Abstract
Aims/hypothesis
We examined to what extent visual acuity and perimetric sensitivity as measures of central and paracentral visual function would be useful for evaluating the presence and severity of diabetic macular oedema.
Materials and methods
We evaluated 59 eyes of 59 diabetic patients by identifying the presence (n=20) or absence (n=39) of macular oedema on stereo fundus photographs. The area of oedema and its distance to the centre of the macula were measured. Ischaemic macular damage was quantified by measuring the foveal avascular zone and adjacent perifoveolar intercapillary areas on fluorescein angiograms. Visual function was assessed by visual acuity charts and by short-wavelength perimetry and standard white-on-white perimetry of the central 10° field.
Results
Visual acuity did not differ between eyes with and without macular oedema. In eyes with oedema, visual acuity was correlated to the distance of the oedema from the centre of the macula (log of minimum angle of resolution {LogMar} score decreased by 0.15/mm; p=0.006) and to the thickness of the retina when the centre was affected (LogMar score decreased by 0.003/μm of thickness; p=0.0002). Multivariate analyses confirmed the results (R 2=0.46 and 0.77, respectively). Short-wavelength perimetry sensitivity was more depressed in eyes with oedema (p=0.033) but was not significantly associated with the presence of oedema after correction for macular ischaemic damage. There was no correlation between these field defects and the severity of oedema.
Conclusions/interpretation
Visual acuity was a useful measure of visual function in diabetic macular oedema involving the centre. Visual field defects were more common in eyes with macular oedema but reflected ischaemic damage of the macula rather than macular oedema itself.
Similar content being viewed by others
Introduction
Vascular abnormalities and increased vascular permeability resulting in macular oedema are a common cause of visual loss in patients with diabetic retinopathy [1]. Laser treatment can considerably reduce visual acuity loss, provided it is instituted in a timely way [2]. Diabetes is a common disease, and hence most patients who are examined for diabetic retinopathy are not seen by retinal specialists but by comprehensive ophthalmologists or general practitioners. The diagnosis of macular oedema is dependent on the subjective interpretation of morphological changes seen on fundus photographs, during ophthalmoscopy or slit-lamp biomicroscopy. This is a difficult but important evaluation, which is easier for retinal specialists than for other clinicians.
Visual acuity loss due to diabetic macular oedema is well known and tends to alert the clinician to the possibility of macular oedema, but at this stage the centre of the macula is usually already involved and the outcome of laser treatment less successful. Visual function tests that could identify macular oedema before visual acuity is affected would be of great value. One possible approach would be to identify decreased sensitivity in paracentral areas using perimetry. Like visual acuity testing, perimetry is readily available and used by all ophthalmologists.
The aim of the present study was therefore to test the hypothesis that not only visual acuity, but also perimetric sensitivity as a measure of paracentral visual function could be useful in the evaluation of the presence and severity of diabetic macular oedema. To exclude the possibility that visual function was affected by factors other than oedema, e.g. by occluded vessels in the centre of the macula, our analyses also considered the area of the foveolar avascular zone (FAZ) and adjacent perifoveolar capillary network areas (PIAs), and we also evaluated eyes without oedema.
Subjects and methods
Subjects
Our study included 59 out of 63 diabetic patients with various degrees of diabetic retinopathy, who were invited to participate and who completed all tests. Inclusion criteria were: age less than 70 years; no ocular disease, other than diabetic retinopathy, that could affect visual function; and no previous laser treatment of the examined eye. One eye of each patient was included. If both eyes were eligible, the eye with best visual acuity was selected.
Data on age at diagnosis and on duration of diabetes, as well as on treatment for diabetes and hypertension were collected. Blood pressure was measured in the supine position after 5 min of rest using a mercury sphygmomanometer. Diastolic blood pressure was taken as Korotkoff phase V. Patients on insulin treatment who were less than 30 years old at diabetes diagnosis were classified as type 1 diabetic, others as type 2 diabetic patients.
The research followed the tenets of the Declaration of Helsinki; informed consent was obtained from all subjects, and the study was approved by the Ethics Committee of Lund/Malmö.
Definition of macular oedema
The definition of macular oedema was based on stereo fundus photographs. Any abnormal thickness of the retina within the vascular arcades observed by the examiner was considered to be macular oedema [3]. Severity of oedema was expressed as the area of extension, distance to the centre of the macula, and retinal thickness.
Characterisation of vascular changes and cataract
Fundus photography
After dilatation of the pupil, stereo fundus photographs of one 35° standard field centred on the fovea were taken using a Topcon TRC 50 IX retinal camera (Topcon Corporation, Tokyo, Japan) and colour slide film (Kodachrome 64). The location and extent of the oedema on the colour slides were estimated and marked on a digital image in one 35° field centred on the fovea and processed in the Topcon Image Net 2000 system (Topcon Corporation). The estimated area and the distance between its central margin and the fovea were calculated using the Topcon Image Net 2.55 system software (Topcon Corporation). The location and extent of oedema on stereo photographs were compared with areas of abnormal retinal thickness on optical coherence tomography (OCT) maps. Diagnosis of macular oedema and OCT measurements were performed in a masked fashion.
Optical coherence tomography
Retinal thickness was measured with OCT (OCT II, version A 6.1; Carl Zeiss Meditec, Dublin, CA, USA) after pupil dilatation. Optical coherence tomography is a technique for high-resolution non-invasive imaging of the human retina and is considered a valuable and reliable tool for monitoring retinal thickness. Six 5-mm OCT scans were obtained in a 30° radial spoke pattern with the fovea as the centre, using an internal fixation light. The retinal mapping program of the A 6.1 software was used to calculate the average retinal elevation in nine zones of the central retina, as measured by the six radial scans trough the macula (Fig. 1) [4]. The reliability of the OCT measurements was estimated as the coefficient of variation of retinal elevation measured in the fovea at the mid-point in each of the six scans, as a measure of fixation control. The limit for acceptable reliability was set as a coefficient of variation ≤10%.
a Radial spoke pattern of the six OCT scans with fovea in the centre. b Normal limits (μm) for retinal elevation in each of the nine OCT zones; nasal sectors to the right and temporal ones to the left. Measurement values that exceeded the normal limits indicated significantly increased retinal elevation
To define significant abnormal retinal thickness, normal data were collected among healthy volunteers with an age profile similar to that of the patients included in our study. One eye of each of 30 subjects between 25 and 67 years of age, median 47 years, with no history of retinal disease and normal retinal appearance on fundus examination, were included in the normal database. The distributions of retinal thickness were bell-shaped and symmetrical about their means. For each of the nine sectors we calculated normal values and the 99th percentiles assuming Gaussian distribution. Eyes with abnormal retinal thickness were defined as eyes with at least one sector with a value exceeding the 99th percentile normal limit.
Fluorescein angiography
Fluorescein (25%) angiography was performed after dilatation of the pupil. Digital images were taken using a Topcon TRC 50 IX retinal camera in one 35° field centred on the fovea and processed in the Topcon Image Net 2000 system. The borders of the FAZ and each of the PIAs adjacent to FAZ [5] were marked (Fig. 2) and the areas were calculated using the Topcon Image Net 2.55 software. Only high-quality angiograms were accepted and the outlining procedure was performed on very early angiograms before any obscuring leakage had occurred in eyes with macular oedema. Outlining and measurements were performed in a masked fashion.
Cataract
The presence of cataract was registered using a slit-lamp microscope and the degree was estimated using the Lens Opacities Classification System II (LOCS II) [6]; the lowest score was 0 and the highest 4.
Characterisation of visual function
Visual acuity
Best corrected visual acuity was evaluated by counting log of minimum angle of resolution (LogMar) scores, i.e. a threshold estimate using Early Treatment Diabetic Retinopathy Study charts [7].
Visual field tests
All patients underwent visual field testing with standard 10-2 short-wavelength perimetry (SWAP) and 10-2 white-on-white perimetry (WWP) programmes of the Humphrey 750 Field Analyzer (Carl Zeiss Meditec) at two separate visits. The field tests performed at the first visit were considered training fields and were excluded from analyses. Fields were evaluated in terms of the pattern deviation probability maps included in the Statpac interpretation tool [8]. Since no Statpac interpretation was available for SWAP 10-2, a normal database including 180 eyes of 90 healthy subjects was constructed for the generation of a Statpac program including pattern deviation probability maps [9]. In these maps, test point locations with significantly reduced differential light sensitivity are flagged as abnormal after elimination of effects of media opacities, such as cataract. An increased number of test point locations with decreased sensitivity or clusters of such points indicates pathology.
Glycaemic control
Glycaemic control was assessed using glycated haemoglobin (HbA1c), analysed with HPLC (Varian II Hemoglobin A1c program; BioRad); the reference range was 3.6–5.0% for healthy individuals ≤50 years old and 4.0–5.3% for those >50 years old.
Statistical methods
Continuous descriptive variables were compared using Student’s t-test and proportions were compared applying binomial distributions, assuming Gaussian distributions. Visual acuity and damage of visual fields in terms of the number of test locations with significantly depressed differential light sensitivity at the p<1% level were compared between eyes with and without macular oedema using the Mann–Whitney U-test. In univariate analyses, the extent of oedema and its distance from the centre of the macula, the size of the FAZ and PIAs, cataract, refraction, patient age, and HbA1c were correlated to visual acuity and perimetry. Associations yielding significance or borderline significance (p<0.2) were correlated to the two measures of visual function using multivariate analyses. Statview 5.01 (SAS, Cary, NC, USA) was used for all statistical analyses. A p-value less than 0.05 was considered significant.
Results
Patient characteristics
Twenty-three patients had type 1 and 36 had type 2 diabetes. Mean age at the time of this study was 50.6 years; the youngest patient was 20 and the oldest 69 years of age. Mean age at diagnosis was 35 (2–62) (minimum–maximum) years and the known duration of diabetes 15.8 (0–57) years. HbA1c was 7.6±1.4% (mean ± SD) and systolic/diastolic blood pressure was 134±22/78±11 mmHg. Thirty-four patients were on antihypertensive medication.
Patient characteristics did not differ between those with and without oedema (Table 1).
Quantification of macula oedema, thickness of the retina and FAZ and PIAs
Twenty of the 59 eyes included in the study had macular oedema on 35° stereo photographic colour slides. Extension of oedema was 1.6 mm2 (median), ranging from 0.2 to 28.7 mm2 and the distance from the central margin to the centre of the macula was 0.4 (0–2.4) mm. Retinal thickness on OCT was 281 (239–445) μm.
Forty-six of the 59 subjects had high-quality angiograms enabling accurate outlining and quantification of FAZ and PIAs. The concordance between two independent outlining procedures measuring FAZ was high, with a correlation coefficient of 0.99. The total area of FAZ and PIAs in these 46 eyes was 0.59 (0.22–3.93) mm2.
Co-localisation of macular oedema on stereo fundus photographs and abnormal retinal thickness on OCT
The location and extent of areas of macular oedema detected on stereo fundus photographs agreed well with the thickened zones identified on the OCT maps. In 15 of the 20 eyes, the overlapping was complete, but in five eyes oedema was observed on stereo photographs only. In three of the latter five eyes, the oedema was localised at the peripheral margin of the OCT detection area, and in two the oedematous area was small (≤0.3 mm2) and localised between two radial OCT scans. OCT identified thickened zones in 18 eyes without any detectable macular oedema on stereo photographs. In all but one of these eyes, the thickness was just slightly above the upper normal limit. The median of the intra-individual coefficient of variation of the centre of the six OCT scans was 7%, ranging from 3 to 10%.
Cataract
The highest LOCS II grading was 1 for nuclear cataract (n=16), 2 for cortical (n=2) and 2 for posterior subcapsular cataract (n=1).
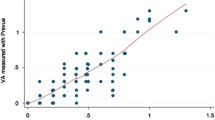
Visual acuity
Median visual acuity LogMar score was −0.04 and the range was from −0.22 to 0.82. Visual acuity was not significantly worse in the 20 eyes with macular oedema (median LogMar score −0.05) on stereoscopic colour slides than in eyes without oedema (−0.04) (p=0.90). In the univariate analysis, visual acuity was significantly associated with the distance from the centre of the macula to the central margin of the oedema (Table 2), i.e. oedema closer to the centre was associated with worse visual acuity (p=0.006). There was also an association between visual acuity and abnormal retinal thickness on OCT, both in the central macular thickness (p=0.0002) and when taking the thickness of all zones into consideration (p=0.0002) (Table 3), but visual acuity was not influenced by the size of FAZ and PIAs. The explaining variables for visual acuity, established in the multivariate analyses, were the distance of oedema from the centre of the macula and HbA1c (R 2=0.46) (Table 4), thickness in the centre, and mean thickness of all zones on OCT (R 2=0.77) (Table 5).
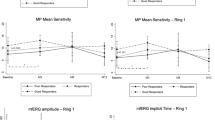
Visual fields
SWAP fields in eyes with macular oedema showed a higher number of locations with depressed differential light sensitivity (median 10.8) than in eyes without oedema (median 5.2) (p=0.033) but there was a considerable overlap between eyes with and without oedema (Fig. 3). A corresponding analysis for WWP yielded no significant difference between eyes with and without oedema; the median numbers of locations were 5.0 and 3.4, respectively (p=0.104). In the univariate analyses, SWAP and WWP results were associated only with the area of FAZ and PIAs (p=0.02 and p=0.03, respectively) (Tables 2 and 3). The explaining variables for SWAP and WWP defects, established in the multivariate analyses, were the respective sizes of FAZ and PIAs (R 2=0.24 and 0.28, respectively) (Tables 4 and 5). There was no correlation between SWAP or WWP defects and severity of macular oedema expressed as area of oedema, abnormal thickness and distance to the centre of the macula (Tables 2 and 3).
Discussion
In this study, we have confirmed that visual acuity correlates well with the distance of macular oedema to the centre of the macula. In addition, we have demonstrated that visual acuity correlates to retinal thickness in the macula when the centre is involved. The results indicate that visual acuity is not impaired until the centre of the macula is already involved. There were more locations with depressed differential light sensitivity on SWAP in eyes with than without oedema but with a considerable overlap between groups, and when considering also other aspects of diabetic retinopathy, such as the occlusion of perifoveolar capillary network, oedema no longer influenced the results. The results indicate that the visual field defects reflected ischaemic damage of the macula rather than macular oedema per se.
A study comparable with ours on perimetric sensitivity and diabetic macular oedema has been performed by Hudson et al. [10]. We used the same visual field testing and we interpreted the same parameters in the perimetric results, e.g. pattern deviation. In the Hudson study, SWAP localised field loss corresponding to the clinical mapping of the area of clinically significant macular oedema, as defined by the Early Treatment Diabetic Retinopathy study [11], and it was concluded that SWAP offers improved sensitivity for the psychophysical detection of clinically significant macular oedema. However, Hudson and colleagues did not include eyes without oedema in their analyses and also did not characterise the perifoveolar capillary network. Although it cannot be excluded that the difference in results could depend on our use of a different classification of macular oedema, our multivariate analysis showed that FAZ and PIAs together was the only explanatory variable not only for SWAP but also for WWP defects, as previously described in more detail [9]. Similar observations on SWAP have been published by Remky et al. [12]. Taken together, our results suggest that SWAP may help to predict early ischaemic damage to the macula and indicate that SWAP may be of limited usefulness for clinicians in their efforts to evaluate sight-threatening macular oedema.
We used the international definition of macular oedema proposed by the Global Diabetic Retinopathy Project Group [3], based on the presence or absence of oedema within the vascular arcades and designed to facilitate the communication between physicians who care for people with diabetes. The diagnosis and quantification of macula oedema was thorough. Diagnosis was obtained from stereo photographs of the macula, which is considered as standard [11]. The detection was dependent on the clinical examiner or reader of the photographs and so was the estimation of the extent of oedema and the distance to the centre of the macula. To that end, the location of oedema was verified by OCT, which provides objective, high-resolution, non-invasive imaging of the human retina and is considered a valuable and reliable tool for monitoring retinal thickness [4, 13–17]. Thus, macular oedema was assessed and quantified on stereo fundus photographs in terms of the extent and location of oedema in relation to the centre of the macula. In addition, the location of oedema was verified by OCT and quantified in terms of retinal thickness.
There was good agreement between the location of abnormal thickness of the retina on stereo photographs and OCT. In some eyes, however, abnormal thickness of the retina was observed on fundus photographs only. Similar results have been reported by Ström et al. [18], and it is likely that for some subtle lesions and for those at the margin of the OCT detection area stereo photography is more sensitive than OCT. On the other hand, OCT recognised marginally abnormal thickness without detectable macular oedema in 18 eyes. Since the thickness was modest and just slightly above the upper reference limit, it may well be that the normal upper limit for abnormal retinal thickness in our reference subjects was somewhat narrow. However, when using thickness on OCT as the standard for oedema instead of detection of oedema on stereo photographs in the present study, neither the results nor the conclusions changed.
The presence of cataract did not influence our results. The frequency of cataract was low, the degrees were mild, and in the visual field analysis we used pattern deviation maps designed to reduce the effects of cataract. It could also be argued that SWAP defects reflect impaired colour vision, but the similar correlations between FAZ, PIAs and WWP make this less likely.
In summary, measuring visual function in patients with diabetic macular oedema may add some useful information to the interpretation of retinal morphology. Visual acuity is a good measure but it is usually not reduced until the centre is involved. Visual fields are affected before visual acuity loss but the sensitivity and specificity of perimetry are rather low because of overlap between eyes with and without oedema, and the visual field defects seem to reflect ischaemic macular damage rather than oedema itself. Taken together, our results indicate that, if patients with diabetic macular oedema are to be referred to retinal specialists before visual acuity is affected, evaluation of morphological findings on fundus photographs or at retinal examination remains the most important diagnostic procedure. However, for those who find interpretation of retinal findings difficult, visual functional testing could help identify patients who need to see a retinal specialist.
Abbreviations
- FAZ:
-
Foveal avascular zone
- LOCS:
-
Lens Opacities Classification System
- LogMar:
-
Log of minimum angle of resolution
- OCT:
-
Optical coherence tomography
- PIAs:
-
Perifoveolar intercapillary areas
- SWAP:
-
Short-wavelength automated perimetry
- WWP:
-
White-on-white perimetry
References
Klein R, Klein BE, Moss SE, Cruickshanks KJ (1995) The Wisconsin Epidemiologic Study of Diabetic Retinopathy XV. The long-term incidence of macular edema. Ophthalmology 102:7–16
Early Treatment Diabetic Retinopathy Study Research Group (1987) Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema. Early Treatment Diabetic Retinopathy Study Report Number 2. Ophthalmology 94:761–774
Wilkinson CP, Ferris FL 3rd, Klein RE, Lee PP, Agardh CD, Davis M et al (2003) Proposed international clinical diabetic retinopathy and diabetic macular edema severity scales. Ophthalmology 110:1677–1682
Hee MR, Puliafito CA, Duker JS et al (1998) Topography of diabetic macular with optical coherence tomography. Ophthalmology 105:360–370
Sleightholm MA, Arnold J, Kohner EM (1988) Diabetic retinopathy: I. The measurement of intercapillary area in normal retinal angiograms. J Diabet Complications 2:113–116
Chylack LT, Leske MC, McCarthy D, Khu P, Kashiwagi T, Sperduto R (1989) Lens Opacities Classification System II (LOCS II). Arch Ophthalmol 107:991–997
Ferris FL 3rd, Kassoff A, Bresnick GH, Bailey I (1982) New visual acuity charts for clinical research. Am J Ophthalmol 94:91–96
Heijl A, Lindgren G, Olsson J, Åsman Å (1989) Visual field interpretation with empiric probability maps. Arch Ophthalmol 107:204–208
Bengtsson B, Heijl A, Agardh E (2005) Visual fields correlate better than visual acuity to severity of diabetic retinopathy. Diabetologia DOI: 10.1007/s00125-005-0001-x
Hudson C, Flanagan JG, Turner GS, Chen HC, Young LB, McLeod D (1998) Short-wavelength sensitive visual field loss in patients with clinically significant diabetic macular oedema. Diabetologia 41:918–928
Early Treatment Diabetic Retinopathy Study research group (1985) Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Early Treatment Diabetic Retinopathy Study research group. Arch Ophthalmol 103:1796–1806
Remky A, Arend O, Hendricks S (2000) Short-wavelength automated perimetry and capillary density in early diabetic maculopathy. Invest Ophthalmol Vis Sci 41:274–281
Rivellese M, George A, Sulkes D, Reichel E, Puliafito C (2000) Optical coherence tomography after laser photocoagulation for clinically significant macular edema. Ophthalmic Surg Lasers 31:192–197
Massin P, Vicaut E, Haouchine B, Erginay A, Paques M, Gaudric A (2001) Reproducibility of retinal mapping using optical coherence tomography. Arch Ophthalmol 119:1135–1142
Muscat S, Parks S, Kemp E, Keating D (2002) Repeatability and reproducibility of macular thickness measurements with the Humphrey OCT system. Invest Ophthalmol Vis Sci 43:490–495
Sanchez-Tocino H, Alvarez-Vidal A, Maldonado MJ, Moreno-Montanes J, Garcia-Layana A (2002) Retinal thickness study with optical coherence tomography in patients with diabetes. Invest Ophthalmol Vis Sci 43:1588–1594
Goebel W, Kretzchmar-Gross T (2002) Retinal thickness in diabetic retinopathy: a study using optical coherence tomography (OCT). Retina 22:759–767
Ström C, Sander B, Larsen N, Larsen M, Lund-Andersen H (2002) Diabetic macular edema assessed with optical coherence tomography and stereo fundus photography. Invest Ophthalmol Vis Sci 43:241–245
Acknowledgements
This study was supported by the Medical Faculty of Lund University, the Foundation for Visually Impaired in Former Malmöhus län, the Järnhardt Foundation, the Stoltz’ Foundation, the Malmö University Hospital Foundation, and the Skane County Council Foundation for Research and Development.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Agardh, E., Stjernquist, H., Heijl, A. et al. Visual acuity and perimetry as measures of visual function in diabetic macular oedema. Diabetologia 49, 200–206 (2006). https://doi.org/10.1007/s00125-005-0072-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-005-0072-8