Abstract
Aims/hypothesis
Circulating levels of adiponectin are negatively associated with multiple indices of insulin resistance, and the concentration is reduced in humans with insulin resistance and type 2 diabetes. However, the mechanisms by which adiponectin improves insulin sensitivity remain unclear.
Subjects and methods
Combining euglycaemic–hyperinsulinaemic clamp studies with indirect calorimetry and skeletal muscle biopsies, we examined the relationship between plasma adiponectin and parameters of whole-body glucose and lipid metabolism, and muscle glycogen synthase (GS) activity in 51 Caucasians (ten lean, 21 obese and 20 with type 2 diabetes).
Results
Plasma adiponectin was significantly reduced in type 2 diabetic compared with obese and lean subjects. In lean and obese subjects, insulin significantly reduced plasma adiponectin, but this response was blunted in patients with type 2 diabetes. Plasma adiponectin was positively associated with insulin-stimulated glucose disposal (r=0.48), glucose oxidation (r=0.54), respiratory quotient (r=0.58) and non-oxidative glucose metabolism (r=0.38), and negatively associated with lipid oxidation during insulin stimulation (r=−0.60) after adjustment for body fat (all p<0.01). Most notably, we found a positive association between plasma adiponectin and insulin stimulation of GS activity in skeletal muscle (r=0.44, p<0.01).
Conclusions/interpretation
Our results indicate that plasma adiponectin may enhance insulin sensitivity by improving the capacity to switch from lipid to glucose oxidation and to store glucose as glycogen in response to insulin, and that low adiponectin may contribute to impaired insulin activation of GS in skeletal muscle of patients with type 2 diabetes.
Similar content being viewed by others
Introduction
Adiponectin is a novel adipocyte-specific protein, which is present abundantly in the circulation in humans [1]. In contrast to other adipokines, such as leptin, TNF-α and resistin, adiponectin levels are decreased in obesity [1–3], and show a strong negative correlation with multiple indices of insulin resistance in humans in vivo [2–8]. In patients with type 2 diabetes, adiponectin levels are further reduced [2, 3], and low plasma adiponectin predicts a decline in insulin sensitivity and the future development of type 2 diabetes [9, 10]. Furthermore, treatment of type 2 diabetes with thiazolidinediones seems to involve increased secretion of adiponectin from adipose tissue in response to activation of peroxisome proliferator-activated receptor-γ [3, 8, 11]. While further studies are needed to establish the pathophysiological role of reduced plasma adiponectin in type 2 diabetes, these data support the hypothesis that adiponectin may be a key regulator of insulin sensitivity and energy metabolism [1].
The physiological and molecular mechanisms underlying the insulin-sensitising effect of adiponectin in vivo remain to be fully clarified, but studies in rodents and cell cultures indicate that adiponectin stimulates fatty acid oxidation and glucose uptake in muscle [12–15], and augments insulin-mediated suppression of hepatic glucose output [16, 17]. These effects may be mediated by the binding of adiponectin to one of two recently identified adiponectin receptors, termed AdipoR1 and AdipoR2 [18], and subsequent activation of AMP-activated protein kinase (AMPK) and downstream signalling molecules [12, 13, 19]. Chronic pharmacological activation of AMPK in rodents improves not only fatty acid oxidation and glucose uptake but also mitochondrial biogenesis in muscle [20, 21]. Furthermore, novel approaches such as magnetic resonance spectroscopy, gene expression profiling and proteome analysis of human skeletal muscle support a role for impaired mitochondrial oxidative phosphorylation and ATP synthesis in type 2 diabetes [22–25]. For these reasons, the hypothesis of blunted signalling along the adiponectin-AMPK signalling pathway in insulin resistance is attractive [1]. However, we and others have found normal AMPK activity and isoform protein expression in muscle biopsies from obese non-diabetic and type 2 diabetic subjects [26–28], which indicates that adiponectin may enhance insulin sensitivity by regulating signalling through alternative pathways. Correspondingly, adiponectin has been reported to augment insulin-mediated tyrosine phosphorylaton of the insulin receptor (IR) and IRS-1 in rodent skeletal muscle [14]. In addition, a cross-sectional study of lean, obese and type 2 diabetic individuals showed that low adiponectin levels were associated with a lower fold-increase in tyrosine phosphorylation of muscle IR in response to insulin [5]. Thus, there is evidence that low plasma adiponectin might interfere with insulin signalling, leading to impaired glucose transport and glycogen synthesis. Skeletal muscle is the major site of insulin resistance, and quantitatively impaired muscle glycogen synthesis is the major defect of insulin-stimulated glucose metabolism in type 2 diabetes [29]. Correspondingly, impaired insulin activation of muscle glycogen synthase (GS) is a consistent finding in patients with type 2 diabetes and high-risk individuals [29, 30]. Recently, an association between plasma adiponectin and insulin-stimulated non-oxidative glucose disposal was demonstrated in offspring of patients with type 2 diabetes [6]. Based on these findings we hypothesised that low adiponectin levels may contribute to impaired insulin activation of muscle GS in patients with type 2 diabetes.
To investigate possible mechanisms underlying the insulin-sensitising effect of adiponectin in humans in vivo, we examined the association of plasma adiponectin with measures of whole-body lipid and glucose metabolism and muscle GS activity in a cross-sectional population of lean, obese and type 2 diabetic subjects. Our investigations combined euglycaemic–hyperinsulinaemic clamp studies with indirect calorimetry and skeletal muscle biopsies.
Subjects and methods
Subjects
A total of 51 Caucasians participated in the study. This included ten healthy lean, 21 healthy obese and 20 obese type 2 diabetic subjects, who were consecutively enrolled for euglycaemic–hyperinsulinaemic clamp studies combined with skeletal muscle biopsies (Table 1). We have previously reported α1- and α2-AMPK activity, phosphorylation of AMPK on Thr172, and phosphorylation of acetyl CoA carboxylase (ACC) on Ser221 in skeletal muscle biopsies obtained from the first 20 participants enrolled in the present study (ten obese type 2 diabetic and ten obese control subjects, all males) [26]. Type 2 diabetic patients were treated by diet either alone or in combination with sulfonylurea, metformin or insulin, which were withdrawn 1 week prior to the study. The patients were all GAD65 antibody negative and without signs of diabetic retinopathy, nephropathy, neuropathy or macrovascular complications. All the control subjects had normal glucose tolerance and no family history of diabetes. However, on the clamp day, one lean and three obese control subjects showed fasting plasma glucose levels consistent with IFG. All subjects had normal results on screening blood tests of hepatic and renal function. All subjects were instructed to refrain from strenuous physical activity for a period of 48 h before the experiment. Informed consent was obtained from all subjects before participation. The study was approved by the Local Ethics Committee and was performed in accordance with the Helsinki Declaration.
Study design
All study subjects were admitted to the Diabetes Research Centre at Odense University Hospital, Denmark. After an overnight fast the subjects underwent a euglycaemic–hyperinsulinaemic clamp. After a 2-h basal tracer equilibration period, insulin was infused at a rate of 40 mU·m−2·min−1 for 4 h. A primed-constant [3-3H]glucose infusion was used throughout the 6-h study, and [3-3H]glucose was added to the glucose infusates to maintain plasma specific activity constant at baseline levels during the 4-h clamp period as described in detail previously [31]. Using this protocol, physiological hyperinsulinaemia at a serum insulin concentration of ∼400 pmol/l was obtained in all groups during the insulin-stimulated period. In type 2 diabetic subjects, plasma glucose was allowed to decline to ∼5.5 mmol/l during the initial part of the 4-h insulin infusion period before glucose infusion was initiated. Total glucose disposal rates (R d) were calculated using Steele’s non-steady-state equations adapted for labelled glucose infusates as described [31]. The distribution volume of glucose was taken as 200 ml/kg body weight and the pool fraction as 0.65. The studies were combined with indirect calorimetry using a flow-through canopy gas analyser system (Deltatrac; Datex, Helsinki, Finland). After an equilibration period of 10 min, the average gas exchange recorded over the two 30-min steady-state periods (basal and insulin-stimulated) were used to calculate the RQ and rates of glucose and lipid oxidation as previously described [32]. Rates of non-oxidative glucose metabolism (NOGM) were calculated as the difference between R d and glucose oxidation. Percent body fat was determined by the bioimpedance method.
Assays
Plasma adiponectin was determined by an in-house time-resolved immunofluorometric assay (TR-IFMA) based on commercial antibodies and recombinant human adiponectin (R&D Systems, Abingdon, UK) as recently described [33]. Adiponectin has a molecular mass of ∼30–36 kDa depending on the degree of glycosylation, but the molecule is known to form a wide range of polymers in vivo. The predominant polymers include trimers, hexamers and highly congregated multimers of ∼300 kDa. Both antibodies of the present assay were able to detect several adiponectin polymers in serum, including the three major molecular forms (data not shown). Within- and between-assay CV values of standards and unknown samples averaged <5 and 10%, respectively. Plasma glucose was measured at the bedside on a Beckman glucose analyser (Beckman Instruments, Fullerton, CA, USA) by the glucose oxidase method. Serum insulin and C-peptide were analysed by commercial TR-IFMAs (Perkin Elmer Life Sciences, Turku, Finland), and serum NEFA and triglycerides were measured by an enzymatic colorimetric method (Wako Chemicals, Neuss, Germany).
Muscle biopsies
Muscle biopsies were obtained from the vastus lateralis muscle before and after the 4-h insulin infusion period using a modified Bergström needle with suction under local anaesthesia (10–15 ml lidocaine 2% [20 g/l] injected s.c.). Muscle samples were immediately blotted free of blood, fat and connective tissue and frozen in liquid nitrogen within 20–30 s. The muscle samples were freeze-dried and dissected free of blood, fat and connective tissue before analysis of muscle enzyme activity, which was measured in muscle homogenates as described previously [30].
GS activity
GS activity was measured in homogenates by a method described by Richter et al [34]. GS activity was determined in the presence of 0.17 or 8 mmol/l glucose-6-phosphate and given as the percent of fractional velocity (FV) (100×activity in the presence of 0.17 mmol/l glucose-6-phosphate divided by the activity at 8 mmol/l glucose-6-phosphate).
Statistical analysis
Data calculation and statistical analysis were performed using the SPSS for Windows Version 10.0 program. Variables with skewed distribution (insulin and adiponectin) were logarithmically transformed for statistical analysis. Results are given as means±SEM. Differences between the groups were assessed with one-way ANOVA and Tukey’s post hoc testing. Differences within groups were evaluated using Student’s t-test for paired data. The relationships between plasma adiponectin and continuous variables were examined by calculation of Pearson’s correlation coefficients, and partial correlation was used to examine relationships between plasma adiponectin and continuous variables, independently of percent body fat. Significance was accepted at the p≤0.05 level.
Results
Characteristics
Anthropometric and biochemical characteristics of the study subjects are shown in Table 1. The lean subjects had significantly lower BMI and percent body fat, and significantly higher plasma HDL cholesterol than obese subjects and type 2 diabetic patients. Fasting levels of plasma glucose, plasma triglycerides, HbA1c, serum insulin and C-peptide were significantly higher in type 2 diabetic patients than in lean and obese subjects. Serum insulin and C-peptide levels were also significantly higher in obese than in lean subjects (Table 1).
Metabolic studies
Metabolic characteristics of the study subjects are shown in Table 2. Basal R d were significantly higher in type 2 diabetic patients than in obese subjects, whereas basal serum NEFA and basal rates of glucose oxidation, NOGM, RQ and lipid oxidation were similar in the three groups. In the insulin-stimulated state, R d, glucose oxidation, NOGM and RQ were significantly reduced, and lipid oxidation and serum NEFA were significantly increased in type 2 diabetic patients compared with obese and lean subjects. Except for NOGM and serum NEFA the same differences were seen between obese and lean subjects.
Plasma adiponectin
Basal plasma adiponectin levels were significantly lower in patients with type 2 diabetes (5.7±0.5 mg/l) than in obese (8.7±1.1 mg/l; p=0.05) and lean (10.6±1.6 mg/l; p=0.008) subjects (Fig. 1a). There was no difference between lean and obese subjects (p=0.45). The administration of insulin in physiological concentrations over 4 h caused a small but significant reduction in plasma adiponectin levels in lean (7.9%; p<0.001) and obese (5.1%; p<0.001) subjects. In patients with type 2 diabetes, the insulin-mediated suppression of plasma adiponectin was not significant (2.2%; p=0.08). The insulin-mediated decrease in plasma adiponectin was significantly impaired in type 2 diabetic subjects compared with lean subjects, but not when compared with obese subjects (Fig. 1b).
Plasma adiponectin levels (a, b) and glycogen synthase activity given as percent fractional velocity (GS FV) (c, d) at basal (white bars) and at the end (black bars) of a 4-h 40 mU·m−2·min−1 euglycaemic–hyperinsulinaemic clamp in ten lean, 21 obese and 20 type 2 diabetic subjects. The percentage decrease in plasma adiponectin levels (b) and the incremental increase in GS FV (Δ-GS FV) over basal (d) in response to insulin infusion are shown for lean (white bars), obese (grey bars) and type 2 diabetic subjects (black bars). Data are means±SEM. *p<0.01 vs lean subjects; #p<0.05 vs obese subjects; §p<0.001 vs basal
GS activity
In the basal state there was no difference between the three groups in GS FV activity (Fig. 1c). Insulin infusion significantly increased GS FV activity in lean and obese subjects (both p<0.001), but not in patients with type 2 diabetes (p=0.16). In the insulin-stimulated state GS FV activity was significantly lower in type 2 diabetic and obese subjects compared with lean subjects (Fig. 1c). Furthermore, insulin-stimulated GS FV activity was significantly lower in patients with type 2 diabetes compared with obese subjects (Fig. 1c). The increase in GS FV activity (Δ-GS FV) induced by insulin was significantly lower in patients with type 2 diabetes compared with obese and lean subjects, and also in obese compared with lean subjects (Fig. 1d).
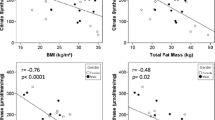
Adiponectinaemia in relation to metabolic parameters
To explore possible mechanisms underlying the insulin-sensitising effect of circulating adiponectin in humans in vivo, we examined the relationship between basal plasma adiponectin and insulin action on whole-body parameters of lipid and glucose metabolism after adjustment for percent body fat. Basal plasma adiponectin was positively associated with insulin-stimulated values of R d, glucose oxidation, NOGM and RQ, and negatively associated with lipid oxidation and serum NEFA during insulin stimulation (Fig. 2a–d). In the subgroup of male subjects (n=38) these relationships remained significant (Fig. 2a–d).
The relationship of basal plasma adiponectin with rates (mg·m−2·min−1) of (a) total glucose disposal (R d), (b) glucose oxidation, (c) non-oxidative glucose metabolism (NOGM) and (d) lipid oxidation, as well as (e) respiratory quotient (RQ) and (f) serum NEFA at the end of a 4-h 40 mU·m−2·min−1 euglycaemic–hyperinsulinaemic clamp in a cross-sectional population of ten lean (triangles), 21 obese (open circles) and 20 type 2 diabetic subjects (closed circles). Correlation coefficients were adjusted for percent body fat and are given for the total population (r) and male subjects alone (r′) (n=38)
To study the potential role of insulin-mediated suppression of plasma adiponectin with respect to insulin sensitivity, we also examined the relationship between the relative decrease in plasma adiponectin (clamp adiponectin divided by basal adiponectin) and these parameters of insulin action after adjustment for percent body fat. The relative decrease in plasma adiponectin correlated positively with insulin-stimulated values of R d (r=0.32; p=0.02), glucose oxidation (r=0.40; p=0.005) and RQ (r=0.39; p=0.008), and negatively with lipid oxidation (r=−0.38; p=0.008) during insulin stimulation, whereas no significant relationship with NOGM (r=0.22; p=0.14) or serum NEFA (r=−0.24; p=0.09) was observed.
Adiponectinaemia in relation to GS and AMPK activity
To gain insight into potential molecular mechanisms by which plasma adiponectin increases skeletal muscle insulin sensitivity, we examined the relationship between plasma adiponectin and muscle GS activity (Table 3). There was no association between plasma adiponectin and GS FV activity in the basal state. In contrast, basal plasma adiponectin was positively associated with GS FV activity in the insulin-stimulated state as well as with Δ-GS FV activity both before (not shown) and after adjusting for percent body fat (Fig. 3a). The relative decrease in plasma adiponectin also correlated significantly with Δ-GS FV activity before (r=0.32; p=0.026) but not significantly after correction for percent body fat (Table 3).
The relationship of basal plasma adiponectin with (a) the incremental increase of glycogen synthase fractional velocity over basal in response to insulin infusion (Δ-GS FV) in a cross-sectional population of ten lean (triangles), 21 obese (open circles) and 20 type 2 diabetic subjects (closed circles), and (b) with basal α2-AMPK activity in a subset of ten obese (squares) non-diabetic subjects. Correlation coefficients were adjusted for percent body fat
The first 20 of 51 subjects enrolled in the present study consisted of ten obese non-diabetic and ten obese type 2 diabetic male subjects. In these subjects we have previously reported α1- and α2-AMPK activity, phosphorylation of AMPK on Thr172, and phosphorylation of ACC on Ser221 [26]. In this subpopulation of male subjects, basal plasma adiponectin also correlated significantly with Δ-GS FV activity (r=0.53; p=0.02 adjusted for percent body fat) and tended to correlate with insulin-stimulated values of GS FV activity (r=0.44; p=0.060 adjusted for percent body fat). Basal plasma adiponectin showed no relationship with either α1- or α2-AMPK activity, phosphorylation of α-AMPK on Thr172 or phosphorylation of ACC on Ser221 in the total subpopulation. However, in the subgroup of obese non-diabetic subjects, in which the correlation between plasma adiponectin and Δ-GS FV activity was conserved (r=0.69; p=0.04 adjusted for percent body fat), we found a significant positive correlation between plasma adiponectin and α2-AMPK activity (r=0.87; p=0.002 adjusted for percent body fat) (Fig. 3b).
Discussion
The most important finding of the present study was the relationship between plasma adiponectin and insulin activation of GS in skeletal muscle. This provides a possible explanation at the molecular level for the association between plasma adiponectin and insulin-stimulated NOGM, which was recently reported in offspring of patients with type 2 diabetes [6], and now confirmed by us in a cross-sectional population of middle-aged subjects. Consistent with earlier reports [2–6, 8], we found a positive association between plasma adiponectin and insulin-stimulated R d. Moreover, we report that plasma adiponectin correlates positively with glucose oxidation and negatively with lipid oxidation during insulin stimulation. This is supported by the finding of a close positive association between plasma adiponectin and insulin-stimulated RQ, which reflects the capacity to switch from lipid to glucose oxidation, also termed metabolic flexibility. These observations extend those previously reported in young individuals with or without a family history of type 2 diabetes [4, 6]. Taken together our results indicate that the insulin-sensitising effect of plasma adiponectin involves an improved capacity to switch from lipid to glucose oxidation and to store glucose as glycogen in response to insulin, and that low plasma adiponectin in type 2 diabetes may contribute to insulin resistance by interfering with insulin action on GS in skeletal muscle.
The demonstration of a relationship between basal plasma adiponectin and the capacity of insulin to stimulate GS in skeletal muscle is a novel finding of the present study. This suggests that low adiponectin levels may contribute to impaired insulin activation of muscle GS, which represents a consistent molecular abnormality in skeletal muscle insulin resistance in individuals with obesity, type 2 diabetes or a family history of diabetes [29, 30], as well as human cultured myotubes obtained from patients with type 2 diabetes [35]. The mechanism by which plasma adiponectin interferes with insulin activation of GS could involve modulation of proximal insulin signalling components or of GS itself. Thus, in rodents the administration of adiponectin enhances insulin-stimulated tyrosine phosphorylation of the IR and IRS-1 in muscle [14], and in humans plasma adiponectin was associated with insulin-stimulated tyrosine phosphorylation of IR [5]. On the other hand, we and others have found normal distal insulin signalling through Akt and GS kinase-3 despite impaired insulin activation of GS in skeletal muscle of patients with type 2 diabetes and myotubes established from such subjects [30, 36–38]. Thus, it is possible that the negative effect of low adiponectin is mediated directly by, for example, lipid- and stress-activated kinases on GS, or through as yet unknown signalling intermediates by interfering with insulin-mediated dephosphorylation of GS.
Circulating adiponectin is predominantly present as trimers, hexamers and high molecular weight (HMW) forms [1]. Currently available clinical data support the hypothesis that HMW adiponectin is the most physiologically relevant form [39, 40]. Only HMW adiponectin shows the same strong associations with parameters of insulin sensitivity as total adiponectin [39]. This is thought to indicate that most of the reported relationships are explained largely by HMW adiponectin. It is likely that this includes the observed relationship between total adiponectin and insulin-stimulated NOGM and GS in the present study. However, further studies are warranted to explore the direct molecular mechanisms by which these forms of circulating adiponectin sensitise muscle to insulin action. Females have higher circulating levels of total adiponectin, and in particular the proportion of HMW and hexameric adiponectin, than do males [1, 40, 41]. A selective inhibition of the secretion of HMW adiponectin by testosterone may contribute to these differences [42]. The finding that the associations between plasma adiponectin and measures of glucose and lipid metabolism as well as insulin activation of GS remained intact in male subjects, excludes the possibility that these relationships were due to the larger variation in adiponectin induced by this sexual dimorphism.
Using systemic indirect calorimetry, we found a reduced insulin-stimulated RQ in type 2 diabetes and to a lesser extent in obesity, and showed that the magnitude of this response correlated positively with plasma adiponectin. These results suggest a role for plasma adiponectin in metabolic flexibility. Our data reflect whole-body substrate oxidation, which makes it impossible to estimate the relative contribution of insulin-sensitive tissues such as liver, fat and muscle to this relationship. The finding of a strong inverse association between plasma adiponectin and the ability of insulin to suppress serum NEFA levels may indicate a role for adiponectin in sensitising adipocytes to the antilipolytic effect of insulin, and this could at least in part explain the observed association between adiponectin and insulin-mediated suppression of whole-body lipid oxidation. On the other hand, measurement of RQ across the tissue bed of the leg has shown that metabolic inflexibility represents a characteristic feature of skeletal muscle insulin resistance in type 2 diabetes and obesity [43]. Therefore, it cannot be excluded that the observed relationship between plasma adiponectin and insulin-stimulated RQ also applies to skeletal muscle.
There is experimental evidence that globular adiponectin stimulates lipid oxidation in human myotubes [12] and rodent skeletal muscle [13–15], and that this is mediated by activation of AMPK [1, 12, 19], which has been shown to induce mitochondrial biogenesis [20, 21]. Our finding of an association between plasma adiponectin and muscle α2-AMPK activity in a small group of non-diabetic obese subjects, and a preliminary report of similar findings in patients with type 2 diabetes [44], provide correlative support for these mechanisms. However, in the present study this relationship was absent in the total subpopulation of healthy and type 2 diabetic obese male subjects. In addition, reduced basal lipid oxidation in muscle, metabolic inflexibility and lower plasma adiponectin levels in type 2 diabetes and obesity are not reflected in lower AMPK activity or altered protein expression of AMPK isoforms in vivo compared with healthy lean subjects [26–28]. Moreover, exercise-induced improvement of insulin sensitivity, which is associated with increased AMPK activity in both healthy and type 2 diabetic subjects [28, 45], is not paralleled by increased plasma adiponectin [46, 47]. Thus, there is no simple relationship between plasma adiponectin, AMPK activity and insulin sensitivity in skeletal muscle, and further studies are needed to establish the role of adiponectin in metabolic flexibility and mitochondrial function, and to what extent AMPK is involved. This also suggests that adiponectin by its binding to AdipoR1 or AdipoR2 may regulate other pathways in order to mediate its insulin-sensitising effect in skeletal muscle.
Another interesting finding of our study was that the relative decrease in plasma adiponectin in response to physiological hyperinsulinaemia for 4 h was blunted in patients with type 2 diabetes. Other groups have speculated that the suppression of plasma adiponectin in response to physiological hyperinsulinaemia for 3–5 h might reflect the relationship between hypoadiponectinaemia and chronic hyperinsulinaemia [3, 48]. For several reasons this explanation appears unlikely. Thus, in addition to the blunted response in type 2 diabetic subjects, we found that the insulin-mediated suppression of plasma adiponectin was in fact associated with improved insulin action on R d, glucose oxidation, RQ and lipid oxidation. Also, the decrease in plasma adiponectin during physiological hyperinsulinaemia actually parallels the finding of sustained activation of glucose metabolism and insulin signalling molecules in response to insulin infusion for 3–4 h in humans [30, 36, 49], and insulin infusion for even longer periods (8 h) improves mitochondrial ATP production [50]. As with the ability of insulin to decrease plasma adiponectin, these actions of insulin are impaired in patients with type 2 diabetes, and are thought to contribute to insulin resistance [30, 50]. Therefore, our data suggest that insulin-mediated suppression of adiponectin may have a physiological role, which may be beneficial rather than simply reflecting the effect of chronic hyperinsulinaemia. Our data, however, cannot demonstrate a cause and effect relationship, and further studies are warranted to determine the physiological relevance of this response.
In summary, we demonstrated a relationship between plasma adiponectin and insulin action on glucose metabolism (oxidation and storage) and lipid oxidation. This was reflected in a relationship between plasma adiponectin and the ability of insulin to switch from mainly lipid to glucose oxidation. These findings, although only correlative in nature, indicate that low adiponectin levels may play a role in the metabolic inflexibility associated with insulin resistance in type 2 diabetes and obesity. Most importantly, we hypothesised and demonstrated an association between plasma adiponectin and insulin activation of GS in skeletal muscle. This finding, for the first time, provides a potential explanation at the molecular level for the insulin-sensitising effect of plasma adiponectin, and suggests that therapeutic strategies that raise plasma adiponectin levels would alleviate one of the most consistent defects in skeletal muscle insulin resistance of patient with type 2 diabetes, namely impaired insulin activation of GS.
Abbreviations
- ACC:
-
acetyl CoA carboxylase
- AMPK:
-
AMP-activated protein kinase
- FV:
-
fractional velocity
- GS:
-
glycogen synthase
- IR:
-
insulin receptor
- NOGM:
-
non-oxidative glucose metabolism
- Rd :
-
glucose disposal rates
- TR-IFMA:
-
time-resolved immunofluorometric assay
References
Kadowaki T, Yamauchi T (2005) Adiponectin and adiponectin receptors. Endocr Rev 26:439–451
Weyer C, Funahashi T, Tanaka S et al (2001) Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia. J Clin Endocrinol Metab 86:1930–1935
Yu JG, Javorschi S, Hevener AL et al (2002) The effect of thiazolidinediones on plasma adiponectin levels in normal, obese, and type 2 diabetic subjects. Diabetes 51:2968–2974
Tschritter O, Fritsche A, Thamer C et al (2003) Plasma adiponectin concentrations predict insulin sensitivity of both glucose and lipid metabolism. Diabetes 52:239–243
Stefan N, Vozarova B, Funahashi T et al (2002) Plasma adiponectin concentration is associated with skeletal muscle insulin receptor tyrosine phosphorylation, and low plasma concentration precedes a decrease in whole-body insulin sensitivity in humans. Diabetes 51:1884–1888
Salmenniemi U, Zacharova J, Ruotsalainen E et al (2005) Association of adiponectin level and variants in the adiponectin gene with glucose metabolism, energy expenditure, and cytokines in offspring of type 2 diabetic patients. J Clin Endocrinol Metab 90:4216–4223
Stefan N, Stumvoll M, Vozarova B et al (2003) Plasma adiponectin and endogenous glucose production in humans. Diabetes Care 26:3315–3319
Bajaj M, Suraamornkul S, Piper P et al (2004) Decreased plasma adiponectin concentrations are closely related to hepatic fat content and hepatic insulin resistance in pioglitazone-treated type 2 diabetic patients. J Clin Endocrinol Metab 89:200–206
Spranger J, Kroke A, Mohlig M et al (2003) Adiponectin and protection against type 2 diabetes mellitus. Lancet 361:226–228
Lindsay RS, Funahashi T, Hanson RL et al (2002) Adiponectin and development of type 2 diabetes in the Pima Indian population. Lancet 360:57–58
Combs TP, Wagner JA, Berger J et al (2002) Induction of adipocyte complement-related protein of 30 kilodaltons by PPARgamma agonists: a potential mechanism of insulin sensitization. Endocrinology 143:998–1007
Chen MB, McAinch AJ, Macaulay SL et al (2005) Impaired activation of AMP-kinase and fatty acid oxidation by globular adiponectin in cultured human skeletal muscle of obese type 2 diabetics. J Clin Endocrinol Metab 90:3665–3672
Yamauchi T, Kamon J, Minokoshi Y et al (2002) Adiponectin stimulates glucose utilization and fatty-acid oxidation by activating AMP-activated protein kinase. Nat Med 8:1288–1295
Yamauchi T, Kamon J, Waki H et al (2001) The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat Med 7:941–946
Fruebis J, Tsao TS, Javorschi S et al (2001) Proteolytic cleavage product of 30-kDa adipocyte complement-related protein increases fatty acid oxidation in muscle and causes weight loss in mice. Proc Natl Acad Sci USA 98:2005–2010
Combs TP, Berg AH, Obici S, Scherer PE, Rossetti L (2001) Endogenous glucose production is inhibited by the adipose-derived protein Acrp30. J Clin Invest 108:1875–1881
Berg AH, Combs TP, Du X, Brownlee M, Scherer PE (2001) The adipocyte-secreted protein Acrp30 enhances hepatic insulin action. Nat Med 7:947–953
Yamauchi T, Kamon J, Ito Y et al (2003) Cloning of adiponectin receptors that mediate antidiabetic metabolic effects. Nature 423:762–769
Tomas E, Tsao TS, Saha AK et al (2002) Enhanced muscle fat oxidation and glucose transport by ACRP30 globular domain: acetyl-CoA carboxylase inhibition and AMP-activated protein kinase activation. Proc Natl Acad Sci USA 99:16309–16313
Bergeron R, Ren JM, Cadman KS et al (2001) Chronic activation of AMP kinase results in NRF-1 activation and mitochondrial biogenesis. Am J Physiol Endocrinol Metab 281:E1340–E1346
Winder WW, Holmes BF, Rubink DS, Jensen EB, Chen M, Holloszy JO (2000) Activation of AMP-activated protein kinase increases mitochondrial enzymes in skeletal muscle. J Appl Physiol 88:2219–2226
Petersen KF, Dufour S, Befroy D, Garcia R, Shulman GI (2004) Impaired mitochondrial activity in the insulin-resistant offspring of patients with type 2 diabetes. N Engl J Med 350:664–671
Mootha VK, Lindgren CM, Eriksson KF et al (2003) PGC-1alpha-responsive genes involved in oxidative phosphorylation are coordinately downregulated in human diabetes. Nat Genet 34:267–273
Patti ME, Butte AJ, Crunkhorn S et al (2003) Coordinated reduction of genes of oxidative metabolism in humans with insulin resistance and diabetes: Potential role of PGC1 and NRF1. Proc Natl Acad Sci USA 100:8466–8471
Højlund K, Wrzesinski K, Larsen PM et al (2003) Proteome analysis reveals phosphorylation of ATP synthase beta-subunit in human skeletal muscle and proteins with potential roles in type 2 diabetes. J Biol Chem 278:10436–10442
Højlund K, Mustard KJ, Staehr P et al (2004) AMPK activity and isoform protein expression are similar in muscle of obese subjects with and without type 2 diabetes. Am J Physiol Endocrinol Metab 286:E239–E244
Steinberg GR, Smith AC, Van Denderen BJ et al (2004) AMP-activated protein kinase is not down-regulated in human skeletal muscle of obese females. J Clin Endocrinol Metab 89:4575–4580
Musi N, Fujii N, Hirshman MF et al (2001) AMP-activated protein kinase (AMPK) is activated in muscle of subjects with type 2 diabetes during exercise. Diabetes 50:921–927
Beck-Nielsen H, Vaag A, Poulsen P, Gaster M (2003) Metabolic and genetic influence on glucose metabolism in type 2 diabetic subjects-experiences from relatives and twin studies. Best Pract Res Clin Endocrinol Metab 17:445–467
Højlund K, Staehr P, Hansen BF et al (2003) Increased phosphorylation of skeletal muscle glycogen synthase at NH2-terminal sites during physiological hyperinsulinemia in type 2 diabetes. Diabetes 52:1393–1402
Hother-Nielsen O, Henriksen JE, Holst JJ, Beck-Nielsen H (1996) Effects of insulin on glucose turnover rates in vivo: isotope dilution versus constant specific activity technique. Metabolism 45:82–91
Frayn KN (1983) Calculation of substrate oxidation rates in vivo from gaseous exchange. J Appl Physiol 55:628–634
Saraheimo M, Forsblom C, Fagerudd J et al (2005) Serum adiponectin is increased in type 1 diabetic patients with nephropathy. Diabetes Care 28:1410–1414
Richter EA, Mikines KJ, Galbo H, Kiens B (1989) Effect of exercise on insulin action in human skeletal muscle. J Appl Physiol 66:876–885
Gaster M, Petersen I, Højlund K, Poulsen P, Beck-Nielsen H (2002) The diabetic phenotype is conserved in myotubes established from diabetic subjects: evidence for primary defects in glucose transport and glycogen synthase activity. Diabetes 51:921–927
Kim YB, Nikoulina SE, Ciaraldi TP, Henry RR, Kahn BB (1999) Normal insulin-dependent activation of Akt/protein kinase B, with diminished activation of phosphoinositide 3-kinase, in muscle in type 2 diabetes. J Clin Invest 104:733–741
Gaster M, Brusgaard K, Handberg A, Højlund K, Wojtaszewski JF, Beck-Nielsen H (2004) The primary defect in glycogen synthase activity is not based on increased glycogen synthase kinase-3alpha activity in diabetic myotubes. Biochem Biophys Res Commun 319:1235–1240
McIntyre EA, Halse R, Yeaman SJ, Walker M (2004) Cultured muscle cells from insulin-resistant type 2 diabetes patients have impaired insulin, but normal 5-amino-4-imidazolecarboxamide riboside-stimulated, glucose uptake. J Clin Endocrinol Metab 89:3440–3448
Lara-Castro C, Luo N, Wallace P, Klein RL, Garvey WT (2006) Adiponectin multimeric complexes and the metabolic syndrome trait cluster. Diabetes 55:249–259
Pajvani UB, Hawkins M, Combs TP et al (2004) Complex distribution, not absolute amount of adiponectin, correlates with thiazolidinedione-mediated improvement in insulin sensitivity. J Biol Chem 279:12152–12162
Peake PW, Kriketos AD, Campbell LV, Shen Y, Charlesworth JA (2005) The metabolism of isoforms of human adiponectin: studies in human subjects and in experimental animals. Eur J Endocrinol 153:409–417
Xu A, Chan KW, Hoo RL et al (2005) Testosterone selectively reduces the high molecular weight form of adiponectin by inhibiting its secretion from adipocytes. J Biol Chem 280:18073–18080
Kelley DE, Mandarino LJ (2000) Fuel selection in human skeletal muscle in insulin resistance: a reexamination. Diabetes 49:677–683
Bajaj M, Suraamornkul S, Sriwijilkamol A, Musi N, DeFronzo R (2005) Effects of PPAR-alpha and PPAR-gamma agonists on muscle AMPK activity in patients with type 2 diabetes. Diabetes 54(Suppl 1):A151 (Abstract)
Musi N, Yu H, Goodyear LJ (2003) AMP-activated protein kinase regulation and action in skeletal muscle during exercise. Biochem Soc Trans 31:191–195
Hulver MW, Zheng D, Tanner CJ et al (2002) Adiponectin is not altered with exercise training despite enhanced insulin action. Am J Physiol Endocrinol Metab 283:E861–E865
Yokoyama H, Emoto M, Araki T et al (2004) Effect of aerobic exercise on plasma adiponectin levels and insulin resistance in type 2 diabetes. Diabetes Care 27:1756–1758
Mohlig M, Wegewitz U, Osterhoff M et al (2002) Insulin decreases human adiponectin plasma levels. Horm Metab Res 34:655–658
Wojtaszewski JF, Hansen BF, Gade J et al (2000) Insulin signaling and insulin sensitivity after exercise in human skeletal muscle. Diabetes 49:325–331
Stump CS, Short KR, Bigelow ML, Schimke JM, Nair KS (2003) Effect of insulin on human skeletal muscle mitochondrial ATP production, protein synthesis, and mRNA transcripts. Proc Natl Acad Sci USA 100:7996–8001
Acknowledgements
H. Pedersen, A. Mengel, L. Hansen and C. B. Olsen are thanked for skilled technical assistance. This study was supported by grants from the Danish Diabetes Association, the Novo Nordisk Foundation, the Institute of Clinical Research, University of Southern Denmark and The Danish Medical Research Council.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Højlund, K., Frystyk, J., Levin, K. et al. Reduced plasma adiponectin concentrations may contribute to impaired insulin activation of glycogen synthase in skeletal muscle of patients with type 2 diabetes. Diabetologia 49, 1283–1291 (2006). https://doi.org/10.1007/s00125-006-0240-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-006-0240-5