharmacokinetic profiles of biphasic insulin aspart 30/70 and 70/30 in patients with type 1 diabetes: a randomized double-blinded crossover study. Diabet Med 22:273–277
Brange J, Ribel U, Hansen JF et al (1988) Monomeric insulins obtained by protein engineering and their medical implications. Nature 333:679–682
Brange J (1997) The new era of biotech insulin analogues. Diabetologia 40 (Suppl 2):S48–S53
Jacobsen LV, Søgaard B, Riis A (2000) Pharmacokinetics and pharmacodynamics of a premixed formulation of soluble and protamine-retarded insulin aspart. Eur J Clin Pharmacol 56:399–403
Vølund A, Brange J, Drejer K et al (1991) In vitro and in vivo potency insulin analogues designed for clinical use. Diabet Med 8:839–847
Binder C, Lauritzen T, Faber O, Pramming S (1984) Insulin pharmacokinetics. Diabetes Care 7:188–199
Wenk RE (1998) Mechanism of interference by hemolysis in immunoassays and requirements for sample quality. Clin Chem 44:2554
Littell RC, Milliken GA, Stroup WW, Wolfinger RD (1996) SAS system for mixed models. Cary, SAS Institute
Clausen WHO, Tabanera R, Dalgaard P (2005) Solving the bias problem in pharmacokinetic data. Research Report 05/05. University of Copenhagen, Denmark
Goldberg DE (1989) Genetic algorithms in search, optimization, and machine learning. Addison-Wesley, Reading
Bates DM, Watts DG (1988) Nonlinear regression analysis and its applications. Wiley, New York
R Development Core Team (2004) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, http://www.R-project.org
Kang S, Brange J, Burch A, Vølund A, Owens DR (1991) Subcutaneous insulin absorption explained by insulin’s physiochemical properties—evidence from absorption studies of soluble human insulin and insulin analogues in humans. Diabetes Care 14:1057–1065
Nucci G, Cobelli C (2000) Models of subcutaneous insulin kinetics. A critical review. Comput Methods Programs Biomed 62:249–257
Wilinska ME, Chassin LJ, Schaller HC, Schaupp L, Pieber TR, Hovorka R (2005) Insulin kinetics in type 1 diabetes. Continuous and bolus delivery of rapid acting insulin. IEEE Trans Biomed Eng 52:3–12
Kobayashi T, Sawano T, Itoh T, Kosaka K, Hirayama H, Kasuya Y (1983) The pharmacokinetics of insulin after continuous subcutaneous infusion or bolus subcutaneous injection in diabetic patients. Diabetes 32:331–336
Mosekilde E, Jensen KS, Binder C, Pramming S, Thorsteinsson B (1989) Modeling absorption kinetics of subcutaneous injected soluble insulin. J Pharmacokinet Biopharm 17:67–87
Robinson RTCE, Harris, ND, Ireland RH, Lindholm A, Heller SR (2003) Comparative effect of human soluble insulin and insulin aspart upon hypoglycaemia-induced alterations in cardiac repolarization. Br J Clin Pharmacol 55:246–251
Lindholm A, Jensen LB, Home PD, Raskin P, Boehm BO, Råstam J (2002) Immune responses to insulin aspart and biphasic insulin aspart in people with type 1 and type 2 diabetes. Diabetes Care 25:876–882
Heinemann L (2002) Variability of insulin absorption and insulin action. Diabetes Technol Ther 4:673–682
Perriello G, De Feo P, Torlone E et al (1991) The dawn phenomenon in type 1 (insulin-dependent) diabetes mellitus: magnitude, frequency, variability, and dependency on glucose counterregulation and insulin sensitivity. Diabetologia 34:21–28
Holl RW, Heinze E (1992) Dawn or Somogyi phenomenon? High morning fasting blood sugar levels in juvenile type 1 diabetics. Deutsche Medizinische Wochenschrift 117:1503–1507 (German)
Acknowledgements
The authors are grateful to J. S. Christiansen and J.-W. Chen for carrying out the clinical trial [5] that allowed us to perform this research. This research was supported by The Danish Ministry of Science, Technology and Innovation, and Novo Nordisk.
Duality of interest
W. H. O. Clausen has received educational grant support from Novo Nordisk. A. Vølund is an employee at Novo Nordisk A/S. W. H. O. Clausen and A. Vølund are shareholders of Novo Nordisk.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Clausen, W.H.O., De Gaetano, A. & Vølund, A. Within-patient variation of the pharmacokinetics of subcutaneously injected biphasic insulin aspart as assessed by compartmental modelling. Diabetologia 49, 2030–2038 (2006). https://doi.org/10.1007/s00125-006-0327-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-006-0327-z